Syllabus (Fourth Edition, 2023)
Topics
U1: Endocrine Physiology
i. Describe the exocrine and endocrine functions of the pancreas.
ii. Describe the physiology of insulin, glucagon, and somatostatin.
iii. Describe the control of blood glucose.
iv. Describe the control, secretions and functions of the pituitary and the hypothalamus.
v. Describe the control, secretions, and functions of the thyroid.
vi. Describe the control, secretions, and functions of renal and adrenal hormones.
vii. Describe the control of plasma calcium.
U2: Endocrine Pharmacology
i. Understand the pharmacology of glucocorticoids.
ii. Understand the pharmacology of insulin preparations.
iii. Understand the pharmacology of oral hypoglycaemic drugs.
iv. Understand the pharmacology of thyroid hormones.
v. Understand the pharmacology of mineralocorticoids.
vi. Outline the pharmacology of glucagon.
vii. Understand the pharmacology of vasopressin and its analogues.
Topics not covered in previous SAQs
U2: Endocrine Pharmacology
iv. Understand the pharmacology of thyroid hormones.
v. Understand the pharmacology of mineralocorticoids.
vi. Outline the pharmacology of glucagon.
Learning Objectives for the First Part Examination in Intensive Care Medicine
- This will ensure that trainees, tutors, and examiners can work from a common base.
- All examination questions are based around this Syllabus.
- These learning objectives are designed to outline the minimum level of understanding required for each topic.
- The accompanying texts are recommended on the basis that the material contained within them provides sufficient information for trainees to meet the learning objectives.
- Trainees are strongly encouraged to explore the existing and evolving body of knowledge of the Basic Sciences as they apply to Intensive Care Medicine by reading widely.
- For all sections of the syllabus an understanding of normal physiology and physiology at extremes of age, obesity, pregnancy (including foetal) and disease (particularly critical illness) is expected.
- Similarly, for pharmacology, trainees are expected to understand a drug’s pharmacology in these contexts.
- An understanding of potential toxicity and relevant antidotes is also expected.
Definitions
Throughout the document specific wording has been used under the required abilities to indicate the level of knowledge and understanding expected and a glossary of these terms is provided.
Definitions
| Calculate | Work out or estimate using mathematical principles. |
| Classify | Divide into categories; organise, arrange. |
| Compare and contrast | Examine similarities and differences. |
| Define | Give the precise meaning. |
| Describe | Give a detailed account of. |
| Explain | Make plain. |
| Interpret | Explain the meaning or significance. |
| Outline | Provide a summary of the important points. |
| Relate | Show a connection between. |
| Understand | Appreciate the details of; comprehend. |
SAQs
U1. Endocrine Physiology
i. Describe the exocrine and endocrine functions of the pancreas.
2019B 13
Describe the exocrine functions of the pancreas.
CICMWrecks Answer
Exocrine pancreas
- produces 1.5L/day pancreatic juice
- Pancreatic juice – digestive enzymes and bicarbonate
- Enzymes: synthesized and secreted from the exocrine acinar cells
- Bicarbonate: secreted from epithelial cells lining small pancreatic ducts
Contents
- Digestive Enzymes:
- Proteases: trypsin and chymotrypsin: proteolysis
- Pancreatic Lipase: Hydrolysis of triglycerides
- Amylase: Hydrolysis of carbohydrates
- Other Pancreatic Enzymes: Ribonuclease, deoxyribonuclease, gelatinase and elastase
- Bicarbonate and water:
- Bicarbonate neutralizes acid coming into small intestine from stomach
- Produced by carbonic anhydrase → secreted into the lumen of the duct → pancreatic juice
Control of pancreatic exocrine secretions
- Vagus nerve:
- Low level stimulus via Ach in response to anticipation of meal
- Enteric endocrine system:
- Cholecystokinin:
- secreted in duodenum
- Stimulated by partially digested proteins and fats
- CCK released into blood → binds to pancr acinar cells
- secreted in duodenum
- Secretin:
- Secreted in proximal small intestine
- In response to acid in duodenum
- Stimulates duct cells to secrete water and bicarb
- Secreted in proximal small intestine
- Gastrin:
- Secreted by stomach
- in response to gastric distension and irritation
- Stimulates acinar cells to secrete digestive enzymes
- Secreted by stomach
- Cholecystokinin:
Occurs in three phases: cephalic → Gastric → Intestinal
JC 2019
Examiner Comments
2019B 13: 33% of candidates passed this question.
Most candidates were able to mention some pancreatic enzymes, though often in insufficient detail to attract full marks. The amount, type, pH, etc. of pancreatic secretions was often not included. Many candidates did not describe the stimuli for pancreatic secretion. Better answers described the cephalic, gastric and intestinal phases of pancreatic secretion.
2023A 06
Describe pancreatic secretions and their regulation.
CICMWrecks Answer
Pancreatic Secretions
| EXOCRINE SECRETIONS | HCO3– | |
| Water | ||
| Enzymes | Proteases | |
| Amylase | ||
| Lipase | ||
| Others | ||
| ENDOCRINE SECRETIONS | Insulin | |
| Glucagon | ||
| Somatostatin | ||
Pancreas: Exocrine Secretions
Contents
- Digestive Enzymes:
- Proteases: trypsin and chymotrypsin: proteolysis
- Pancreatic Lipase: Hydrolysis of triglycerides
- Amylase: Hydrolysis of carbohydrates
- Other Pancreatic Enzymes: Ribonuclease, deoxyribonuclease, gelatinase and elastase
- Bicarbonate and water:
- Bicarbonate neutralizes acid coming into small intestine from stomach
- Produced by carbonic anhydrase → secreted into the lumen of the duct → pancreatic juice
Control of pancreatic exocrine secretions
- Vagus nerve:
- Low level stimulus via Ach in response to anticipation of meal
- Enteric endocrine system:
- Cholecystokinin:
- secreted in duodenum
- Stimulated by partially digested proteins and fats
- CCK released into blood → binds to pancr acinar cells
- secreted in duodenum
- Secretin:
- Secreted in proximal small intestine
- In response to acid in duodenum
- Stimulates duct cells to secrete water and bicarb
- Secreted in proximal small intestine
- Gastrin:
- Secreted by stomach
- in response to gastric distension and irritation
- Stimulates acinar cells to secrete digestive enzymes
- Secreted by stomach
- Cholecystokinin:
Occurs in three phases: cephalic → Gastric → Intestinal
Pancreas: Endocrine Secretions
Insulin
- Peptide hormone produced in beta cells of Islets of Langerhans in pancreas
- Proinsulin: insulin precursor; A + B chain joined by 2 disulphide bridges + C peptide
- Insulin: formed when C peptide is cleaved by endopeptidases → insulin + free C peptide are packaged in vesicles
- Exocytosis:
- Primary trigger = ↑BSL
o ↑BSL → ↑facilitated diffusion of glucose through GLUT2 transmembrane channels into B-islet cells → ↑metabolic activity of cell → ↑formation of ATP - ATP-gated K channels on beta islet cell membrane are closed by ↑ATP levels → ↓ K flux → membrane depolarisation → triggers opening of voltage gated Ca2+ channels → Ca2+ influx triggers insulin containing vesicle exocytosis
- Primary trigger = ↑BSL
- Plasma insulin secretion occurs in 2 phases
- ↑BSL → rapid ↑insulin concentration as vesicles with pre-formed insulin empty contents
- When all vesicles have emptied → B islet cells release insulin as it is synthesised
- Physiological effects:
- Facilitation of glucose uptake: GLUT4 in adipose tissue, skeletal muscle, heart – require insulin to facilitate cellular glucose uptake. NB brain has GLUT-1 and liver has GLUT-2 which are not insulin dependent
- Storage of metabolic substrates: hepatic glycogenesis, FA synthesis in liver, ↑esterification of FAs (to make TGs) in adipose tissue
- Inhibition of endogenous glucose production: insulin inhibits lipolysis + glycogenolysis + gluconeogenesis
- Cellular uptake of amino acids and K
- ↑amino acid uptake → promotes protein synthesis
- ↑K uptake: prevents hyperkalaemia following meal
Glucagon
- peptide hormone produced by alpha cells of islets of Langerhans
- unlike insulin, the have no glucose sensing apparatus
- Secretion:
- stimulated by hypoglycaemia: hypoglycaemia-induced ↑ANS activity (i.e. indirect) + ↑adrenaline
- inhibited by: insulin, somatostatin, ↑freeFA and ketone body concentrations
- Actions: ↑plasma glucose conc by: promoting gluconeogenesis+glycogenolysis, inhibits glycolysis in liver. Important during starvation
Somatostatin
- secreted by delta cells in pancreatic islets (and pyloric antrum, duodenum)
- inhibitory hormone
- Stimuli for release: (i) ↑ plasma levels of glucose, a.a. and FA, and (ii) Acidic gastric environment
- inhibited by vagus nerve
- Effects:
- ↓ secretion of pancreatic hormones (insulin, glucagon, pancreatic polypeptide)
- ↓ GH release from pituitary
- ↓ gastric, duodenal and GB motility
- ↓ secretion and absorption in GIT (Eg. gastric acid secretion)
Pancreatic polypeptide
- Polypeptide secreted by F-cells of Islets of Langerhans
- influence GIT function (Ie. ↑enzyme secretion, ↓ intestinal motility, Etc.)
Examiner Comments
2023A 06: 21% of candidates passed this question.
It was vital to recognise and describe both the exocrine and endocrine secretions of the pancreas and their regulation. Insulin, glucagon, and somatostatin are all secreted from the pancreas and their omission was the most common reason for not passing this question. Many candidates unfortunately wrote solely on exocrine secretions. Satisfactory answers provided a moderate amount of detail on both the endocrine (insulin, glucagon and somatostatin) and exocrine (bicarbonate and digestive enzymes; trypsin/chymotrypsin, pancreatic amylase and lipase) secretions of the pancreas including what determines their secretion.
2015A 06
Outline the physiology of pancreatic secretion (80% of marks)
and outline the pharmacology of octreotide (20% of marks)
CICMWrecks Answer: Pancreas Secretions
Pancreatic Secretion
| EXOCRINE SECRETIONS | HCO3– | |
| Water | ||
| Enzymes | Proteases | |
| Amylase | ||
| Lipase | ||
| Others | ||
| ENDOCRINE SECRETIONS | Insulin | |
| Glucagon | ||
| Somatostatin | ||
Exocrine Secretions
- produced by acinar and ductal cells
- ~1.5L per day
- HCO3–
- alkalinize gastric contents
- enzyme carbonic anhydrase
- Water
- Enzymes
- Proteases: Trypsinogen → Trypsin (by enterokinase in gut), Chymotrypsinogen → Chymotrypsin. Proteolysis.
- Amylase: Hydrolysis of glycogen, starch, and complex carbohydrate.
- Lipase: Hydrolysis of dietary triglycerides.
- Others: ribonuclease, deoxyribonuclease, gelatinase and elastase
Endocrine Secretions
- Insulin
- polypeptide hormone
- synthesized from proinsulin in RER of B cells in Islets of Langerhans
- Excreted via exocytosis in response to ↑intracellulae Ca2+
- Minimal protein binding, tiny Vd 0.075 L/kg
- Metabolized in liver, muscle, kidney byt Glutathione insulin transhydrogenase
- Renal elimination of inactive metabolites
- Circulatory hald life ~5mins
- Increased anabolism, decreased catabolism
- maintains normal blood glucose levels by facilitating cellular glucose uptake, regulating carbohydrate, lipid and protein metabolism
- promotes cell division and growth through its mitogenic effects
- Glucagon
- polypeptide hormone
- synthesized in pancreatic A cells
- secreted into portal vein
- Circulating half life ~5mins
- Metabolized in liver (1st pass) – low circulating level
- Glycogenolysis, gluconeogenesis, glucose release, ketone formation
- Lipolysis
- Inotopy, increases metabolic rate
- Stimulates somatostatin, insulin release
- Somatostatin
- polypeptide hormone
- Inhibits Glucagon, Insulin, other pancreatic peptides
- may function as CNS neurotransmitter
CICMWrecks Answer: Pharmacology of Octreotide
Pharmacology of Octreotide
Examiner Comments
2015A 06: 38 % of candidates passed this question.
An outline of exocrine function should have included the sources of secretions, secretions involved in the digestion of proteins, carbohydrates and fats, the roles of trypsin inhibitors and bicarbonate secretion and the regulation of enzyme and bicarbonate secretion.” Knowledge of endocrine physiology was good whereas the depth of knowledge regarding exocrine function was generally shallow with many errors.
Only some general facts around the pharmacology of octreotide were required to pass this section of the question. Responses revealed limited knowledge and contained many errors.
ii. Describe the physiology of insulin, glucagon, and somatostatin.
2010B 08
Outline the physiological consequences of an inability to produce insulin.
CICMWrecks Answer
Insulin
Insulin is a 51 amino acid hormone (MW 5734 D) consisting of two chains (α and β) made in the pancreatic beta cells as a folded protein. It is released in response to blood glucose levels > 5mmol/L.
Actions:
Acts by binding to the insulin receptors (α and β subunits) on the surface of target cells, causing a shape change which results in the phosphorylation of several proteins within the cell, which modulate the activity of several processes. Insulin is anabolic, increasing the storage of glucose, fatty acids, and amino acids.
Roles:
CHO:
- Stimulates GLUT 4 receptors to move to the surface of muscle and adipose tissue cells to increase glucose uptake (this does not happen in RBC, brain tissue, intestinal mucosal cells or renal tubule cells).
- Upregulates Glycogen Synthase to increase glycogen production
- Upregulates glucokinase in hepatocytes to trap glucose in cells by phosphorylating it
- Decreases gluconeogenesis and glycogenolysis (by inhibiting glucose-6-phosphatase)
Proteins:
- Upregulates amino acid uptake, enhances protein synthesis, and inhibits protein degradation in muscle and other tissues, thereby decreasing the plasma concentrations of most amino acids
Lipids:
- Upregulates Pyruvate Dehydrogenase, Lipoprotein Lipase and Fatty Acid Synthase to facilitate the breakdown of TAGs to fatty acids for uptake by adipose tissue cells
- Inhibits Hormone Sensitive lipase to decrease the hydrolysis of triglycerides stored in the adipocyte
Inability to produce insulin will therefore result in:
- Hyperglycaemia (but relative intracellular hypoglycaemia, as glucose is unable to enter cells)
- Loss of inhibition of gluconeogenesis from proteins and adipose tissue
- Reduction in protein synthesis and TAG synthesis
- Utilisation of fatty acids as an alternative fuel source à
- Adipose tissue is broken down to FFA via Hormone Sensitive lipase (which is no longer inhibited by insulin), and Acetyl CoA produced from the FFA.
- Acetyl CoA can enter the Krebs cycle or be transported to the liver for ketone body production via beta oxidation (acetoacetate, beta-hydroxybutyrate and acetone)
- Ketone bodies are distributed to the tissues, converted back to Acetyl CoA and used as fuel
- The presence of high levels of ketone bodies results in a metabolic acidosis à produces ‘air hunger’ and Kussmaul breathing in an attempt to compensate for this acidosis
- Acidosis produces hyperkalaemia (the lack of insulin-induced K entry to cells also contributes)
- Increase in plasma free fatty acids and amino acids
- Hyperglycaemia exceeds the renal tract’s ability to reabsorb glucose and a glycosuria occurs along with an osmotic diuresis of the large, osmotically active glucose molecule
- Patient becomes hypovolaemic and hyponatremic due to loss of Na through the renal tract
Examiner Comments
2010B 08: 7 (47%) of candidates passed this question.
Most candidates were able to detail how insulin allowed influx of glucose into insulin dependent cells, in combination with potassium. Good candidates were able to explain how the inability to produce insulin allowed hypovolaemia and electrolyte loss, with the ensuing tachycardia and hypotension. Few candidates mentioned insulin’s action on hormone sensitive lipase (HSL), and that deficiency of insulin leads to increased activity of this enzyme. The fact that when insulin is not produced, the liver cells carry out β-oxidation of the fatty acid (released peripherally by the action of HSL) releasing acetyl CoA which is coalesced into acetoacetic acid was mentioned by only a few. However, the fact that ketone bodies in the form of acetoacetic acid, β-hydroxybutyric acid and acetone accumulate and cause a metabolic (anion gap) acidaemia, appeared to be well known. Few, went on to describe that a compensatory respiratory alkalosis will be generated and detail how and why this occurred.
Syllabus: N2a&b, E2,F1, C1g 2b
References: Guyton and Hall Textbook of Medical Physiology 10th Ed, pg 888
iii. Describe the control of blood glucose.
2024A 07 – 2018B 12
Outline the control of blood glucose.
2009B 04
Describe the body’s mechanisms for regulating blood glucose.
CICMWrecks Answer
General
- Normal BSL 4-6mmol/L
- Tight BSL control important as:
- ↓ BSL: disrupt normal function of brain, retina, gonads (obligate glucose users)
- ↑ BSL: ↑ osmolality, osmotic load on kidneys → diuresis + cellular dehydration, loss of electolytes/ substrate → tissue damage
BSL control via feedback mechanism
- Sensors: pancreatic islets of Langerhans
- Central regulator: lateral (feeding) and ventromedial (satiety) centres of hypothalamus
- Effectors:
- Behavioural (feeding)
- Hormonal: insulin vs. glucoagon balance (act on liver, muscle, adipocytes)
- Renal (excretion)
- Modulated by: catecholamines, cortisol, thyroid homrones
- short term regulation: via secretion or inhibition of insulin + glucagon from pancreatic islets
- long term: neuronal mechanisms (SNS activation) + hormones (cortisol, GH)
Sensors
- Pancreatic beta cells → sense ↑ BSL
- Secrete insulin in biphasic pattern: initial rapid ↑ → prolonged slow ↑
- 1st phase of insulin secretion: ↑ BSL → glucose enters via GLUT2 → converted to pyruvate → enters TCA → generate ATP → inhibit ATP sensitive K channel → ↓ K efflux → depolarisation → open voltage gated Ca2+ channels → exocytosis of insulin granules
- 2nd phase of insulin secretion: glutamate produced as by-product of TCA → maturation of other insulin granules
- Pancreatic alpha cells → sense ↓ BSL
- ↑ glucagon release
Effectors
- insulin: secreted in response to ↑ BSL → following effects to ↓ BSL
- ↑ GLUT4 insertion into cell membrane → ↑ glucose uptake into cells esp. muscle + fat
- ↑ glycogen synthesis
- ↑ glucose utilisation + ↑ fat and protein synthesis
- ↓ glycogenolysis / ↓ gluconeogenesis
- glucagon: secreted in reponse to ↓BSL → following effects to ↑ BSL
- ↑ glycogenolysis / ↑ gluconeogenesis
- minimal effect on adipose tissue and muscle
- Adrenaline: stimulated by ↓ BSL, stress
- Inhibit insulin
- Liver: ↓ glycogenesis, ↑ glucose release, ↑ KB
- Fat: ↑ FFA release, ↓ glucose uptake
- Muscle: ↓ glucose uptake, ↑ FFA metabolism
- Sustained ↓ BSL stimulates GH + cortisol release
- ↓ glucose utilisation + ↑ fat utilisation → limiting further ↓ BSL
- ↓ protein synthesis / ↑ aa release / ↑ FFA metabolism
- Neuronal Mechanisms:
- Hypothalamus directly stimulated by hypoglycaemia → ↑ SYNS activity → adrenaline release → stimulates hepatic glucose release
Kerr 2016
Examiner Comments
2024A 07: 60% of candidates passed this question.
This question required candidates to discuss the role of the pancreas and liver in the homeostasis of blood glucose. This included how the pancreas senses high or low glucose levels, the mechanism of secretion of insulin and glucagon and subsequent effects on the liver. The response in early fasting when glucagon stores are depleted was expected as well as the role of other organs in this setting such as muscle glycogen and hypothalamus driven satiety. A brief mention other hormonal responses in the setting of hypoglycaemia was also expected (including ACTH, cortisol, adrenaline, growth hormone and thyroid hormones).
2018B 12: 53% of candidates passed this question.
A definition of normal glucose levels was expected, mentioning how it is regulated despite variable intake. Most answers incorporated the roles of insulin/glucagon and the glucostat function of the liver. Sufficient detail regarding the mechanism of insulin release was often lacking. Extra marks were awarded for description of the role of the satiety centre in the hypothalamus, glucokinase and processes in fasting and starvation that maintain blood glucose levels.
Marks were not awarded for describing effects of insulin and glucagon unrelated to glucose control.
2009B 04: 4 (44%) of candidates passed this question.
This question sought a candidate’s knowledge of the basic science underpinning a topical area of clinical Intensive Care practice. Candidates were expected to mention normal values of blood glucose and detail the relevant humoral (dominant) and neural (sympathetic) factors.
These included mention of, description of and mechanisms for the stimulation/inhibition and actions of humoral factors such as insulin, glucagon, cortisol, etc as the specifically apply to blood glucose control, neural stimulation and the liver’s role as a glucostatic organ.
Good candidates would demonstrate a structured response to their answer.
Syllabus – N12b
Reference: Textbook of Medical Physiology 11th ed Guyton and Hall, Ch. 78
2007B 16
Describe the physiological response to hypoglycaemia.
CICMWrecks Answer
BSL normally maintained 4-7mmol/L
- maintained by –ve feeback system
- detector: islets of Langerhans cells in pancreas
- stimulus= BSL
- effector = insulin:glucagon release ratio
- aim: maintain BSL to provide substrate for obligate glucose metbaolisers (brain + RBC)
- hypoglycaemia = BSL <3mmol/L
Acute hypoglycaemia
- ↓ BSL: compensatory mechanisms not yet activated (hormonal ∆s not yet occurred) → glucagon, cortisol, GH levels minimal initial change
- early sign: hunger
- later signs: neurological impairment → confusion, agitation → progression with ↓ BSL → coma, seizures, death
| BSL (mmol.L-1) | Symptoms | Endocrine Response |
| 4.6 | Insulin secretion inhibited | |
| 3.8 | Autonomic dysfunction | Glucagon, adrenaline, and GH secretion |
| 2.8 | CNS dysfunction | Cortisol secretion |
| 2.2 | Lethargy, Coma | |
| 1.7 | Convulsions | |
| 0.6 | Permanent brain damage, Death |
Physiological consequences of acute hypoglycaemia
- SNS activation → ↑ catecholamine release
- Central: nausea, agitation, hunger
- Liver: ↑ glycogenolysis, ↑ glucose release
- Pancreas: inhibition of insulin release
- CVS: ↑ HR, ↑ SVR, peripheral shutdown, sweating
- ↓ insulin release: ↑ BSL detected by β cells of islets of Langerhans
- adipose tissue:
- ↓ glucose uptake (↓GLUT4 transporters in membrane)
- ↓ fat uptake (extracellular inhibition of LPL in endothelium)
- ↑ FFA release (↑ intracelular hormone sensitive lipase)
- muscle
- ↓ glucose uptake (↓ GLUT4)
- ↓ protein synthesis
- ↓ glucogenesis
- ↑ FFA metabolism
- liver
- ↑ glucose release (glycogenolysis)
- ↑ FFA release (some ketone body formation)
- ↑ gluconeogenesis via glycerol (fats) and lactate (RBC metabolism)
- adipose tissue:
- ↑ catabolic hormones: ↓ BSL stimulates hormonal changes which aim to ↑ BSL over sustained period
- ↑ glucagon → ↑ hepatic gluconeogenesis from aa, lactate, glycerol
- cortisol, GH → ↑ FFA release from adipose tissue
Kerr 2016
Examiner Comments
2007B 16: 4 candidates (57%) passed this question.
To pass this question, the candidate only needed to stage the range of normal blood glucose, define hypoglycaemia then give an overview of the body’s response to hypoglycaemia (control of blood glucose – sensors, integrators, effectors). Additional credit was given for a more detailed description of the various responses. Few candidates mentioned the role of the sympathetic nervous system. Much time was wasted in giving detailed descriptions of metabolic pathways to the exlusion of an overview of the body’s responses.
iv. Describe the control, secretions and functions of the pituitary and the hypothalamus.
2021A 13
List the cell types in the anterior pituitary gland. Outline their secretions, control and target organ effects.
CICMWrecks Answer
Anterior Pituitary Gland
- Anterior lobe of pituitary gland (aka. adenohyophysis) → forms 80% of pituitary gland → consists of 3 parts:
- Pars tuberalis
- Parts intermedius (intermediate lobe)
- Pars distalis (anterior lobe) → produces most anterior pituitary hormones
- Derived from buccal ectoderm → it extends upwards from the epithelial lining of the primitive mouth cavity (as Rathke’s pouch), then fuses with the downward growing infundibulum of the hypothalamus (which forms the posterior pituitary)
- Consists of non-neural secretory epithelial cells connected INDIRECTLY to the hypothalamus via the “hypothalamic-hypophysial portal system”:
- Non-neural secretory epithelium:
- Granular secretory cells (chromophils)
- Acidophils (80%) → red-staining cells → synthesise and store large peptide hormones in secretory granules
- Lactotropes → PRL
- Somatoropes → GH (somatotropins)
- Basophils (20%) → blue-staining cells → synthesise and store glycoprotein hormones in secretory granules
- Gonadotropes → FSH and LH
- Thyrotropes → TSH
- Corticotropes → ACTH (and MSH)
- Acidophils (80%) → red-staining cells → synthesise and store large peptide hormones in secretory granules
- Agranular secretory cells (chromophobes)
- Weakly staining cells → inactive or degranulated secretory cells → does not synthesise any hormones
- Granular secretory cells (chromophils)
- Hypothalamic-hypophysial portal system
- Branches of superior hypophysial artery → forms “1° capillary plexus” near median eminence of hypothalamus → then forms lesser portal veins that gives rise to “2° capillary plexus” in anterior lobe of pituitary gland
- Functions of portal venous system
- Blood supply of 90% of anterior pituitary (and infundibulum)
- Pathway for hypophysiotropic hormones (from median eminence of hypothalamus) to reach the anterior pituitary gland, and
- Allows hormones secreted by anterior pituitary gland to enter systemic circulation
- Non-neural secretory epithelium:
- Blood supply → 90% supplied by hypothalamic-hypophysial portal system (from superior hypophysial artery)
Hypophysiotrophic hormones: Control of anterior pituitary gland
- Hypophysiotrophic hormones are small peptides (EXCEPT for DA) produced by cell bodies (containing “parvocellular neurons”) in the hypothalamus located near the median eminence → small amounts are secreted from the tuberoinfundibular tract into the hypothalamic-hypophysial portal system → reaches anterior pituitary where it exerts either an “excitatory” or “inhibitory” effect on non-neural secretory epithelial cells
Nb. Only trace levels of these hormones are found in systemic circulations b/c → (i) small amounts are secreted, and (ii) they are secreted into the hypothalamic-hypophysial portal system
- Nature of release from hypothalamus:
- Pulsatile manner → can vary with circadian rhythm, but induced in the presence of specific stimuli (Eg. cold, stress, Etc.)
- Regulated by –ve feedback (esp from hormones secreted by peripheral organs) EXCEPT PRL (see below)
- Types of hormones:
- Thyrotrophin-releasing hormone (TRH) → tripeptide (3 a.a.) → stimulates TSH secretion from thyrotropes
- Corticotrophin-releasing hormone (CRH) → 41 a.a. peptide → stimulates ACTH secretion from corticotropes
- Gonadotrophin-releasing hormone (GnRH) → 10 a.a. peptide → stimulates LH and FSH secretion from gonadotropes
- Growth-hormone releasing hormone (GHRH) → 43 a.a. peptide → stimulates GH secretion from somatoropes
- Somatostatin (GHIH) → 14 a.a. peptide → suppresses GH secretion from somatotropes (also ACTH, TSH and PRL release; also inhibits insulin/glucagon)
- Prolactin releasing factor (PRF) → stimulates PRL secretion from lactotropes
- Dopamine (DA) → suppresses PRL secretion from lactotropes
Bianca 2016
Examiner Comments
2021A 13: 40% of candidates passed this question.
Few candidates described cell types as chromophils and chromophobes. There were many errant references to chromaffin cells which are found mainly in the adrenal medulla, and to staining on H&E. Chromophil cells stain by absorbing chromium salts. Few candidates mentioned that the hormones secreted by the anterior pituitary are peptides. Most candidates outlined the hypophyseal-portal system well. Knowledge of TSH and ACTH control and target organ effects were good. Similar knowledge for LH, FSH, PRL and GH was much more sporadic.
2009B 21
List the hormones secreted by the pituitary gland. (30% marks)
Outline the physiological factors that control secretion of hormones from the posterior pituitary. (70% marks)
CICMWrecks Answer
Pituitary
- HPA describes complex feedback loops between these endocrine organs
- Shortloop feedback: -ve feedback from pituitary on the hypothalamus e.g. thyroxin inhibiting TSH release
- Long-loop feedback: -ve feedback from pituitary target gland (e.g. thyroid, adrenal, gonads) on the hypothalamus e.g. cortisol inhibiting CRH (as well as ACTH) release
- Pituitary hormones
- Anterior pituitary
- Secretes 6 hormones in response to hypothalamic endocrine stimulus
- Stimulating hormones:
- Act at another gland
- Includes: ACTH, TSH, FSH, LH
- Directly acting hormones
- Include: GH, prolactin
- Posterior pituitary
- ADH
- Oxytocin
- Anterior pituitary
Control of secretion of hormones from the posterior pituitary
ADH:
- Nonapeptide (9 a.a.) synthesized 1°ly in cell body of SON (some also in PVN) of the
hypothalamus → transported to posterior pituitary via infundibulum where it is stored - It is secreted in response to:
- ↑ plasma osmolality (Major determinant)
- Detected by osmoreceptors (in anterior hypothalamus near SON/PVN)
- Very sensitive (detects 1% change in osmolality) → threshold for ADH
release is 280 mosm/kg (slightly less than normal plasma osmolality) →
steep linear rise > 290 mosm/kg
- Non-osmotic stimuli:
- Haemodynamic changes
- ↓ PV → ↓ MAP that is sensed by baroreceptors (mainly lowpressure BR in atrium) → cause ↑ ADH release
- ↓ sensitivity cf. osmotic stimuli (detects 5-10% change in PV)
- BUT very potent → overrides osmoreceptors (in terms of control
of ADH secretion) when there are LARGE changes in PV!!!
- ↑ AII
- Pain
- Nausea/vomiting (powerful stimuli)
- Exercise
- Drugs (↑ release – morphine, nicotine, barbiturate; ↓ release – EtOH)
- Haemodynamic changes
- ↑ plasma osmolality (Major determinant)
- Effects:
- V1 receptor (GPCR via Gq → activates PLC to ↑ IP3 → ↑ IC [Ca2+] → smooth muscle contraction) → this causes:
- Contraction of vascular SM cells (potent vasoconstrictor effect) → ↑ TPR and MAP
- Renal afferent arteriolar constriction and contraction of renal mesangial cells → ↓ GFR/RBF
- Platelet aggregation and degranulation
- V2 receptor (GPCR via Gs → activates AC to ↑ cAMP → activates PKA) → this causes:
- Upregulates insertion of apical membrane AQP2 (stored in vesicles) in principal cells of CCD and MCD → ↑ H2O permeability → ↑ H2O reabsorption into hypertonic medullary interstitium (across BLM AQP3 and 4) → causes ↓ plasma osmolality (and ↑ urine concentration)
- Upregulates “urea transporters” in principal cells of inner MCD → ↑ permeability to urea → ↑ urea absorption to maintain ↑ medullary osmolality (strengthens CCM)
- ↑ Na+ reabsorption and K+
secretion by principal cells of CCD - ↑ CF VIII release by vascular endothelium
- Other effects:
- CNS → promotes memory, learning, attention and concentration
- ACTH release form anterior pituitary gland
- V1 receptor (GPCR via Gq → activates PLC to ↑ IP3 → ↑ IC [Ca2+] → smooth muscle contraction) → this causes:
- ADH’s effect is very short-lived → short t ½ ~ 20 mins (rapidly inactivated by tissue peptidases → excreted by liver and kidney)
Oxytocin
- Nonapeptide (9 a.a.) synthesised 1°ly in cell body of PVN (some also in SON) of the hypothalamus → transported via infundibulum to be stored in posterior pituitary gland
- Control of secretion – (i) ↑ release in response to → cholinergic stimulation, (ii) ↓ release in response to → β-adrenergic activity, EtOH, enkephalins
- Effects:
- Ejection of milk – Somatic touch stimulation of nipple (Ie. suckling) stimulates “let-down reflex” → cause oxytocin release to induce contraction of myoepithelium of lactating mammary glands → milk secretion
- Myometrial contraction of pregnant uterus → during late pregnancy, a neuroendocrine reflex loop causes ↑ both oxytocin secretion and oxytocin receptor population → role in inducing labour/delivery
- Uterine secretion/contractions during coitus → facilitates propulsion of semen to fallopian tubes
- Various behavioural effects
Bianca / Kerr 2016
Full Pituitary Hormone Table
| Location | Hormone | Action | Stimulated by: | Inhibited by: |
|---|---|---|---|---|
| Anterior pituitary | ACTH | Short chain peptide Stimulates cortisol release from zona fasiculata | CRH | Cortisol |
| TSH | Glycoprotein Stimulates synthesis + release of T3 + T4 | TRH | T3 | |
| FSH | Glycoprotein gonadotropin Females: stimulates oestrogen synthesis + ovarian follicle development Males: stimulates sperm maturation | GnRH | Sex steroids | |
| LH | Glycoprotein gonadotropin Females: rapid ↑ stimulates ovulation + corpus luteum development Males: stimulates testosterone synthesis | |||
| GH | Long chain peptide released in pulsatile fashion Anabolic effects: directly stimulates lipolysis → ↑FFA Indirectly stimulates IGF-1 release → promoting cell growth + development | GHRH High with exercise, hypoglycaemia, stress | Somatostatin IGF-1 | |
| Prolactin | Long chain peptide breast development during gestation + lactation post delivery | |||
| Posterior pituitary | ADH | Short chain peptide Acts on: – V1 R in vascular smooth muscle → vasoconstriction – V2 R in CD (↑water reabsorption) + endothelium (↑vWF FVIII release) – V3 R in pituitary → stimulate ACTH release | Hypothalamic neural stimulus | |
| Oxytocin | Short chain peptide; structurally similar to ADH Causes: uterine contraction, let down reflex, psychological, bonding |
Kerr 2016
Examiner Comments
2009B 21: 4 (44%) of candidates passed this question.
Once again candidates are reminded to read and answer the question presented to them as well as take into consideration the proportion of marks allocated. The expectation from the first section of the question was for candidates to only “list” the hormones secreted by the pituitary gland. The main hormones expected were ACTH, TSH, GH, FSH, LH and prolactin anteriorly; and, ADH (vasopressin) and oxytocin posteriorly.
Unfortunately, a number of candidates confused which hormones come from which region and therefore were unable to score marks in the second part. The question clearly asked for factors controlling secretion of hormones from the posterior pituitary, therefore, detailed descriptions of the mechanism of action of ADH in the kidney, or of hormones arising from the anterior pituitary did not relate to the question and were not allocated marks.
With respect to ADH, most marks were gained by candidates who described not only osmolality and plasma volume, but the relative sensitivity of the pituitary to these and the pre-potent nature of volume over osmolality; also, the influence of other hormonal axes involved in plasma volume regulation. Marks were also available for other inputs including pain, stress, exercise, etc. A brief description of factors influencing oxytocin was also expected.
Syllabus – N12d
Reference: Gannong p383, Guyton p359
2023A 16
Outline the role of the hypothalamus.
2018A 20
Outline the structure (20% of marks) and function (80% of marks) of the hypothalamus.
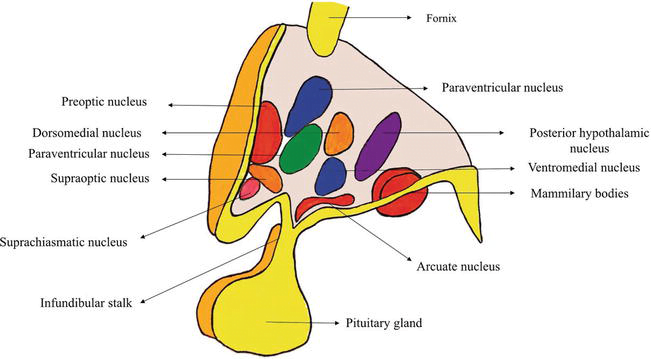
CICMWrecks Answer
Hypothalamus
- Hypothalamus
- organ that regulates large number of autonomic/ endocrine processes
- acts as control centre
- Cells
- magnocellular neurosecretory cells in the paraventricular nucleus and the supraoptic nucleus of the hypothalamus produce neurohypophysial hormones, oxytocin and vasopressin. These hormones are released into the blood in the posterior pituitary.
- Much smaller parvocellular neurosecretory cells, neurons of the paraventricular nucleus, release corticotropin-releasing hormone and other hormones into the hypophyseal portal system, where these hormones diffuse to the anterior pituitary.
- Location
- Part of the fore brain. Considered part of the diencephalon
- Located below the thalamus and forms the floor and lower part of the lateral walls of the third ventricle
- Anteriorly extends up to the optic chiasma
- Posteriorly continuous with the tegmentum of midbrain
- Structure
- formed by gray matter conglomeration of neurons that organize in nuclei and also by white-matter substance formed by myelinated nervous fibers.
- Nuclei send and receive fibers to other parts of brain
- divided by the anterior horns of the fornix in a lateral, medial, and periventricular (median) region and by a coronal plane passing through the infundibulum in an anterior and posterior region.
- Regions
- Anterior / Prechiasmatic / Supraoptic
- located above the optic chiasm
- contains: supraoptic, preoptic and medial preoptic, the suprachiasmatic and the anterior hypothalamic nucleus, alongside with the paraventricular nucleus
- Infundibular / Tuberal
- located above tuber cinereum (between anterior and posterior)
- composed of two parts, anterior and lateral
- contains: dorsomedial, ventromedial, paraventricular, supraoptic, and arcuate nucleui
- Posterior / Mamillary
- formed by medial and lateral area
- medial area contains mamillary nuclei and posterior nucleus
- lateral area contains lateral nucleus and tuberomammillary nucleus
- Anterior / Prechiasmatic / Supraoptic
- Connections: Nervous, Endocrine, CSF, Direct to pituitary
- Blood supply
- mainly hypophyseal artery (branch of anterior cerebral artery)
- Detailed arterial supply:
- Anterior: branches of ACA and ACOM
- Tuberal: branches of PCOM and superior hypophyseal artery
- Posterior: branches of PCA
- Infundibulum: superior hypophyseal arteries from the ophthalmic branch of ICA (C6)
- drains into hypothalamohypophyseal system of veins to anterior pituitary → hypophyseal vein
Function of Hypothalamus
Autonomic nervous system activity
- CVS:
- Ant hypothalamic stimulation → ↓BP + ↓HR
- Post hypothalamic stimulation → ↑BP + ↑HR
- Thermoregulatory: integrates thermoreceptor input + controls activity of heat loss + heat gain mechanisms
- Satiety: hunger modulated by glucose, CCK, glucagon, and leptin
- Water balance:
- Osmoreceptors: control ADH release from posterior pituitary
- ATII: stimulates thirst + ADH release via subfornical organ + organum vasculosum
- Circadian rhythm
- Behaviour
- Sexual function
Endocrine/ hormonal activity
- Direct neural control of posterior pituitary gland
- Pituitary neurosecretory neurons
- Magnocellular neurons:
- consists of SON + PVN
- synthesise and secrete ADH and oxytocin
- Parvocellular neurons:
- form tuberoinfundibular tract → secrete hypophysiotropic hormones
- release controlled by Nad, dopamine, 5-HT
- Magnocellular neurons:
- Hypothalamic hormones → action in pituitary
- Anterior pituitary by hormone secretion into long portal vein
- GnRH → stimulates FSH + LH release
- CRH → stimulates ACTH release
- GHRH → stimulates GH release
- TRH → stimulates TSH release
- Somatostatin (GH inhibiting hormone) → inhibits GH, TSH, ACTH, and PRL release
- PRL releasing hormone (PRH) → stimulates PRL release
- Dopamine → inhibits PRL release
- Posterior pituitary by neuronal innervation
- ACh → stimulates release of ADH + oxytoxin
- NAd → inhibits ADH + oxytocin secretion
- Anterior pituitary by hormone secretion into long portal vein
(See next tab for detailed table of nuclei with functions, and communications of hypothalamus)
Sources: https://www.intechopen.com/chapters/63258
https://human-memory.net/hypothalamus/#Structure
JC / Kerr 2022
Additional: Nuclei and functions Table, Communications
Nuclei and functions
| Region | Area | Nucleus | Function |
|---|---|---|---|
| Anterior (Supraoptic / prechiasmatic) | Preoptic | Preoptic nucleus | – Thermoregulation |
| Medial | Medial preoptic nucleus | – Regulates the release of gonadotropic hormones from the adenohypophysis – Contains the sexually dimorphic nucleus, which releases GnRH, differential development between sexes is based upon in utero testosterone levels – Thermoregulation | |
| Supraoptioc nucleus | – Vasopressin release – Oxytocin release | ||
| Paraventricular nucleus | – thyrotropin-releasing hormone release – corticotropin-releasing hormone release – oxytocin release – vasopressin release – somatostatin round | ||
| Anterior hypothalamic nucleus | – thermoregulation – panting – sweating – thyrotropin inhibition | ||
| Suprachiasmatic nucleus | – Circadian rhythms | ||
| Lateral | Lateral nucleus | primary source of orexin neurons that project throughout the brain and spinal cord – Mainly promotion of feeding behaviour and arousal | |
| Infundibular (Middle / tuberal) | Medial | Dorsomedial hypothalamic nuclei | – blood pressure – heart rate – GI stimulation |
| Ventromedial nucleus | – satiety – neuroendocrine control | ||
| Arcuate nucleus | – Growth hormone-releasing hormone (GHRH) – feeding – Dopamine-mediated prolactin inhibition | ||
| Lateral | Lateral nucleus | primary source of orexin neurons that project throughout the brain and spinal cord – Mainly promotion of feeding behaviour and arousal | |
| Lateral tuberal nuclei | – regulation of feeding. Its absence or destruction has been implicated in extremes of starvation such as anorexia nervosa. | ||
| Posterior (mamillary) | Medial | Mamillary nuclei (part of mamillary bodies) | – memory |
| Posterior nucleus | – Increase blood pressure – pupillary dilation – shivering – vasopressin release | ||
| Lateral | Lateral nucleus | primary source of orexin neurons that project throughout the brain and spinal cord – Mainly promotion of feeding behaviour and arousal | |
| Tuberomammillary nucleus | – arousal (wakefulness and attention) – feeding and energy balance – learning – memory – sleep |
Communications of Hypothalamus
- Nervous connections: divided into afferent and efferent fibers
- Afferent fibres: carry somatic and visceral sensations as well as from special senses
- Somatic and visceral afferents via lemniscal afferent fibers and nucleus of tractus solitarius, that reach the hypothalamus via reticular formation
- Visual afferents from the optic chiasma reach the suprachiasmatic nucleus
- Olfactory afferents are received through medial forebrain bundle
- Auditory afferents though not identified completely but are influenced by the hypothalamus
- Hippocampo-hypothalamic afferents reach via fornix to mamillary bodies
- Tegmental fibers from midbrain
- Thalamo-hypothalamic fibers from the midline and dorsomedial nuclei of the thalamus
- Amygdalo-hypothalamic fibers from the amygdaloid complex reach the hypothalamus via stria terminalis
- Efferent fibers: complex and numerous
- To brain stem and spinal cord: The hypothalamic nuclei send efferent fibers to nuclei present in the brainstem and spinal cord. In this way, they control the autonomic nervous system.
- Mammillothalamic Tract: This tract consists of fibers arising in the mamillary body and terminating in the anterior nucleus of thalamus.
- Mammillotegmental Tract: These fibers terminate in the reticular formation, present in the tegmentum of the midbrain.
- Limbic System: The nuclei in the hypothalamus also send efferent fibers to the various nuclei of the limbic system.
- Afferent fibres: carry somatic and visceral sensations as well as from special senses
- Endocrine:
- regulating factors or hormones released by hypothalamus → reach pituitary via the hypophyseal portal system of veins → cells of pituitary release hormones
- Direct:
- Cell bodies present in hypothalamus → axonal terminals in posterior pituitary gland
- Bodies synthesise oxytocin and vasopressin, stored in axonal terminals in posterior pituitary and released on demand
- CSF:
- clear metabolic waste
- distribute glucose, amino acids, lipids, and neurotransmitters
Examiner Comments
2023A 16: 29% of candidates passed this question.
This question required candidates to integrate parts of the syllabus that are often not presented together in the reference texts. Many candidates provided only an incomplete list of the roles of the hypothalamus as their answer which did not score enough marks to pass. Additionally, presenting information succinctly and in a format that demonstrated an understanding of priority of function with respect to the CICM syllabus, was critical for time management and ensuring that more the important/major roles were presented in more detail. This question required candidates to cover roles including autonomic control, thermoregulation, hormonal regulation, body rhythms and regulation of drives with feedback control mechanisms where appropriate. Those who scored well demonstrated a comprehensive breadth of knowledge of these areas as well as giving the pertinent points around areas of positive and negative feedback and the sensor areas and effector responses required to answer an outline question.
2018A 20: 21% of candidates passed this question.
Most candidates understood the endocrine functions of the hypothalamus, and to some degree its interactions with the pituitary. Fewer candidates mentioned the importance of the hypothalamus as an integrator for the autonomic nervous system, or its roles in arousal/emotions.
Many candidates had only a vague idea of the structure of the hypothalamus, while the best candidates were able to relate function to structure quite accurately
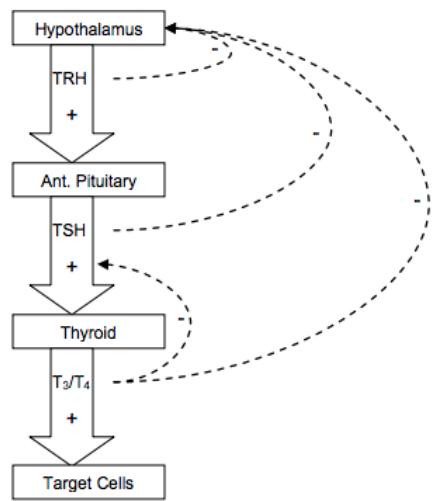
v. Describe the control, secretions, and functions of the thyroid.
2021B 14
Describe the production, action and regulation of thyroid hormones.
2016A 17
Describe the physiology of the thyroid hormones.
CICMWrecks Answer
Thyroid Hormones
- 3 main thyroid hormones
- thyroxine (T4): 95%; ½ life 7 days; less active
- tri-iodothyronine (T3): 7%; ½ life 24hrs; 3-5x activity of T4
- reverse T3 (rT3): inactive
- T3 + T4 formed from iodination of aa tyrosine
- iodine obtained from diet in form of iodide + actively taken up into thyroid follicular cells (req 120-150ug/day)
- Release
- TRH from hypothalamus → stimulates TSH release → binds to R on cell membrane of follicular cells, GPCR → ↑cAMP → ↑AC →
- ↑iodine uptake into follicular cells
- ↑synthesis of T3 + T4 via ↑iodination + ↑rate coupling reactions
- ↑proteolysis of thyroglobulin within follicular cells → liberate T3 + T4
- MoA
- T3 + T4 highly protein bound (>99%) predominantly to thyroxine binding globulin, albumin, thyroxin binding pre-albumin
- Thyroid hormones enter cell → T3 binds to intracellular thyroid receptors (TR) → hormone receptor complex = transcription factors (bind to DNA via zinc fingers) → alter gene transcription → clinical effects
- T4 de-iodinated to T3
Production and Regulation
Synthesis
- Steps:
- dietary iodine converted to iodide for absorption
- iodide actively transported into follicular cells in thyroid (trapping) → oxidised to iodine (via thyroid peroxidase)
- iodine binds tyrosine in thyroglobulin molecule (iodinase) → forms mono-iodotyrosine then di-iodotyrosine (peroxidase)
- di-iodotyrosine + di-iodotyrosine = thyroxine (T4) (perixodase) → binds thyroxine binding globulin + thyroxine binding pre-albumin
- ↑activity with TSH of:
- iodide pump activity
- thyroid peroxidase
- iodinase
- peroxidase
- vesicular lysosomal activity
- thyroid hormones formed within thyroglobulin; synthesised in golgi apparatus
- thyroglobulin stored in follicular colloid → vesicular lysosomal activity breaks down thyroglobulin to release T3 + T4 which diffuse out of follicular cells and into circulation
Metabolism of thyroid homrones
- T4 deiodinated to T3/ rT3 (inactive compound 1:1) → deiodinated in liver, kidney, skeletal muscle to inactive compounds
Negative feedback
Physiological Action
| System | Action | Physiological + pathological effects |
|---|---|---|
| CNS | Development | – normal CNS development – ↓T → ↓CNS development → retardation, rigidity, deaf-mutism – sexual function |
| CVS | Chronotrope Inotrope Vasodilation | – ↑number β-adrenoceptors → ↑HR – ↑circulating catecholamines → ↑contractility + ↑CO – ↑T → ↑body temp → vasodilation → ↓SVR |
| Resp | Metabolic | – ↑T → ↑metabolic rate → ↑MV |
| Bone | Anabolic | – essential for normal bone growth |
| ANS | Stimulatory | – ↑T → synergy with circulating catecholamines → ↑SNS |
| Metabolic / endocrine | Cellular effect Feedback Anabolic/ catabolic | – ↑Na/K ATPase activity → ↑MR of cells + calorigenic – feedback inhibition → ↓TRH + ↓TSH ; ↑T → ↑GH release – CHO: ↑CHO absorption – Fat: ↑lipolysis; ↑LDL Rs → ↑ liver uptake circulating cholesterol – Protein: physiological amounts: ↑protein synthesis; excess amounts: protein breakdown (thyrotoxic myopathy) |
Kerr 2016
Examiner Comments
2021B 14: 81% of candidates passed this question.
This question was divided in three sections to help candidates formulate an answer template, which for the most part was answered well. Most answers included a detailed description of the production and regulation of thyroid hormones, including the importance of negative feedback. A brief description of the action of thyroid hormones on intracellular receptors, and a system-based description of physiological effects, including CHO, protein and fat metabolism was expected.
2016A 17: 40% of candidates passed this question.
Thyroid hormones consist of thyroxine (T4), tri-iodothyronine (T3) and reverse T3 (rT3). It was expected candidates would briefly describe each of these. T4 is a pro-hormone synthesized from tyrosine in follicular cells of the thyroid gland and represents 80% of body’s thyroid hormone production. It exists in free form, plasma protein bound (albumin and pre-albumin (TBPA) and tissue protein bound thyroid-binding globulin (TBG) and has a half-life around 7 days. Tri-iodothyronine (T3) is the most biologically active thyroid hormone (5 times T4), is produced directly from tyrosine (20%) or in the periphery by conversion of T4 (80%) with a half-life 1.5 days. Reverse T3 (rT3) is formed via peripheral conversion of T4 by de-iodination.
A classic negative feedback loop exists to control thyroid hormone secretion. Thyroid Stimulating Hormone (TSH) from the anterior pituitary is controlled by Thyrotropin Releasing Hormone (TRH) from the Hypothalamus via hypothalamic-hypophyseal portal system. Both of these factors are inhibited by elevated levels of T4 and T3.
The mechanism of action is by binding to nuclear receptors to effect protein synthesis. Thyroid hormone has a wide variety of physiological effects across many systems including respiratory, cardiovascular, metabolic and growth and sexual function.
The answer required candidates to detail both the synthesis and control of thyroid hormones as well discussing the action of thyroid hormones. Few candidates could differentiate the roles and actions of T3 and T4.
2008B 15
Outline the physiological consequences of hyperthyroidism in an adult.
CICMWrecks Answer
- Metabolic:
- Increased basal metabolic rate (metabolic rate increased in nearly all cells)
- Carbohydrate
- ↑absorption
- ↑gluconeogenesis
- ↑insulin secretion
- ↑cellular glucose uptake
- Lipid
- ↑absorption
- ↑resorption from adipose tissue
- → ↑plasma free fatty acids
- ↑removal of cholesterol by liver (excreted in bile)
- → ↓plasma cholesterol
- Protein
- ↑muscle catabolism
- CVS:
- +ve inotropy
- +ve chronotropy
- Vasodilation (so BP stays roughly the same)
- Resp:
- ↑VT and ↑RR
- Due to higher metabolic rate
- ↑VT and ↑RR
- Neuro:
- Lowered seizure threshold
- Anxiety
- Insomnia
- GIT:
- Increased motility
- MSK:
- ↑contractility
- Late effects of protein catabolism -> muscle wasting and weakness
Mooney 2016
Examiner Comments
2008B 15: 0 (0%) candidates passed this question
This question sought an understanding of the physiological effects of thyroid hormones. The major area of weakness for candidates was a lack of detailed understanding of the physiological actions of thyroid hormones and/or providing an answer that predominately listed clinical manifestations. A good answer would have included the following points –
- Stimulation of Carbohydrate Metabolism – all aspects of carbohydrate metabolism, including rapid uptake of glucose by the cells, enhanced glycolysis, enhanced gluconeogenesis, increased rate of absorption from the gastrointestinal tract, and increased insulin secretion
- Stimulation of Fat Metabolism – all aspects of fat metabolism are also enhanced lipids are released from fat stores and increased oxidation of free fatty acids by the cells – decreases the concentrations of cholesterol, phospholipids, and triglycerides in the plasma, even though it increases the free fatty acids
- Increased Basal Metabolic Rate – increased CMRO2
- Increased Requirement for Vitamins
- Increased vasodilatation, Cardiac Output, heart rate (not BP), contractility
- Increased Respiration – secondary to increased metabolism
- Increased Gastrointestinal Motility and secretions
- Excitatory Effects on the Central Nervous System, seizures and insomnia
- Effect on the Function of the Muscles – stimulates contractility and metabolism, but too much leads to the muscles become weakened because of excess protein catabolism. Also muscle tremor by increased reactivity of the neuronal synapses in the areas of the spinal cord that control muscle tone
- Effect on Other Endocrine Glands – . increases the rate of glucose metabolism everywhere in the body and therefore causes a corresponding need for increased insulin and glucagon secretion by the pancreas.
- Also, increase bone formation and, as a consequence, increases the need for parathyroid hormone. Thyroid hormone also increases adrenal glucocorticoid metabolism by the liver.
Syllabus: N2e
Reference Text: Guyton Chp 76
vi. Describe the control, secretions, and functions of renal and adrenal hormones.
2017A 04
Describe the endocrine functions of the kidney.
CICMWrecks Answer
Non-RAAS Endocrine Functions
Vitamin D
Vitamin D has a complex metabolic pathway which meanders through a number of organ systems:
- Vitamin D2 (ergocalciferol) only in diet
- Vitamin D3 (cholecalciferol) absorbed in diet or produced in skin by the action of UV light
- 7-dehydrocholesterol à 7-dehydroxycholecalciferol à cholecalciferol
- Liver: Cholecalciferol hydrolysed à 25-hydroxycholecalciferol (25-OHD3)
- Enzyme: Vitamin D25-hydroxylase (CYP450 enzyme)
- Released into plasma, binds to Vitamin D-binding protein (a globulin carrier protein)
- Kidney: 25-OHD3 hydrolysed à 1,25-dihydroxycholecalciferol (calcitriol – active form)
- in the proximal tubule, Enzyme: 1alpha hydroxylase
- Released into circulation
- Transported by Vitamin D binding enzyme to intestine, kidney, bone
Erythropoietin
Secretion of EPO to stimulate RBC production.
Erythropoiesis is stimulated by EPO release:
- In adults, EPO is released from the:
- Peritubular capillary fibroblasts (85%)
- Liver (15%)
- EPO is released in response to:
- Hypoxia (near the secretory cells which lie in between the cortex and medulla)
- Hypotension
- Low Hct
- Erythropoiesis is inhibited by:
- High red cell volume
Production of EPO is decreased in renal failure, which is why patients with end-stage renal disease require exogenous EPO.
Prostaglandins:
Production of prostaglandins esp PGE2 and prostacyclin – potent renal vasodilators
Bradykinin:
Production of bradykinin – potent renal vasodilator
RAAS
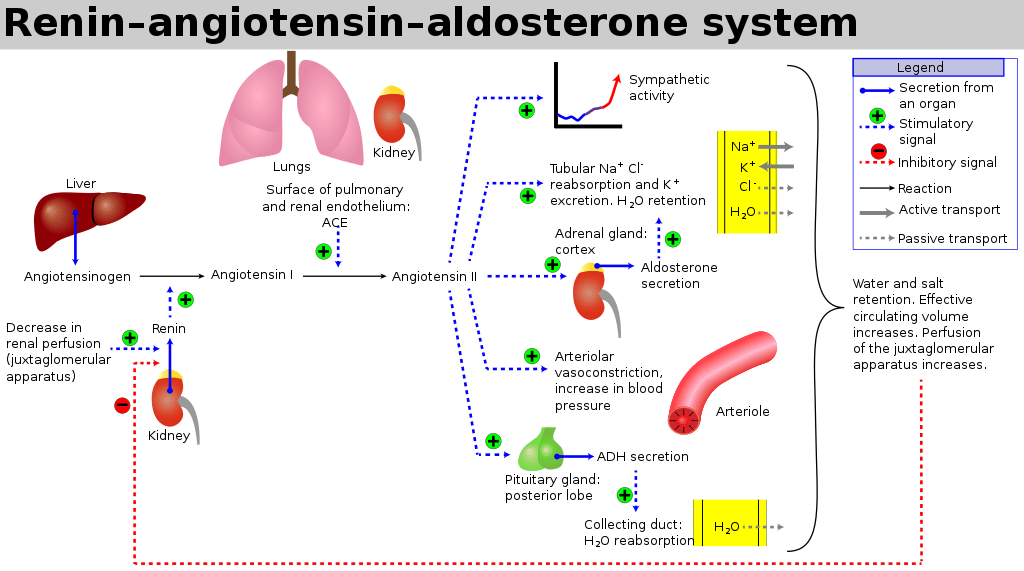
The RAAS is a signaling pathway involved in blood pressure control. It involves a number of hormones:
- Angiotensinogen is produced by the liver
- Renin is a protease enzyme (Half-life 80mins)
- produced by the kidneys
- stored by the granular cells of the juxtaglomerular apparatus, which lies close to the glomerulus and distal tubule
- Secretion is stimulated by:
- Pressure changes in the afferent arteriole
- Stimulation of the macula densa when changes occur in tubular NaCl concentration
- Renal sympathetic nerve activity (a direct β1 effect)
- Baroreceptor reflexes
- Negative feedback from AT II
- Exists to cleave hepatic angiotensinogen to the 10-AA peptide angiotensin I
- Note: Renin is rate-limiting step for activation of RAAS
- Angiotensin I
- has mild vasoconstrictor properties, but not enough to cause significant changes in circulation
- Angiotensin Converting Enzyme (ACE)
- Found mainly in pulmonary vascular endothelial cells – converts angiotensin I to angiotensin II
- Also cleaves bradykinin into inactive metabolites
- Angiotensin II
- Effects include a general reduction in sodium and water excretion, and maintenance of circulating blood volume, GFR and blood pressure.
- Rapidly removed from circulation in 1-2mins, presumably by tissue peptidases (Angiotensinases)
- Aldosterone
- is secreted from the zona glomerulosa of the adrenal cortex
- It acts in the renal CCD to enhance the activity of ENaC and K+ secretion by principal cells.
- increases Na+ (and water) reabsorption in exchange for K+ (kidney, gut, salivary, sweat)
JC 2019
Examiner Comments
2017A 04: 39% of candidates passed this question.
It was expected that candidates would discuss the major hormones produced (or activated) by the kidney. These included erythropoeitin, renin and calcitriol. Good answers included the following: the area where the hormone is produced or modified; stimuli for release; factors which inhibit release; and the subsequent actions / effects. Marks were not awarded for hormones that act on the kidney.
2021B 05
Write detailed notes on angiotensin, including its synthesis, role within the body and regulation.
2009B 18
Outline the physiology of, and factors which regulate levels of angiotensin.
CICMWrecks Answer
Angiotensinogen is a peptide hormone produced by the liver
- Angiotensin 1 (decapeptide)
- ↑ Renin by JGA → cleavage of Angiotensinogen → AT1
- No biological activity
- Angiotensin 2 (octapeptided)
- ACE in pulmonary capil endothelia
- → ↑AT2
- Angiotensin 3 (septapeptide)
- 40% of the pressor activity AT2
- 100% of the aldosterone-producing activity
- Angiotensin 4 (hexapeptide)
- Minimal biological activity
Actions of AT2 include:
- Acts via GPCR (Gq via PLC to increase IP3 and intracellular Ca)
- CVS
- Vasopressor
- Resets baroreceptor control of HR at higher pressure
- Potent mitogen for smooth muscle and cardiac myocytes
- Direct positive inotrope
- CNS
- ↑ sympathetic outflow
- ↑ thirst
- ↑ ADH release from posterior pituitary.
- Renal
- Negative feedback on renin release
- ↑ aldosterone release
- ↓ RBF and GFR
- Direct renal arteriole constriction (efferent = afferent)
- Mesangial cell contraction thus ↓ Kf and GFR
- ↑ sodium/chloride reabsorption in PCT
- Direct effect and via ↑ aldosterone release
Factors which alter renin release cause a corresponding change in Angiotensin 2
- Stimulation of renin secretion (↑ renin → ↑ angiotensin 2)
- β-1 agonism
- ↓ renal perfusion pressure
- ↓ sodium delivery to DCT
- Prostaglandins
- Inhibition or renin secretion (↓ renin → ↓ angiotensin 2):
- ↑ renal perfusion pressure (via afferent arteriolar dilatation)
- ↑ sodium delivery to DCT
- ↑ by angiotensin II (negative feedback) and vasopressin
Gladwin 2016
Examiner Comments
2021B 05: 24% of candidates passed this question.
This question provided headings for the answer template. Good answers integrated the required facts from the appropriate chapters of the major texts. Most answers lacked detail surrounding the factors that increase or decrease angiotensin activity. Few answers provided any detail as to all the mechanisms through which angiotensin exerts it effects. A lot of answers focussed singularly on the vascular effects of angiotensin. Overall, there was often a paucity of detail, with vague statements and incorrect facts.
2009B 18: 4 (44%) of candidates passed this question.
For a good answer it was expected that candidates would mention the relationship of angiotensinogen, angiotensin I, renin and Angiotensin Converting Enzyme to angiotensin II production, the actions and fate of angiotensin II and factors that regulate angiotensin II. It was expected that candidates mention angiotensin acts as a potent vasoconstrictor, stimulates aldosterone secretion, facilitates noradrenaline release, preferentially vasoconstricts Efferent arteriole in nephron, preserving GFR in low perfusion states, increases renal tubular Na + reabsorption and increases secretion of vasopressin and ACTH.
Regulation of Angiotensin could be separated into factors increasing angiotensin levels (eg prostaglandins, low K+ levels, Sympathetic stimulation, ↓ Na+ delivery at distal tubule, any factor contributing to reduced renal blood flow (eg hyovolaemia, cardiac failure, renal artery stenosis) and factors reducing angiotensin levels (eg hypervolaemia, afferent arteriolar dilatation and vasopressin).
Syllabus – N1 (h), C2b (f)
Reference: Textbook of medical Physiology, Guyton, Chp 26, Goodman and Gillman, Chp 30
2011B 06
Describe the physiology of the Renin and Angiotensin system.
CICMWrecks Answer
Renin-Angiotensin-Aldosterone system primarily for hormonal regulation of blood volume.
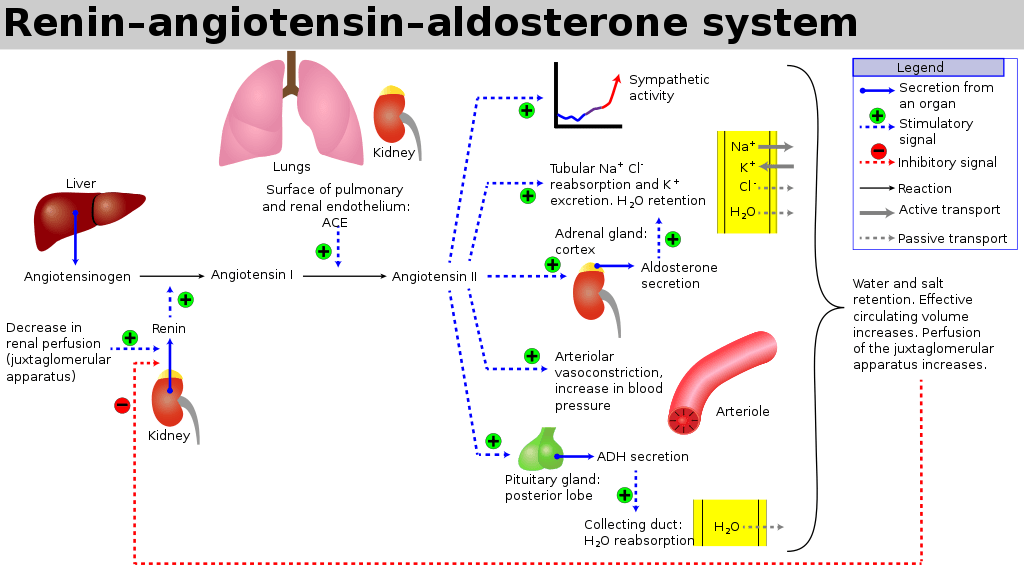
Renin
- Proteolytic enzyme
- Secreted from granula cells in juxtaglomerular apparatus
- Secretion:
- Stimulated by:
- ↓ GFR
- ↓ tubular Na/Cl at macula densa
- β1 SNS stimulation of granular cells
- ↑ prostacyclin levels
- ↓ levels of angiotensin 2 or ADH
- Inhibited by:
- ↑ renal perfusion pressure
- ↑ sodium delivery to DCT
- ↑ by ATII and ADH
- Stimulated by:
- Target:
- circulating angiotensinogen
- Effects:
- Tubular effects:
- ↑’d PCT Na/Cl reabsorption, ↑’d tubular K secretion
- Direct PCT effect
- Aldosterone release
- Volume Status effects:
- ↑’d total body water via
- ↑’d thirst (hypothal)
- ↑’d ADH secretion
- Renal Blood flow effects
- Direct: Reduced RBF and GFR (Aff>Eff)
- ↑’d renin → ↑ AT2 (see AT2 below) → ↑’d Aldosterone
- Vasoconstriction (aff=eff)
- Mesangial cell contraction
- Tubular effects:
Angiotensin 2
- Production:
- Angiotensinogen is the precursor peptide hormone produced by the liver
- Angiotensin 1 (decapeptide)
- ↑ Renin by JGA (above) → cleavage of Angiotensinogen → AT1
- No biological activity
- Angiotensin 2 (octapeptided)
- Angiotensin Converting Enzyme (ACE) in pulmonary capil endothelia
- → ↑AT2
- Angiotensin 3 (septapeptide)
- 40% of the pressor activity AT2
- 100% of the aldosterone-producing activity
- Angiotensin 4 (hexapeptide)
- Minimal biological activity
- Target:
- Mesangial cells, arteriolar SM, CNS, posterior pituitary
- AT1 and AT2 receptors
- Acts via GPCR (Gq via PLC to increase IP3 and intracellular Ca)
- Effect:
- CVS
- Vasopressor
- Resets baroreceptor control of HR at higher pressure
- Potent mitogen for smooth muscle and cardiac myocytes
- Direct positive inotrope
- CNS
- ↑’d sympathetic outflow
- ↑’d thirst
- ↑’d ADH release from posterior pituitary.
- Renal
- Negative feedback on renin release
- ↑’d aldosterone release
- ↓’d RBF and GFR
- Direct renal arteriole constriction (efferent = afferent)
- Mesangial cell contraction thus ↓’d Kf and GFR
- ↑’d sodium/chloride reabsorption in PCT
- Direct effect and via ↑’d aldosterone release
- CVS
Aldosterone
- Steroid Hormone
- Source:
- Adrenal cortex (zona glomerulosa)
- Release Stimuli:
- adrenal cortical hyperkalaemia
- ↑’d AT2
- ↑’d ACTH
- Target:
- Distal collecting duct and CCD principal cells ENaC receptors.
- Na/K ATPase co-transporters in DCT/CCD, GIT and secretory glands
- Effect:
- Sodium (↑’d plasma Na)
- Upregulates basolateral ENaC and Na/K ATPase to increase Na reabsoption
- ↑’d Na reabsorption throughout the GIT/sweat and salivary glands via Na/K ATPase
- ↑’d H2O reabsorption and ↑’d Na via solvent drag
- Potassium (↓’d plasma K)
- ↑’d K secreation at DCT/CCD principal cells (via ROMK)
- ↑’d K secretion throughtout the GIT/Salivary glands
- ↑’d intracellular K uptake
- Chloride (↑’d plasma Cl)
- ↑’d Cl uptake in distal tubule
- Acid (H) Effects
- Upregulation of H and H/K-ATPase in type A intercalated cells of CCD
- Increases H secretion (and HCO3 reabsorption)
- Sodium (↑’d plasma Na)
Gladwin 2016
Examiner Comments
2011B 06: 15 (60%) of candidates passed this question.
Renin and angiotensin are core components in the regulation of plasma volume and blood pressure regulation. It is unfortunate that many candidates presenting to this examination are not able to provide sufficient information for a pass. For a good answer, candidates were expected to mention what renin and angiotensin are and what they do, as well as briefly mention the place of angiotensin converting enzyme (converts Angiotensin I to Angiotensin II and inactivates bradykinin). Renin is a proteolytic enzyme cleaves angiotensinogen to angiotensin I, secreted by the juxtaglomerular cells of the kidney which are located in media of afferent arteriole and in close proximity to the glomerulus and the distal convoluted tubule (macula densa). Angiotensin II acts on cell surface AT1 and AT2 receptors. Major functions being to preserve of GFR & enhanced Na/H2O reabsorption in the setting of reduced renal blood flow (candidates expected to outline the mechanism by which this occurs), vasoconstriction, stimulate aldosterone secretion and increase thirst and ADH secretion. The better candidates also mentioned that it decreases sensitivity of baroreceptor reflex, increases secretion of ACTH and facilitates noradrenaline release from sympathetic nervous system as well as its fate (metabolized by blood/tissue peptidases). A good response for regulation would have been mentioning principally regulated via renin release (which in itself is influenced by renal sympathetic nervous system activity, intrarenal baroreceptors and macula densa sodium chloride delivery, ADH and intra-renal prostaglandins), negative feedback from angiotensin II.
Syllabus: N2h
Recommended sources: Textbook of medical Physiology, Guyton, Chp 26.
2019A 06
Outline the physiology of the adrenal gland (70% of marks).
Describe the actions of aldosterone (30% of marks).
CICMWrecks Answer
Adrenal Gland
- Wedges of glandular and neuroendocrine tissue adhering to the top of the kidneys by a fibrous capsule.
- Blood flow:
- have one of the greatest blood supply rates per gram of tissue of any organ: up to 60 small arteries may enter each gland
- Artery → Cortex → Medulla → Veins
- Three arteries:
- Superior Suprarenal A. (Br. Of Inferior Phrenic)
- Middle Suprarenal A. (Br. Of Aorta)
- Inferior Suprarenal A. (Br. Of Renal Artery)
- One Suprarenal on each side:
- Rt Suprarenal drains into IVC
- Lt Suprarenal drains into Lt renal V.or Lt Inferior Phrenic V.
The gland can be divided into:
- Adrenal cortex
- component of the hypothalamic-pituitary-adrenal (HPA) axis
- secretes steroid hormones important for the regulation of the long-term stress response, blood pressure and blood volume, nutrient uptake and storage, fluid and electrolyte balance, and inflammation.
- Adrenal medulla
- neuroendocrine tissue composed of postganglionic sympathetic (SNS) neurons
- The sympathomedullary (SAM) pathway involves the stimulation of the medulla by impulses from the hypothalamus via neurons from the thoracic spinal cord.
- The medulla is stimulated to secrete the catecholamine hormones epinephrine and norepinephrine.
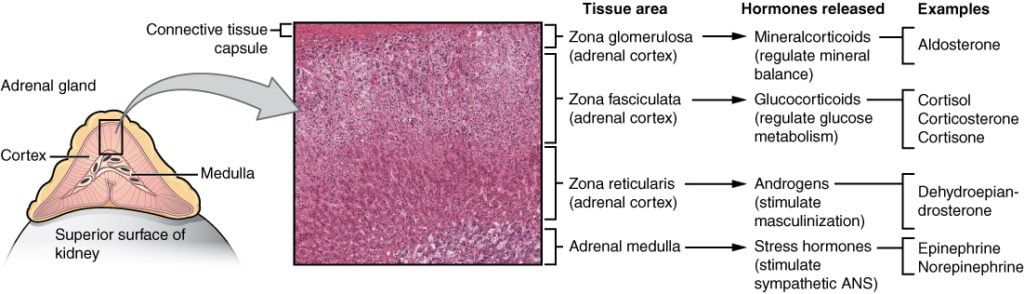
Mineralocorticoids (Aldosterone)
Aldosterone is the key mineralocorticoid hormone, accounting for 95% of mineralocorticoid activity:
- Release is stimulated by:
- Increased serum K+
- Increased Angiotensin II
- Hypovolaemia
- Decreased osmolarity
- Increased ACTH
- Decreased serum pH
- Acts to increase sodium and water retention (and removal of potassium), via:
- Increased expression and activation of Na+/K+ pumps on the basolateral membrane of DCT and CT cells, causing increased Na+ (and water) reabsorption and K+ elimination
- Stimulation of the Na+/H+ pump in intercalated cells on the DCT
- upregulates epithelial sodium channels (ENaCs) in the collecting duct and the colon, increasing apical membrane permeability for Na+ and thus absorption.
- increases Na+ (and water) reabsorption in exchange for K+ (kidney, gut, salivary, sweat)
Sources:
https://opentextbc.ca/anatomyandphysiology/chapter/17-6-the-adrenal-glands/
https://cnx.org/contents/FPtK1zmh@7.28:kaX2y2XZ@3/The-Adrenal-Glands
JC 2019
Examiner Comments
2019A 06: 43% of candidates passed this question.
Lack of breadth and detail were in many of the answers. Physiology of the adrenal gland includes an outline of the adrenal medulla, the types of chromaffin cells, hormones secreted and how secretion is stimulated. The three zones of the adrenal cortex should have been outlined including substances secreted, their function and again how their secretion is stimulated. The actions of aldosterone should have been described; a comment on sodium and water excretion was insufficient to attain many marks for this section. The extra-renal actions of aldosterone were missing from most answers.
vii. Describe the control of plasma calcium.
2017A 05
Describe the regulation of plasma calcium concentration.
2016B 01
Outline the distribution of calcium in normal plasma (20% of marks).
Describe the hormonal control of the calcium concentration in the plasma (80% of marks)
2008A 07
Outline the regulation of plasma calcium concentration.
Outline the mechanism of action of biphosphonates for the management of hypercalcaemia.
CICMWrecks Answer
Normal Calcium: 25,000 mmol (400 mmol/kg)
Distribution:
- Readily exchangeable pool (1%) (ECF esp plasma)
- Total plasma [Ca2+] = 2.12-2.65 mmol/L
- Ionised [Ca2+] = 1.2 mmol/L
- Only the plasma free Ca is physiologically active and regulated by homeostatic mechanisms
- Two pools
- Diffusible (55%)
- 45% free/ionised
- Active form (above)
- 10% complexed
- 45% free/ionised
- Non-diffusible (45%)
- protein bound (esp to albumin)
- pH-dependent (↑ binding with ↑ pH)
- Diffusible (55%)
- Poorly exchangeable pool (99%)
- Bone/teeth (as hydroxyapatite, phosphates, carbonates)
Calcium balance
ECF and hence plasma Ca is the result of a balance between dietary intake, gastrointestinal absorption and excretion, renal excretion and exchange with bone Ca.
Normal Losses:
- Kidneys (40%) → 2.5-7.5 mmol/day
- Filtration of 250 mmol/day
- 95% reabsorbed by tubules
- PCT 65% with Na
- TAL of LoH 20%
- distal nephron 10%
- 5% excreted
- ↑ reabsorption at LoH/distal nephron
- PTH
- 1,25-dihydroxy-vitamin D
- GIT in faeces (60%) → 6-14 mmol/day
Calcium Regulation
- Calcitonin
- 32 AA peptide with 1 disulfide bond it is the hormone of Procalcitonin
- Released from Parafollicular cells (C-cells) of thyroid
- Release Stimuli: Hypercalcaemia, gastrin, beta-agonists, dopamine, oestrogen, CCK, glucagon and secretin
- Effect:
- Increases osteoblast function/Inhibits osteoclast function
- ↓intestinal calcium reabsorption
- inhibition of renal Ca and PO4 reabsorption
- Vitamin D
- Fat soluble sercosteroid from either
- diet or
- synthesis in skin of cholecalciferol from cholesterol then processed in liver and activated in PCT of the kidney
- Release stimuli
- ↑ concentration of PTH causes ↑ 1-alpha-hydroxylase activity in kidney or ↓ Ca or PO4
- Effect:
- ↑ bone release of Ca/PO4
- ↑ intestinal and renal reabsoption of Ca and PO4
- negative feedback on PTH release
- Fat soluble sercosteroid from either
- Parathyroid hormone
- Polypeptide hormone secreted from the parathyroid gland
- Release stimuli:
- ↓ Ca (primary or due to ↑ PO4) sensed by CaSR (Ca sensing receptor) in PT chief cell
- ↓ vitamin D levels
- Effect:
- ↑ Ca/PO4 reabsorption due to ↑ osteoclast activity
- ↑ Vit-D production by kidney (effect on 25 alpha hydroxylase)
- ↑ illeal Ca reabsorption
- ↑ renal reabsoption of Ca/Mg from DCT and TAL loop of henle
- ↓ PCT phosphate reabsorption
Bisphosphonates
- Indication: Hypercalcaemia
- Action:
- Analogues of pyrophosphate in which P-O-P bond is altered to P-C-P bond that is unhydralysable.
- Deposition of the analogue to the bone prevents osteoclast liberation of Calcium
Gladwin 2016
Examiner Comments
2017A 05: 51% of candidates passed this question.
High scoring answers discussed the three major hormones involved in calcium regulation – parathyroid hormone, vitamin D and calcitonin. For each of these it was expected that candidates include: site of production, stimulus for release, inhibitory factors and actions. In the case of renin it was expected that candidates also include the actions of angiotensin and aldosterone. Very few answers discussed inhibitory factors or negative feedback loops.
2016B 01: 53 % of candidates passed this question.
As stated in the question, the distribution in plasma (not body) was expected. Candidates are reminded to include units [mmol/l].
Many candidates spent considerable effort describing the roles of calcium and particularly its role in excitation contraction coupling – which was not asked and hence scored no marks. It was expected that candidates were able to identify the roles of parathormone (PTH), 1,25 OH vitamin D and calcitonin as the major hormonal regulators. Better answers were able to describe the physiology and integration of these hormones at the gut, kidney and bone. Calcitonin and its transient and (probable) minor opposite role were also identified in these answers.
Better answers were also able to identify the permissive roles of growth hormone, cortisol and thyroxine.
2008A 07: 1 candidate (33%) passed this question.
The main points expected for a pass were:
• The components of plasma calcium are diffusible Ca ( free and complexed ) and nondiffusible Ca (protein bound ). Only the plasma free Ca is physiologically active and regulated by homeostatic mechanisms. Plasma free Ca is also affected by plasma pH and albumin concentration.
• The distribution of Ca in the body and the fact that ECF Ca is less than 0.1% of total body Ca. ECF and hence plasma Ca is the result of a balance between dietary intake, gastrointestinal absorption and excretion, renal excretion and exchange with bone Ca.
• Tight hormonal regulation of GIT absorption, bone exchange and renal excretion mainly by parathyroid hormone and calcitriol.
Also expected were details of the actions of PTH on bone and the kidney and the actions of calcitriol on the gut and bone. No candidates described the feedback control mechanisms involving PTH and calcitriol. Additional marks were given for mention of other hormones that have a lesser effect on plasma Ca concentration.
The second part of the question on the mechanism of action of biphosphonates was poorly
answered.
Syllabus N 2i
U2: Endocrine Pharmacology
i. Understand the pharmacology of glucocorticoids.
2011B 24
Describe the pharmacology of corticosteroid drugs
Examiner Comments
2011B 24: 5 (40%) of candidates passed this question.
This question was very broad, requiring the discussion of corticosteroid pharmacology. This embraces the pharmacokinetics, pharmacodynamics and pharmaceutics of the drug class. Synthesis from cholesterol and hepatic metabolism was included in better answers. Comparison of mineralocorticoids versus glucocorticoids was expected. The mechanism of action through binding to intracellular receptors to affect protein synthesis should have been described.
Additional marks were awarded for description of indications, preparations and routes of administration. In any pharmacology question, a list of common adverse effects is important. Of particular relevance is the suppression of the adrenal axis with prolonged administration.
Syllabus: N2 2c
Recommended sources: Stoelting, Pharmacology and Physiology in Anaesthetic Practice, pg 416; Peck & Hill Pharmacology for Anaesthesia and Intensive Care, pgs 355-8.
2012B 24
Compare and contrast peptide and steroid hormones. Give four examples of each.
CICMWrecks Answer
| Peptide Hormone | Steroid Hormone | |
|---|---|---|
| Example | Anterior Pituitary Hormones (FLAGTOP) FSH, LH, ACTH, GH, TSH, Oxytocin, Prolactin | Cortisol, Aldosterone, Oestrogen, Progesterone, Testosterone |
| Structure | Multiple amino acid residues (3-200) Charged surface structure | Lipid soluble Sterol Ring structure |
| Precursors | Amino acids Cleaved from prehormones to prohormones to hormones | Cholesterol |
| Synthesis | Transcription from DNA/RNA | |
| Storage | Secretory Vesicles | Minimal storage Normally mobilised from cholesterol esters in cytoplasm as required |
| Transport | Dissolved in Plasma | Bound to plasma proteins |
| Target | Cell surface receptors | Cytoplasmic and nucleic receptors which results in effectors in the nucleus |
| MOA | Via action of 2nd messenger systems | Bind to DNA and intracellular pathway mRNA and alter transcription |
| Onset | Rapid | Slow |
| Offset | Rapid | Prolonged |
Gladwin 2016
Examiner Comments
2012B 24: 3 (13.7%) of candidates passed.
Most candidates used a table format to present their answer. Most also were able to give examples of peptides and steroids hormone. A common omission was an explanation of the differences in mechanism of action and different mediators. Better answers were able to compare and contrast aspects such as structure, synthesis, precursor, storage, transport and kinetics. Examples of peptide hormones include the anterior and posterior pituitary hormones, Parathyroid hormone, calcitonin, etc. Examples of steroid hormones are the adrenocortical hormones (e.g. glucocorticoid, mineralocorticoids, androgens), sex hormones and 1, 25 di OH vitamin D.
2010B 11
Compare and contrast hydrocortisone, methylprednisolone and dexamethasone.
Examiner Comments
2010B 11: 6 (40%) of candidates passed this question.
Hydrocortisone represents the main endogenous glucorticoid. Methylprednisolone and dexamethasone are synthetic glucocorticoids that all have metabolic, anti – inflammatory and immunosuppressive effects. These are commonly encountered drugs in intensive care practice, yet overall this question was poorly answered. For a good answer candidates were expected to mention the differences in their pharmacokinetics, relative glucocorticoid and mineralcorticoid effects and adverse effects. These drugs share some common features (eg all have a steroid nucleus, hepatic metabolism and renal excretion and adverse effects), features that were poorly covered by the candidates, but also expected to be mentioned for a good answer.
Syllabus: N2,2c
References: Stoelting, Pharmacology and Physiology in Anaesthetic Practice, pge 416, Peck Hill and Williams Pharmacology for Anaesthesia and Intensive Care, pg 355-8
2020B 03 – 2017A 10
Describe the pharmacology of hydrocortisone.
Examiner Comments
2020B 03: 69% of candidates passed this question.
Hydrocortisone is a level 1 drug in the syllabus. Most answers were well structured, many used key headings. In general, detailed information specific to hydrocortisone was lacking. Answers that focused on the mechanism of action, pharmacodynamic effects and pharmacokinetics effects which were detailed and accurate scored well. It was expected that significant detail be included in the sections with relevance to clinical practice for example, the mechanism of action and pharmacodynamic effects including the side effect profile. An indication/appreciation of the timelines of such was also represented in the marking template.
2017A 10: 54% of candidates passed this question.
Hydrocortisone is listed as a Class A drug in the syllabus and as such knowledge of its pharmacokinetics is expected. No marks were awarded for generic pharmacokinetic statements such as: “average bioavailability”, “moderate protein binding”, “bioavailability 100% for IV preparation” etc.
2022B 20
Describe the pharmacokinetics of prednisone (50% marks). List the cardiovascular, renal, metabolic, haematological and immunological effects of prednisone (50% marks)
CICMWrecks Answer
Prednisolone
Pharmacokinetics
- Absorption:
- PO and Rectal
- Rapidly and completely absorbed by both routes – 80–100%.
- Distribution:
- reversibly bound to albumin and a specific corticosteroid-binding globulin
- Protein binding: 80–90% (at low conc), 60-70% (at higher conc.)
- VD: 0.35-0.7 L/kg
- Metabolism:
- liver – hydroxylation with subsequent conjugation.
- Excretion:
- 11–14% unchanged in the urine
- Dose-dependent clearance: 170 to 200 ml/min
- Elimination half-life: 2.6–5 hours
Effects
- CVS
- positive effect on myocardial contractility
- causes vasoconstriction by increasing the number of alpha-1adrenoreceptors and beta-adrenoreceptors and stimulating their function.
- In the absence of corticosteroids, vascular permeability increases; small blood vessels demonstrate an inadequate motor response, and the cardiac output decreases.
- Renal
- weak mineralocorticoid effects and produces sodium retention and increased potassium excretion
- urinary excretion of calcium is also increased
- increases the glomerular filtration rate and stimulates tubular secretory activity.
- Metabolic
- profound effects on carbohydrate, protein, and lipid metabolism.
- stimulates gluconeogenesis and inhibits the peripheral utilization of glucose
- cause a redistribution of body fat, enhance lipolysis, and also reduce the conversion of amino acids to protein.
- Haematological
- increases red blood cell, neutrophil, and haemoglobin concentrations
- depresses other white cell lines and the activity of lymphoid tissue.
- Immunological
- potent anti-inflammatory agent which inhibits all stages of the inflammatory process
- inhibits neutrophil and macrophage recruitment, blocking the effect of lymphokines
- inhibits the formation of plasminogen activator.
- CNS
- increases the excitability of the CNS
- absence of glucocorticoid leads to apathy, depression, and irritability.
- GIT
- increases the likelihood of peptic ulcer disease
- decreases the gastrointestinal absorption of calcium.
Source: Drugs in Anaesthesia and Intensive care 5th Edition
Examiner Comments
2022B 20: 40% of candidates passed this question.
The question asked for detailed information on the pharmacokinetics and selected pharmacodynamics of prednisone. Most candidates provided unnecessary details of the mechanism of action and pharmaceutics significantly wasting time. Many provided incorrect information and general information without specifics which is represented by the low pass rate. The pharmacokinetics part was answered poorly. It was expected from the candidates to have detailed knowledge on the prednisolone binding capacity and affinity to albumin and corticosteroid binding protein as well as the important metabolism of prednisone.
ii. Understand the pharmacology of insulin preparations.
2013B 06
Describe the pharmacology of short acting insulin (actrapid).
Examiner Comments
2013B 06: 13 candidates passed (48.1%).
In general candidates lacked a sufficient depth of knowledge for this commonly used drug. Some candidates confused actrapid with novo rapid. A structured approach (e.g. pharmaceutics, mode of action, pharmacokinetics, etc.) was expected.
iii. Understand the pharmacology of oral hypoglycaemic drugs.
2020B 06
Classify the oral hypoglycaemic drugs (20% marks); include their mechanism of action (40% marks) and their most significant side effects (40% marks).
2013A 06
Classify the oral hypoglycaemic drugs; include their mechanism of action, and their most significant side effects.
CICMWrecks Answer
| Drug class | Mechanism | Side effects |
|---|---|---|
| Biguanides (Metformin) | – Stimulates the movement of GLUT-4 receptors to the membrane of skeletal muscle and adipose tissue cells, increasing glucose uptake by those cells. – Also inhibits gluconeogenesis and glycogenolysis in the liver, and delays intestinal glucose absorption. | – Life threatening lactic acidosis may occur in the presence of renal impairment – Diarrhoea, n/v, abdominal discomfort common – Must be withheld prior to administration of iodinated IV contrast |
| Sulfonylureas (Gliclazide) | – Combine with KATP receptors on pancreatic ß cells, closing the ATP-dependent potassium channels to depolarize the cell, resulting in an influx of calcium which stimulates insulin secretion. | – Risk of hypoglycaemia – GIT disturbance – Stimulate appetite and may cause weight gain |
| Meglitinides (Repaglinide) | – Act by stimulating the same receptor as the sulfonylurea drugs but at a different side. | – Risk of hypoglycaemia – Repaglinide is a major substrate of CYP3A4 and caution should be used when administering with clarithromycin or antifungals, as may result in high plasma levels of repaglinide and consequent severe hypoglycaemia |
| Thiazolidinediones (Rosiglitazone) | – Act on the PPARg in fat cells to induce insulin sensitivity | – Associated with increased risk of peripheral limb fracture in post-menopausal women, and also some cases of diabetic maculopathy. – prone to cause severe fluid retention and precipitate heart failure, contraindicated in CCF – Contraindicated in people with known IHD. |
| Alpha- glucosidase inhibitors (Acarbose) | – Act by inhibit the enzyme that breaks down dietary complex carbs to sugar, reducing the quantity of glucose available for absorption | – Abdominal discomfort & distention, Flatulence – Elevates serum transaminases – Shouldn’t produce hypoglycaemia itself as does not promote insulin release |
| DPP-IV inhibitors (Sitagliptin) | – Inhibit the activity of the enzyme DPP-IV, which normally breaks down the gut hormones GLP-1 (glucagon-like peptide 1) and the protein GIP (gastric inhibitor peptide). GLP-1 and GIP stimulate glucose-mediated insulin release from the pancreas following an oral load of glucose. | – Monitor in renal insufficiency – May cause hypoglycaemia |
| SGLT2 inhibitors (Dapagliflozin) | – Inhibit Sodium-glucose transport protein 2 (SGLT2, which is responsible for reabsorbing glucose in kidney). – Decreased kidney reabsorption of glucose, glucosuria effect (Insulin and pancreatic b cell independent) | – May cause Hypoglycemia – May cause Severe Euglycemic Ketoacidosis, esp in post-op period – UTIs, Candidal Vulvovaginits |
JC 2019
Click to Open CICMWrecks Pharmacopeia Table: Hypoglycaemic Agents
Examiner Comments
2020B 06: 37% of candidates passed this question.
High scoring answers most often started with a strong and logical structure and focused on the requested categories of information. Many candidates gave good answers across the wide range of drugs. Several candidates could have scored more highly by giving more correct information on biguanides and sulphonylureas,
2013A 06:
A good answer would have best been served by a tabular structure and some understanding of the information required. One system of classification of oral hypoglycaemic drugs is by their mechanism of action, or drug group e.g. Biguanides, Sulfonylureas, Thiazolidinediones, Alpha-glucosidase inhibitors, Meglitinides and Dipeptidyl peptidase (DPP) -IV inhibitors.
2024B 10
Outline the mechanisms of action and adverse effects of the following:
(a) Biguanides (35% of marks).
(b) Sodium-Glucose cotransporter – 2 (SGLT-2) inhibitors (SGLT-2) (35% of marks).
(c) Sulfonylureas (30% of marks).
Examiner Comments
2024B 10: 52% of candidates passed this question.
The information required for this question was largely self-explanatory. Higher scoring answers were able to demonstrate understanding by providing some discussion and context with regards to adverse effects rather than a simple list.
iv. Understand the pharmacology of thyroid hormones.
v. Understand the pharmacology of mineralocorticoids.
vi. Outline the pharmacology of glucagon.
vii. Understand the pharmacology of vasopressin and its analogues.
2017A 20
Describe the pharmacology of vasopressin (70% of marks) and its analogues (30% of marks).
2013A 22
Describe the actions of endogenous vasopressin. (60% of marks)
List the vasopressin analogues and their uses. (40% of marks)
Examiner Comments
2017A 20: 28% of candidates passed this question.
A pharmacology answer template outlining pharmacokinetics and dynamics was required. Candidates failed to score marks for describing the physiology of vasopressin secretion. A number of answers demonstrated limited knowledge about its indications for use and its potential adverse effects.
2013A 22:
Overall the first section was not answered in sufficient detail. Aspects such as the antidiuretic effects of vasopressin were often overlooked. Some candidates spent more time on outlining the clinical contexts in which vasopressin is used (which did not score marks), rather than the physiology (which did score marks). DDAVP was the most common analogue mentioned, with the others often being omitted (e.g. terlipressin, ornipressin, etc.).
2023A 20
Compare and contrast the relevant pharmacology of intravenous adrenaline and vasopressin.
Examiner Comments
2023A 20: 20% of candidates passed this question.
The major emphasis of this question and opportunity to score marks reside in “comparing the two drugs” in various aspects – pharmaceutics, indication, mechanism of action, pharmacodynamics, and pharmacokinetics. Although most of the candidates were able to list pharmaceutics, indications, kinetics and dynamics of both the drugs in reasonably structured and tabulated format, many failed to highlight the important commonalities and differences between the two. In mechanism of action, details of the receptor, their location and second messenger system were expected. In pharmacodynamics, similarities and differences in cardiovascular, respiratory, haematological, renal and metabolic effects were needed. There are additional neurological effects and genito-urinary (tocolysis and sphincter tone) of adrenaline which were rarely mentioned. There were frequent significant omissions or incorrect details in the pharmacokinetics sections of both drugs.
2020A 10 – 2011A 23 – 2007B 07
Compare and contrast the pharmacology of Noradrenaline (Norepinephrine) and Vasopressin.
Examiner Comments
2020A 10: 49% of candidates passed this question.
These are both level 1 drugs regularly used in intensive care. Significant depth and detail of each drug were expected. Overall knowledge was deemed to be superficial and lacked integration. Better answers identified key points of difference and overlap in areas such as structure, pharmaceutics, pharmacokinetics, pharmacodynamics, mechanism of action, adverse effects and contraindications. A tabular list of individual drug pharmacological properties alongside each other did not score as well as answers which highlighted key areas of difference and similarities.
2011A 23: 6 (50%) of candidates passed this question.
A straightforward question that was reasonably answered, with most candidates using a methodical tabular approach to explaining the differences in pharmacology between noradrenaline and vasopressin. The benefits of adhering to a wellorganised system of columns showing direct comparisons of the various relevant drug characteristics was clear, with candidates who chose this approach covering most of the necessary information in a clear and comprehensive manner. Some candidates managed to provide a great deal of relevant detail within the allocated time as would be expected in this relatively uncomplicated question. Simple definitions were often lacking and failing to provide this basic introductory information resulted in lower marks for this question. While most candidates were able to discuss the effects of each drug on the cardiovascular system, not as many were able to give outline other physiological effects in sufficient detail. For example, many candidates made little mention of important renal, metabolic and haematological effects. While some candidates discussed pharmacokinetics well, many provided only a very superficial outline of this aspect. The important area of adverse reactions could also have been covered in greater detail.
Syllabus: C2d, 2a and N2, 2f
Recommended sources: Basic and Clinical Pharmacology, Katzung, Chp 9 and 37
2007B 07: 5 candidates (71%) passed this question.
This was best answered using a table. The main points expected for a pass were
- Both are naturally occurring substances
- Direct acting via receptorrs
- Mechanisms by which both increase mean arterial pressure
- Metabolism
- Uses in Intensive Care, septic shock, vasodilatory shock and diabetes insipidus
- Side effects related to intense vasoconstriction and for vasopressin possible coronary ischaemia and sodium and water retention
VIVAs
| 2023B | |
| 2023A | |
| 2022B | |
| 2022A | how are fluctuations in blood sugar minimized between meals, Blood sugar, metabolic responses to insulin |
| 2021B | Adrenal gland physiology, pharmacology |
| 2021A | Glucose storage, physiology, pharmacology |
| 2020B | Thyroid physiology, fate of dietary iodine, beta-blockers |
| 2019B | Glucose metabolism, movement from intestinal lumen to blood |
| 2019A | Thyroid hormone synthesis, pharmacology |
| 2018B | |
| 2018A | insulin and glomerular filtration. |
| 2017B | Endocrine functions of the kidney and renal pharmacology. RAS. |
| 2017A | |
| 2016B | |
| 2016A | blood glucose homeostasis and the pharmacology of insulin |
| 2015B | |
| 2015A | |
| 2014B | |
| 2014A | |
| 2013B | |
| 2013A | physiology of thyroid and the thyroid hormone, anti thyroid drugs |
| 2012B | |
| 2012A | |
| 2011B | What is a hormone? Types, pit, thyroid, T3, T4, PTU |
| 2011A | Glucose regulation, hypoglycamic drugs, insulin, T4 vs T3 |
| 2010B | |
| 2010A | NS, mannitol, properties of fluids, pituitary, ADH |
| 2009B | |
| 2009A | |
| 2008B | Insulin – Physio, Pharm, Refeeding syndrome |
| 2008A | |
| 2007B |

Recent Comments