Syllabus (Fourth Edition, 2023)
Topics
R1: Temperature Physiology
i. Define heat and temperature.
ii. Outline the mechanisms for heat transfer between the body and its environment.
iii. Explain the mechanisms by which normal body temperature is maintained and regulated.
iv. Explain the physiological responses to hypothermia and hyperthermia.
R2: Temperature Measurement
i. Describe the measurement of body temperature.
Topics not covered in previous SAQs
R1: Temperature Physiology
i. Define heat and temperature.
iv. Explain the physiological responses to hypothermia and hyperthermia.
Learning Objectives for the First Part Examination in Intensive Care Medicine
- This will ensure that trainees, tutors, and examiners can work from a common base.
- All examination questions are based around this Syllabus.
- These learning objectives are designed to outline the minimum level of understanding required for each topic.
- The accompanying texts are recommended on the basis that the material contained within them provides sufficient information for trainees to meet the learning objectives.
- Trainees are strongly encouraged to explore the existing and evolving body of knowledge of the Basic Sciences as they apply to Intensive Care Medicine by reading widely.
- For all sections of the syllabus an understanding of normal physiology and physiology at extremes of age, obesity, pregnancy (including foetal) and disease (particularly critical illness) is expected.
- Similarly, for pharmacology, trainees are expected to understand a drug’s pharmacology in these contexts.
- An understanding of potential toxicity and relevant antidotes is also expected.
Definitions
Throughout the document specific wording has been used under the required abilities to indicate the level of knowledge and understanding expected and a glossary of these terms is provided.
Definitions
| Calculate | Work out or estimate using mathematical principles. |
| Classify | Divide into categories; organise, arrange. |
| Compare and contrast | Examine similarities and differences. |
| Define | Give the precise meaning. |
| Describe | Give a detailed account of. |
| Explain | Make plain. |
| Interpret | Explain the meaning or significance. |
| Outline | Provide a summary of the important points. |
| Relate | Show a connection between. |
| Understand | Appreciate the details of; comprehend. |
SAQs
R1: Temperature Physiology
i. Define heat and temperature.
Temperature and Heat
CICMWrecks Answer
Temperature
- A measure of a physical property of a substance that determines the tendency for heat to flow from one object to another → heat energy is transferred from a region of higher temperature to a region of lower temperature
- Units for temperature:
- SI unit → Kelvin (K), which is 1/273.16 of absolute temperature of “triple point of H2O” (where H2O exists in equilibrium as a solid, liquid and gas → occurs at 0.01°C)
- Non-SI unit → Celsius (°C), where 1°C is 1/100th the difference between the
freezing and boiling point of H2O
Heat
- A form of kinetic energy → being a state of “thermal agitation” of molecules in a substance
- Units for heat:
- SI unit → Joules (J)
- Non-SI units → calorie (where 1 calorie = 4.186 J → raises temperature of 1 g of H2O from 14.5°C to 15.5°C); Calorie (where 1 Calorie = 1000 calories = 4186 J)
- Heat can be transferred by:
- Conduction (via collision of molecules through a substance)
- Convection (via bulk flow of fluid (liquid/gas) surrounding the substance)
- Evaporation (via vaporisation of water from a substance’s surface → Nb. Latent heat of vaporisation of H2O is 580 cal/g or 2.4 MJ/kg at 37 °C)
- Radiation (via emission of EMR, often within IR band) → Nb. Unlike other heat transfer mechanisms, this can occur through a vacuum and does not require direct contact
- Heat transfer is dependent on the ambient environment:
- Heat is transferred down its “temperature gradient” (from ↑ to ↓ temperature)
- Relative humidity is vital for determining heat transfer via evaporation (as it establishes a “moisture gradient”)
Specific Heat
- Specific heat of substance is the amount of heat energy required to ↑ temperature of 1 g of substance by 1°C
- SI unit → J/kg (Eg. 4.2 kJ/kg per °C for H2O; 3.6 kJ/kg per °C for body tissue (of which 85% is H2O))
Bianca’s notes
Examiner Comments
Body Temperature
CICMWrecks Answer
Core body temperature
- Refers to deep body temperature of main internal organs (in head, trunk, abdomen) → sites where metabolic activity occur (Ie. heat production)
- Kept constant at 37 +/- 0.4 °C (“Normothermia”) → displays normal variations:
- Diurnal variation – ↑ in evening (37.3°C) and ↓ in early morning (35.8°C)
- Menstrual variation – ↑ 0.5 °C in latter half of cycle
- Variations in core body temperature:
- Normothermia → core body temperature 37 +/- 0.4 °C
- Hypothermia → core body temperature < 36 °C
- Hyperthermia → core body temperature > 37.5 °C
- Body maintains a constant core body temperature at “normothermia” (37 +/- 0.4°C) b/c proteins (esp enzymes) function optimally within a narrow temperature range (35-45 °C), and denature at temperatures > 45 °C
Peripheral body temperature
- Refers to body temperature peripherally (Ie. skin, arms, legs, superficial tissues of core sites) → sites where heat loss occur
- Temperature varies widely → always LESS than core body temperature
Bianca’s notes
Examiner Comments
Not asked before
See R1.iii below for relevant SAQs
ii. Outline the mechanisms for heat transfer between the body and its environment.
2013B 15
Explain the role of the skin.
2007B 06
Explain the role of the skin in maintaining body temperature.
CICMWrecks Answer
Skin
- Largest organ in body ~15% body weight
- Resting blood flow ~500ml/min in 70kg male
- Can increase 30-fold or decrease 10-fold
- Largest barrier between human body and external environment
- Composed of epidermis, dermis and subcutaneous tissue
Role of Skin
- Homeostasis
- Relatively impermeable
- Prevents fluid loss
- Only ~300ml/day lost through skin
- Immunological
- Physical barrier
- Low pH and commensal organisms
- Abundant Antigen Presenting Cells (APC) such as dendritic cells
- Sensory function
- Embedded with nerve endings
- Sensory signals to CNS and spinal reflex arcs
- Touch
- Pain
- Temperature
- Sensory signals to CNS and spinal reflex arcs
- Embedded with nerve endings
- Thermoregulation (SEE BELOW FOR DETAILS)
- Sensory
- C fibres – heat
- A δ fibres – cold
- Effector
- Heat loss
- Occurs via
- Radiation
- Conduction
- Convection
- Evaporation
- Requires transfer of core body heat to skin
- Regulated by AV shunts (glomus body)
- Occurs via
- Heat gain
- Opening of AV shunts prevents loss of core body heat to skin
- Heat loss
- Sensory
- Synthesis of cholecalciferol
- Protection against UV
Role of Skin in Thermoregulation
Sensors:
- Thermoreceptors, on free endings of sensory nerves
- Aδ fibres (myelinated, cold, sense below 38°c)
- C fibres (unmyelinated, warm, sense above 30°c)
- Anterior hypothalamus is sensitive to changes in blood temperature
Controller:
- Hypothalamus
- Maintains temperature around a set temperature
- Influenced by many factors including circadian rhythms, thyroid function and ambient temperature
Effector:
- Heat exchange is due to convection, conduction, radiation and evaporation
- Depends on the direction and size of the gradient between skin and the environment
Skin blood flow:
- Heat loss through radiation and convection
- Increased blood flow to skin increases convection and conduction (blood is warm, if temperature gradient present will lose heat to air at increased rate when more flow)
- Assuming skin temperature is below ambient temperature
- When too cold: Sympathetic outflow from hypothalamus
- Noradrenaline acts on α adrenoreceptors (abundant in skins)
- Constriction of cutaneous precapillary sphincters
- Shunting of blood through arteriovenous shunts, bypassing skin
- Constriction of cutaneous precapillary sphincters
- Noradrenaline acts on α adrenoreceptors (abundant in skins)
- When too warm: Decreased sympathetic outflow
- Cutaneous vasodilation
Sweating:
- Heat lost through evaporation and convection
- Energy of molecules in a liquid is unevenly distributed
- High energy molecules will enter gas phase, be liberated from the liquid
- Lowering the average temperature of the liquid
- Sweat glands in dermis
- Secretion of precursor fluid from the gland
- Ducts ascend through the dermis to exit from the dermis
- Pre-ganglionic sympathetic (cholinergic) innervation
- When too cold, Decreased stimulation
- Fluid moves slowly through duct
- Fluid mostly absorbed, minimal sweat
- When too hot, increased sympathetic stimulation
- Fluid moves quickly through duct
- Fluid not resorbed, lots of sweat
Galwin 2016
Examiner Comments
2013B 15: 13 candidates passed (48.1%).
The skin is the largest organ of the body, accounting for about 15% of the total adult body weight, with a rich, but tightly regulated blood flow. It performs many vital functions, including the protection against external physical, chemical, and biologic threats, the prevention of excess water loss from the body and thermoregulation. It is composed of three principle layers, the epidermis, dermis and subcutaneous tissue, each with their own purpose. In addition candidates were expected to describe those aspects of the skin that play a role in physical protection, immune, sensory, thermoregulatory and water regulation. Candidates lacked a sufficient breath and depth of knowledge in this area and often digressed beyond areas specific to the skin (e.g. thermoregulation not specific to the skin).
2007B 06: 4 candidates (57%) passed this question.
It was expected candidates would describe that the maintenance of body temperature is a balance of heat loss and heat production and outline the seies of controls that are important in this process.
An overview of the reflexes involved was expected with som ecomments on temperature receptors in skin for hot and cold, the hypothalamic integration and then the effector being the skin blood flow (vasodilation / vasoconstriction and A-V shunts).
Answers were expected to include some comment on the fact that heat exchange occurs via radiation / conduction / convection / evaporation and requires a heat gradient and that skin blood changes can facilitate or impair this exchange. Using examples such as; if body needs to loose heat there is vasodilation and sweating often added clarity. Extra credit was given for discussing swet production and the principle and the principle of how that will allow increased heat loss with further credit given for discussing the impact of humidity.
Credit was also given for mentioning piloerection, particularly if candidates went on to explain why this might be useful (even though not really applicable in man).
2016B 20
Describe the mechanisms by which heat is lost from the body (40% of marks). Discuss the importance of each of these in a sedated and intubated adult patient (60% of marks).
2014B 06
List the mechanisms involved in heat production and loss by the body. (80% of marks) Define thermoneutral zone and inter-threshold range. (20% of marks)
CICMWrecks Answer
Definitions
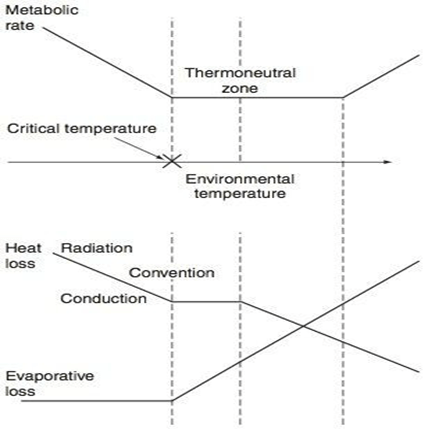
- Thermoneutral zone:
- The range of environmental temperatures in which the metabolic heat production (and oxygen consumption) is minimal and steady and where core temperature is maintained by vasomotor activity alone.
- 25-30 C for a naked, upright man in still air
- Inter-threshold range:
- The range of core temprature over which no autonomic thermoregulatory responses occur
- Normally 0.2 -0.4 °C in a non-anaesthetized state
Mechanisms of Heat production
Total body heat production = Metabolic rate – Total external work
- Metabolism of food to form ATP
- <100% efficient
- Transfer of ATP to functional systems of cells
- <100% efficient
- Basal metabolism of cells
- Muscle contraction
- Overcoming resistance in muscles and other tissues -> friction
- Useful in shivering
- Overcoming resistance in muscles and other tissues -> friction
- Pumping blood
- Overcoming shear forces -> friction
- Breaking chemical bonds
- Flow of ions across membranes
Mechanisms of Heat loss
- Heat is lost by conduction, convection and radiation and evaporation
- The movement of warm blood from the body to skin allows heat loss to the environment
- Conduction:
- Heat transfer occurs due to direct contact to another solid body
- Comprises 3% of total heat loss
- Convection:
- Heat is lost to air via conduction
- This air then moves away, restoring the temperature gradient
- Comprises 15% of total heat loss
- Radiation:
- Heat is emitted from the skin as infrared radiation
- Comprises 60% of total heat loss
- Evaporation:
- There is a distribution of kinetic energies in liquids
- Warmer particles transition to the gas phase, lowering the average temperature of the skin
- Sweat, comprises 22% of total heat loss
Importance in sedated and intubated patient
Radiation:
- Heat loss increased
- if the patient is uncovered and surrounded by cold objects.
- by vasodilatation due to sedative drugs or cholinergics.
- by cool ambient temperature
- in Extracorporeal circuits
- Heat loss Decreased
- by vascoconstriction due to adrenergics
Conduction:
- usually a less important route
- Heat loss increased by use of cold irrigating solutions, and in extracorporeal circuits
Convection:
- Heat loss increased
- if the patient is uncovered
- by cool ambient temperature
- in Extracorporeal circuits
- Heat loss decreased
- Use of Neuromuscular blocking drugs (NMBDs can inhibit shivering, hence decreasing possible convective heat loss via bodily movement)
Evaporation:
- increased if a body cavity is opened, especially if ambient humidity is low.
- Heat loss via evaporation in the trachea and airways may be considerable if inspired gases are not humidified.
- Drugs affecting vascular tone can also alter heat loss by evaporation
Other:
- impaired temperature regulation
- peripheral (e.g. vasodilatation, shivering and impaired piloerection)
- central (central effects of drugs)
- Impairment of neurological or cardiovascular function, or deficiencies of substrate for thermogenesis → alter body’s ability to maintain thermal homeostasis
Mooney / JC 2019
Examiner Comments
2016B 20: 59% of candidates passed this question.
A satisfactory answer required use of terms radiation, convection, conduction etc. in the manner defined in the texts, rather than the layman’s use of the terms. Better answers displayed understanding of the meaning, relative importance and mechanism of methods of heat loss.
The second part of the question required application of these concepts in patients with artificial airway and sedatives, particularly change in control of vascular tone and voluntary behavioural control.
2014B 06: 23% of candidates passed this question.
Many candidates did not read the question carefully and misinterpreted what was being asked. Candidates often digressed into a discussion of thermoregulation. Several candidates wrote about body’s response to cold and heat rather than mechanisms of heat production and loss as was asked.
There was confusion between mechanisms of endogenous heat production and measures to conserve heat. “Behaviour” only attracted marks in relation to voluntary muscle activity for heat production. Changing clothes or seeking a warm environment does not increase heat output by the body. Behaviour can reduce heat loss. Many candidates did not specify ambient or core body temperature.
The definitions of Thermoneutral Zone and Interthreshold Range were not clear. Knowledge generally lacked detail and this was most evident when precise definitions were asked.
iii. Explain the mechanisms by which normal body temperature is maintained and regulated.
2024A 16
(a) Define heat and temperature (15% of marks).
(b) Describe how body temperature is regulated (85% of marks).
2021A 09
Outline the mechanisms by which normal body temperature is maintained and regulated.
2018A 19
Explain the mechanisms by which normal body temperature is maintained and regulated.
CICMWrecks Answer: Definitions
Temperature
- A measure of a physical property of a substance that determines the tendency for heat to flow from one object to another → heat energy is transferred from a region of higher temperature to a region of lower temperature
- Units for temperature:
- SI unit → Kelvin (K), which is 1/273.16 of absolute temperature of “triple point of H2O” (where H2O exists in equilibrium as a solid, liquid and gas → occurs at 0.01°C)
- Non-SI unit → Celsius (°C), where 1°C is 1/100th the difference between the
freezing and boiling point of H2O
Heat
- A form of kinetic energy → being a state of “thermal agitation” of molecules in a substance
- Units for heat:
- SI unit → Joules (J)
- Non-SI units → calorie (where 1 calorie = 4.186 J → raises temperature of 1 g of H2O from 14.5°C to 15.5°C); Calorie (where 1 Calorie = 1000 calories = 4186 J)
- Heat can be transferred by:
- Conduction (via collision of molecules through a substance)
- Convection (via bulk flow of fluid (liquid/gas) surrounding the substance)
- Evaporation (via vaporisation of water from a substance’s surface → Nb. Latent heat of vaporisation of H2O is 580 cal/g or 2.4 MJ/kg at 37 °C)
- Radiation (via emission of EMR, often within IR band) → Nb. Unlike other heat transfer mechanisms, this can occur through a vacuum and does not require direct contact
- Heat transfer is dependent on the ambient environment:
- Heat is transferred down its “temperature gradient” (from ↑ to ↓ temperature)
- Relative humidity is vital for determining heat transfer via evaporation (as it establishes a “moisture gradient”)
Specific Heat
- Specific heat of substance is the amount of heat energy required to ↑ temperature of 1 g of substance by 1°C
- SI unit → J/kg (Eg. 4.2 kJ/kg per °C for H2O; 3.6 kJ/kg per °C for body tissue (of which 85% is H2O))
Bianca’s notes
CICMWrecks Answer: Temperature Regulation
Definitions
- Heat – A form of kinetic energy → being a state of “thermal agitation” of molecules in a substance
- Temperature – A measure of a physical property of a substance that determines the tendency for heat to flow from one object to another → heat energy is transferred from a region of higher temperature to a region of lower temperature
- Temperature setpoint is the level at which the body attempts to maintain its temperature.
- Core body temperature:
- Refers to deep body temperature of main internal organs (in head, trunk, abdomen) →
sites where metabolic activity occur (Ie. heat production) - Kept constant at 37 +/- 0.4 °C (“Normothermia”) → displays normal variations:
- Diurnal variation – ↑ in evening (37.3 °C) and ↓ in early morning (35.8 °C)
- Menstrual variation – ↑ 0.5 °C in latter half of cycle
- Refers to deep body temperature of main internal organs (in head, trunk, abdomen) →
- Variations in core body temperature:
- Normothermia → core body temperature 37 +/- 0.4 °C
- Hypothermia → core body temperature < 36 °C
- Hyperthermia → core body temperature > 37.5 °C
- Peripheral body temperature:
- Refers to body temperature peripherally (Ie. skin, arms, legs, superficial tissues of core
sites) → sites where heat loss occur - Temperature varies widely → always LESS than core body temperature
- Refers to body temperature peripherally (Ie. skin, arms, legs, superficial tissues of core
- Regulation of body temperature is done by balancing heat loss and heat production, predominantly through behavioural mechanisms and skin
Thermoneutral Zone
- The range of environmental temperatures in which the metabolic heat production (and oxygen consumption) is minimal and steady and where core temperature is maintained by vasomotor activity alone.
- 25-30 °C for a naked, upright man in still air
Interthreshold Range
- The range of core temprature over which no autonomic thermoregulatory responses occur
- Normally 0.2 -0.4 °C in a non-anaesthetized state
Regulation of Body Temperature
Temperature sensors are central and peripheral, whilst regulation occurs centrally, and has multiple
effectors
| Cold | Warm | |
|---|---|---|
| Receptor | Bulbs of Krause | Bulbs of Ruffini |
| Afferent nerve type | via Aδ and unmyelinated C sensory fibres | Unmyelinated C fibres |
| Spinal synapse location | Rexed lamina 1,5 | Rexed lamina 1, 2 |
| Ascending tract | Lateral spinothalamic tract in anterior spinal cord | Lateral spinothalamic tract in anterior spinal cord |
| Brainstem synapse | Reticular system of medulla | Reticular system of medulla |
| Central Processor | Hypothalamus (posterior) | Hypothalamus (anterior) |
| Thresholds | No activity at 40 degrees ↑ing activity between 10-27 degrees (remember thermoneutral zone) | Activity with increasing between 30-45 °C Upper threshold limit = 46 °C |
Sensors:
- Central
- Deep tissues/viscera (Eg. in intestinal wall)
- Brain (anterior hypothalamus and extra-hypothalamic areas)
- Spinal cord
- Peripheral
- Dermis (main)
- Corneas
Central Controller:
Hypothalamus is the main body temperature regulatory centre
- Posterior hypothalamus responds to cold
- inputs from peripheral afferents
- responsible for the temperature set point
- ACh is the major neurotransmitter here.
- Anterior hypothalamus responds to heat
- both peripheral input and change in blood temperature
- Major neurotransmitters are Nad, 5HT, dopamine and prostaglandins.
Effector Mechanisms:
- Skin
- Sweating (evaporation)
- Secrete plasma-like fluid Na142, Cl- 104 (urea/K, etc v low amounts) osmolality controlled by rate of secretion and aldosterone
- loss via evaporation (latent heat of vapourisation of water)
- 1-2L in extreme exercise up to 10 L max per 25 hours.
- 0.54 kcal/gram of H2O evaporated
- Degree of evaporation determined by ambient temperature and relative humidity
- Blood Flow (radiation)
- 8 (300 mL/min) – 30% CO skin
- Vasodilation up to 30 fold increase
- Vasoconstriction up to 10 fold decrease
- vasoconstriction/dilation controlled by SNS (α1-mediated) vascular SM contraction and hypothalamic feedback
- Fat/Clothing
- Fat conducts heat 1/3 as readily as other tissues (decreased radiation)
- Clothes reduce conductive heat loss via private zone of air adjacent to skin and decreased convection air currents -50% and more if specialised
- Sweating (evaporation)
- Non-Skin
- Non-shivering thermogenesis
- Predominantly in brown fat
- Uncoupling of oxadative phosphorylation
- Increased heat gain without oxygen consumption/ATP production
- Shivering
- Increased heat gain by metabolism
- Behaviour
- For gain (exercise) or loss (submerging in water)
- Voluntary muscle contraction (Ie. ↑ activity with cold stress; ↓ with hot stress) – Affects heat production
- Body posturing (Ie. ↓ BSA with cold stress;↑ with hot stress) – Affects heat loss
- Clothing (Ie. ↑ clothing with cold stress; ↓ with hot stress) – Affects heat loss
- Appetite
- Cold stress stimulates food-induced thermogenesis → ↑ metabolic rate and heat production
- Thyroid hormone secretion
- Cold stress stimulates thyroid hormone secretion → long-term ↑ metabolic rate and heat production
- Non-shivering thermogenesis
Gladwin / JC 2019
Examiner Comments
2024A 16: 75% of candidates passed this question.
(a) The definition of temperature and heat varies considerably in texts, so reasonable leeway was granted in marking this part.
(b) In this section the following information was expected; body temperature range; thermoneutral zone; sensors (including receptors, fibres, and tracts); central processing (the role of the hypothalamus including anterior and posterior portions); interthreshold range; and a detailed description of the efferent responses for either increasing or decreasing body temperature.
2021A 09: 59% of candidates passed this question.
This question was relatively well answered by most candidates. There was significant variation in the temperatures expressed as normal and few candidates mentioned CORE temperature as a concept. Several candidates gave a detailed description of thermo-neutrality for which there were no marks.
2018A 19: 52% of candidates passed this question.
The best answers were systematic, using a sensor, integrator, effector approach, while also mentioning physiological variations i.e. diurnal, with ovulatory cycle etc.
Few candidates raised the concept of central and peripheral compartments. The differentiation of the concepts of set point, interthreshold range and thermoneutral zone was often confused.
2009A 04
Explain how a normal, healthy adult regulates their body temperature (70% of marks).
Explain how paracetamol exerts an antipyretic effect in a febrile patient (30% of marks).
CICMWrecks Answer: Temperature
Definitions
- Temperature – average kinetic energy of the atoms and molecules that make up a substance
- Temperature setpoint is the level at which the body attempts to maintain its temperature.
- Core body temperature:
- Refers to deep body temperature of main internal organs (in head, trunk, abdomen) →
sites where metabolic activity occur (Ie. heat production) - Kept constant at 37 +/- 0.4 °C (“Normothermia”) → displays normal variations:
- Diurnal variation – ↑ in evening (37.3 °C) and ↓ in early morning (35.8 °C)
- Menstrual variation – ↑ 0.5 °C in latter half of cycle
- Refers to deep body temperature of main internal organs (in head, trunk, abdomen) →
- Variations in core body temperature:
- Normothermia → core body temperature 37 +/- 0.4 °C
- Hypothermia → core body temperature < 36 °C
- Hyperthermia → core body temperature > 37.5 °C
- Peripheral body temperature:
- Refers to body temperature peripherally (Ie. skin, arms, legs, superficial tissues of core
sites) → sites where heat loss occur - Temperature varies widely → always LESS than core body temperature
- Refers to body temperature peripherally (Ie. skin, arms, legs, superficial tissues of core
- Regulation of body temperature is done by balancing heat loss and heat production, predominantly through behavioural mechanisms and skin
Thermoneutral Zone
- The range of environmental temperatures in which the metabolic heat production (and oxygen consumption) is minimal and steady and where core temperature is maintained by vasomotor activity alone.
- 25-30 °C for a naked, upright man in still air
Interthreshold Range
- The range of core temprature over which no autonomic thermoregulatory responses occur
- Normally 0.2 -0.4 °C in a non-anaesthetized state
Regulation of Body Temperature
Temperature sensors are central and peripheral, whilst regulation occurs centrally, and has multiple
effectors
| Cold | Warm | |
|---|---|---|
| Receptor | Bulbs of Krause | Bulbs of Ruffini |
| Afferent nerve type | via Aδ and unmyelinated C sensory fibres | Unmyelinated C fibres |
| Spinal synapse location | Rexed lamina 1,5 | Rexed lamina 1, 2 |
| Ascending tract | Lateral spinothalamic tract in anterior spinal cord | Lateral spinothalamic tract in anterior spinal cord |
| Brainstem synapse | Reticular system of medulla | Reticular system of medulla |
| Central Processor | Hypothalamus (posterior) | Hypothalamus (anterior) |
| Thresholds | No activity at 40 degrees ↑ing activity between 10-27 degrees (remember thermoneutral zone) | Activity with increasing between 30-45 °C Upper threshold limit = 46 °C |
Sensors:
- Central
- Deep tissues/viscera (Eg. in intestinal wall)
- Brain (anterior hypothalamus and extra-hypothalamic areas)
- Spinal cord
- Peripheral
- Dermis (main)
- Corneas
Central Controller:
Hypothalamus is the main body temperature regulatory centre
- Posterior hypothalamus responds to cold
- inputs from peripheral afferents
- responsible for the temperature set point
- ACh is the major neurotransmitter here.
- Anterior hypothalamus responds to heat
- both peripheral input and change in blood temperature
- Major neurotransmitters are Nad, 5HT, dopamine and prostaglandins.
Effector Mechanisms:
- Skin
- Sweating (evaporation)
- Secrete plasma-like fluid Na142, Cl- 104 (urea/K, etc v low amounts) osmolality controlled by rate of secretion and aldosterone
- loss via evaporation (latent heat of vapourisation of water)
- 1-2L in extreme exercise up to 10 L max per 25 hours.
- 0.54 kcal/gram of H2O evaporated
- Degree of evaporation determined by ambient temperature and relative humidity
- Blood Flow (radiation)
- 8 (300 mL/min) – 30% CO skin
- Vasodilation up to 30 fold increase
- Vasoconstriction up to 10 fold decrease
- vasoconstriction/dilation controlled by SNS (α1-mediated) vascular SM contraction and hypothalamic feedback
- Fat/Clothing
- Fat conducts heat 1/3 as readily as other tissues (decreased radiation)
- Clothes reduce conductive heat loss via private zone of air adjacent to skin and decreased convection air currents -50% and more if specialised
- Sweating (evaporation)
- Non-Skin
- Non-shivering thermogenesis
- Predominantly in brown fat
- Uncoupling of oxadative phosphorylation
- Increased heat gain without oxygen consumption/ATP production
- Shivering
- Increased heat gain by metabolism
- Behaviour
- For gain (exercise) or loss (submerging in water)
- Voluntary muscle contraction (Ie. ↑ activity with cold stress; ↓ with hot stress) – Affects heat production
- Body posturing (Ie. ↓ BSA with cold stress;↑ with hot stress) – Affects heat loss
- Clothing (Ie. ↑ clothing with cold stress; ↓ with hot stress) – Affects heat loss
- Appetite
- Cold stress stimulates food-induced thermogenesis → ↑ metabolic rate and heat production
- Thyroid hormone secretion
- Cold stress stimulates thyroid hormone secretion → long-term ↑ metabolic rate and heat production
- Non-shivering thermogenesis
Gladwin / JC 2019
CICMWrecks Answer: Paracetamol Antipyretic effect
Paracetamol antipyresis
- Class: It is an acetanilide derivative used as Analgesic/Antipyretic
- MOA is poorly understood
- Likely via prostaglandin synthesis inhibition, serotonergic and cannabinoid pathways.
- Inhibits COX isoenzymes (COX-1 and COX-2) in areas of low inflammation.
- Inflammation → IL1, IL6, TNF, prostaglandin formation → fever
- Antipyretic Effect
- CNS PG-E synthesis inhibition in anterior hypothalamus
Gladwin / JC 2019
Examiner Comments
2009A 04: Pass rate: 40%
Most candidates mentioned sweating, shivering, vascular response, and behavioural response to cold environment. Outlining the requirements of the temperature sensors, control processing area, and the effectors is, however, essential in order to pass this question. Most candidates did not mention where the temperature sensors are and the possible hormonal response to changes in the temperature of the environment. The interaction between interleukin-1 (and other pyrogens) and prostaglandin production in the hypothalamus was also not discussed.
Syllabus section L1.
Reference: Guyton & Hall 11th Edition page 894-901.
iv. Explain the physiological responses to hypothermia and hyperthermia.
2012A 02
Outline the physiological consequences of therapeutic hypothermia at 32 degrees Celsius
CICMWrecks Answer
Hypothermia:
- Core body temperature < 35 degrees
- Mild: 32-35
- Moderate: 28-32
- Severe: < 28
Effects via system:
- Endocrine and metabolic consequences
- ↓ carbohydrate metabolism and hyperglycaemia
- ↓ drug metabolism and clearance
- ↑ protein catabolic state
- Impaired wound healing (due to catabolic state and wound vasoconstriction)
- ↑ stress response (steroids and catecholamine released)
- Altered Metabolism
- Shivering
- 5x ↑ general MRO2
- ↑hypoxaemia → risk of myocardial and cerebral ischaemia
- In absence of shivering
- general ↓MRO2 (by up to 50%)
- ↓BMR
- Shivering
- Haematological consequences
- ↑ hematocrit and blood viscosity
- Neutropenia and thrombocytopenia
- Coagulopathy and platelet dysfunction
- Respiratory consequences
- ↓ RR and medullary sensitivity to CO2 → ↓ MV (and in severe cases apnoea)
- Left-shift in Hb O2 dissociation curve
- Acid-base changes: alkalosis and hypocapnea
- Rise of pH with falling body temperature
- Fall of PaCO2 with falling body temperature
- Effects on gas solubility
- ↑ oxygen solubility and O2-haemoglobin affinity
- ↑ solubility of gases (incl volatiles)
- V/Q mismatching 2° to inhibition of hypoxic pulmonary vasoconstriction
- Bronchospasm and alterations to deadspace
- Cardiovascular consequences
- ↓ C.O. due to direct –ve inotropic effect of cold and ↑ afterload/SVR
- Tachycardia initially, then progressive bradycardia with ↑ cold
- QT prolongation and the J wave
- Arrhythmias – classically AF and VF
- Resistance to defibrillation
- ↑ SVR and MAP due to peripheral vasoconstriction
- Renal consequences
- “Cold diuresis” due to ↓ vasopressin synthesis
- Central nervous system effects
- Confusion and ↓ level of consciousness
- Shivering
- ↑ seizure threshold
- ↓ CBF
- Immunological consequences
- ↓ granulocyte and monocyte activity
Gladwin 2016
Examiner Comments
2012A 02: 0 (0%) of candidates passed.
It is well documented and often stressed that the Primary Exam is focused upon the basic sciences that underpin clinical Intensive Care. It will examine a candidates understanding of, for example, the physiology associated with a clinical circumstance. Many candidates discussed why we use therapeutic hypothermia after cardiac arrest rather than outline the physiological consequences of hypothermia at 32 degrees Celsius, for which they would not have scored any marks. A good answer was expected to outline changes in metabolism as well as specific organ responses such as cardiovascular (e.g. bradycardia; vasoconstriction; decreased cardiac output, etc), respiratory (decreased minute volume; haemoglobin-oxygen dissociation curve moves left; increased anatomical dead space; diminished HPV; increased pulmonary vascular resistance, etc), renal (e.g. diuresis, changes to GFR, etc) as well as other organs. Again candidates failed to synthesize a coherent and detailed answer.
2015B 02
Describe the consequences of mild hypothermia in the early post-operative setting
2010B 18
Outline the consequences of mild hypothermia in a patient following major surgery
CICMWrecks Answer
- Temperature
- average kinetic energy of the atoms and molecules that make up a substance
- Mild hypothermia
- Temp <35 degrees
- Interthreshold range
- the range of core temperature over which no autonomic thermoregulatory responses occur.
- Under normal conditions: 36.8 ~37.2 degrees
- Under anaesthesia
- Lower threshold decreases 2.5 degrees and upper threshold increases 1.3 degrees
- Therefore decreased ability to maintain core normothermia
Physiology
Cardiovascular system
- Decreased cardiac output
- Peripheral vasoconstriction
- Increased afterload
- Decreased diastolic relaxation
- Decreased preload
- Decreased contractility
- Increased blood viscosity
- Haemoconcentration
- Cold diuresis: Due to decreased responsiveness to ADH and shunting of peripheral blood to central circulation
- Extravasation of intravascular H2O
- Haemoconcentration
- Increased risk of myocardial ischaemia
- Peripheral vasoconstriction
- Coagulopathy
- PT and aPTT increase 9% at 34c compared to 37c
- Increase incidence of atrial arrythmias → ventricular fibrillation at severe hypothermia
- Every degree decrease in temp increases pH 0.015 and decreases pCO2 4.4%
Respiratory
- Initially tachypnoea due to sympathetic stimulation
- Decreased responsiveness to CO2
- Oxyhaemoglobin dissociation curve shifts to left → decreased tissue O2 delivery
CNS
- CMRO2 decreases 7% per 1 degree decrease in core body temperature
GI
- Decreased GI motility
Other
- Post-operative shivering increases total body O2 consumption
- Decreased enzyme activity
- Decreased temperature decreases rate constant in Arrhenius equation
- Decreasesd neutrophil degranulation
- Impaired macrophage phagocytosis
Pharmacology
Pharmacodynamics
- Arrhenius equation for rate constant K
- Where T = temperature
- Therefore as T decreases, the rate constant decreases
- Drug-Receptor interactions are slowed as temperature decreases
- Where T = temperature
Pharmacokinetics
- Decreased absorption of drugs due to delayed gut transit times
- Metabolism of drugs reduced → slow offset of sedative agents given in anaesthesia
- Decreased cardiac output → decreased renal filtration à decreased drug elimination of unchanged drugs → slow offset
- Specific drugs
- Prolonged muscle relaxation from non-depolarizing
- Opioids blunt shivering thermogenesis mechanism → decreased ability to thermoregulate
Sakurai 2016
Examiner Comments
2015B 02: 35% of candidates passed this question.
A well organised answer would provide details on domains of physiology, pharmacology and “other”, such as patient centred effects. Few answers mentioned pharmacology. Providing a definition of “mild” was often overlooked but doing so assisted a focused answer. Many answers spread beyond “mild” hypothermia or address the “causes” rather than the consequence – neither of which gained marks as they were not answering the question asked.
2010B 18: 1 (7%) of candidates passed this question.
This is another very important, and not an infrequently seen, aspect of almost daily intensive care practice which was poorly understood by candidates. For a good answer candidates were expected to outline pharmacological (eg alteration in drug behaviour), physiological (eg shivering, vasoconstriction, impaired coagulation, etc) consequences. Additional points such as poor wound healing, discomfort also attracted a small number of marks. Candidates would have benefited by illustrating their answers with examples, eg prolonged recovery from anaesthesia and duration of neuromuscular blokade.
Syllabus: L2e
References: Hemmings, Foundation of Anaesthesia: Basic and Clinical Science pg 815
2023B 10 – 2022A 16
Outline the impact of sedative agents on thermoregulation (40% marks) and describe the physiological effects of a low body temperature (60% marks).
CICMWrecks Answer
Impact of sedative agents on Thermoregulation
3 phases:
- Phase I – 1st hour – Redistribution of heat from core → periphery
- significant decrease in core temperature from 0.5 to 1.5 C
- thermoregulatory center is depressed by anaesthesia
- Contributors:
- undressed
- skin prep
- evaporative loss
- induction → cutaneous vasodilation
- cool IVF
- cool dry ventilation of lungs
- temp drop in spinal > epidural
- Phase II – Hour 2 to 3 – Slow linear decrease in core temperature
- Increased heat loss
- anaethetic induced peripheral vasodilation
- → increased radiant & evaporative loss.
- → redistribution of heat from core to periphery
- Decreased heat production
- NMBD mean cannot shiver
- anaesthesia means cannot get clothes or eat or curl up.
- Increased heat loss
- Phase III – 3+ hours – Plateau in core temperature
- core temperature plateaus
- peripheral temperature continues to decrease.
Mechanisms of ↓ in core body temperature:
- Resetting of interthreshold range (phase II)
- ↑ width of range to 4 °C → ↓ threshold to cold by 3 °C and ↑ threshold to heat by 1° C → ↓ thermoregulatory responses to Δ in body temperature
- Caused by a central effect → GA agent interferes with normal hypothalamic function to maintain a narrow threshold range
- GA agent-induced vasodilation → redistribution of heat from central to peripheral compartments (phase I)
- Muscle paralysis → loss of shivering response and muscle activity (phase II)
- LOC and paralysis → loss of behavioural responses (phase II)
- GA-induced ↓ BMR/heat production (phase II)
- Cold gases and IVF (phase II) → temp. generally ↓ 0.25-0.5 °C/L of IVF
Physiological effects of low body temperature
| CVS | – Tachycardia initially, then progressive bradycardia with ↑ cold – ↑ cardiac arrhythmias and myocardial ischaemia due to catecholamines released from stress response – ↑ SVR and MAP due to peripheral vasoconstriction – ↓ C.O. due to direct –ve inotropic effect of cold and ↑ afterload/SVR |
| Respiratory | – Left-shift in Hb O2 dissociation curve – V/Q mismatching 2° to inhibition of hypoxic pulmonary vasoconstriction – Bronchospasms – ↓ MV (and in severe cases apnoea) – ↑ solubility of gases (incl volatiles) |
| CNS | – Altered mental state (esp ↑ drowsiness, unconsciousness and delayed awakening from GA) – ↓ CBF |
| Haematological and immunological | – Coagulopathy (due to platelet dysfunction and loss of CF enzyme function) → ↑ transfusion requirements due to bleeding – ↓ WBC activity → ↑ incidence of infections |
| Hepatic / renal | – Impaired renal function (oliguria) – Impaired hepatic metabolic function (esp ↓ drug metabolism, such as muscle relaxants) |
| Metabolic and endocrine | – Impaired wound healing (due to catabolic state and wound vasoconstriction) – ↑ protein catabolic state – ↑ stress response (steroids and catecholamine released) – Shivering → 5x ↑ general MRO2 → causes hypoxaemia (risk of myocardial and cerebral ischaemia) – In absence of shivering → general ↓ MRO2 (by up to 50%) and ↓ BMR |
| Others | – ↑ morbidity and mortality rate (due to above reasons) – Hypothermia may be beneficial during cerebral or cardiac ischaemia as it ↓ metabolic O2 requirements (provided shivering response is blunted) – ↓ anaesthetic requirements (MAC-sparing) – ↓ triggering and severity of MH |
JF / Bianca 2016
Examiner Comments
2023B 10: 66% of candidates passed this question.
The first part of the question required candidates to outline the impact of sedatives on the interthreshold range with an explanation of what this is, how heat is lost, how heat generation is impaired and the mechanism by which these occur (ie. radiation/conduction/convection via vasodilation, with absence of vasoconstriction/heat generation strategies).
The second part of the question required a systems based approach with an outline of the perturbation as a result of the low body temperature. Temperature thresholds for certain physiological effects ie. loss of consciousness or arrhythmia was also expected for an overall thorough answer to this question.
2022A 16: 33% of candidates passed this question.
Sedation reduces body temperature by interfering with heat production and increasing heat loss, along with widening of hypothalamic inter-threshold range. This portion of the question was generally well answered. The question asked to “outline” the answer. Many candidates actually “described” the thermoregulation process in general but were unable to relate those with the impact of sedation. The second part of the question (physiological effect of low body temperature) was answered by most of the candidates with the structure of organ-system wise description. A few candidates scored extra marks by relating these effects with degree of hypothermia and by describing how thermogenesis responses (including shivering) can influence those effects. Some candidates restricted their answers to the effect of thermogenesis in response hypothermia and did not include the overall physiological consequences of low body temperature. Better answers displayed an understanding of core temperature regulation, inter threshold range and the effects of sedatives on thresholds for thermogenic responses, although only a few mentioned gain and maximal response. Better answers included specific detail (mentioned bradyarrhythmia, slow AF, VF, prolonged PR/QRS / J waves rather than just stating arrhythmia) across several organ systems. Marks were not awarded for generic statements such as ‘decreased liver function’ without some additional detail. Inadequate depth of knowledge was main reason behind overall poor scores.
R2: Temperature Measurement
i. Describe the measurement of body temperature.
2016A 19
Describe the methods of temperature measurement.
CICMWrecks Answer
Temperature is the tendency of a body to transfer heat energy to another body, and is measured in degrees.
It is distinct from heat, which is the kinetic energy content of a body, and is measured in Joules. The two are related by the specific heat capacity, which describes how much energy (J) must be applied to a body to raise its temperature from 14°C to 15°C, without a change in state.
Measurement of Temperature
Temperature is measured by a number of methods:
- Liquid Expansion Thermometry
- Electrical methods:
- Resistance thermometry
- Thermistor
- Thermocouple
1. Liquid Expansion Thermometry
This is used in mercury thermometers. These consist of:
- A graduated evacuated capillary of negligible volume, attached to
- A mercury reservoir, of much greater volume, separated by
- A constriction ring
Prevents travel of mercury up the capillary by gravity.
Mechanism:
- When heated, the kinetic energy of the mercury increases and it expands, forcing it up the capillary.
- As the thermal expansion coefficient for all liquids is very small, the capillary must be of a very small volume to create a useable device.
- The speed that this occurs is related to the time-constant of the system
This is typically 30 seconds. Measurement therefore takes ~4 time-constants, or 2 minutes.
Pros
- Easy to use
- Accurate
- Reusable
- Sterilisable
- Cheap
Cons
- Slow response: Only accurate once it has reached thermal equilibrium.
- Glass can break: May cause release of mercury or alcohol.
- Inaccurate at:
- Low temperatures with mercury
Freezes at -38.8°C. - High temperatures with alcohol
Boils at 78.5°C.
- Low temperatures with mercury
2. Electrical
Electrical methods include:
- Resistance thermometer
Platinum wire increases electrical resistance with increasing temperature.- Therefore the voltage drop across the wire will correspond to the temperature of the wire
- Change in resistance is linear across the temperature range
- However, these are expensive.
- Thermistor
Metal (e.g. SiO2) semiconductor which changes its resistance in a predictably non-linear fashion (run-away exponent) with temperature.- Can be manufactured so that change is linear over the clinical range
- Much cheaper than wire resistance methods
- The degree of voltage drop is usually very small, however this can be amplified using a wheatstone bridge
- Thermocouple
At the junction of two dissimilar metals, a potential difference will be produced proportional to their temperature. This is known as the Seebeck effect.- Non-linear (wash in exponent)
- Degrade over time
JC 2019
Examiner Comments
2016A 19: 36% of candidates passed this question.
A good answer included a definition of temperature and a classification of the methods of measuring temperature such as electrical, non-electrical and infrared. There followed a brief description of the physical principles of thermistors, thermocouples and resistance thermometers; mercury and alcohol thermometers, bimetallic strips; and of infrared methods. Candidates who did well reproduced the content of the chapter on temperature measurement in the recommended text book. Candidates who were not familiar with this material attempted to answer the question by falling back on clinical experience of measuring temperature in different sites or occasionally referring to concepts of thermoregulation. Neither approach gained credit.
Some candidates interpreted “methods” incorrectly as “site of measurement” so scored poorly.
VIVAs
| 2023B | Heat and Temperature, Temp Measurement |
| 2023A | |
| 2022B | Temperature, measurement |
| 2022A | |
| 2021B | Temperature, measurement |
| 2021A | |
| 2020B | |
| 2019B | |
| 2019A | |
| 2018B | Heat and Temperature |
| 2018A | |
| 2017B | |
| 2017A | |
| 2016B | |
| 2016A | |
| 2015B | |
| 2015A | |
| 2014B | |
| 2014A | measurement of temperature, physical principles of flow, ionic changes across membranes |
| 2013B | |
| 2013A | |
| 2012B | |
| 2012A | |
| 2011B | |
| 2011A | Body temp control, diurnal variation, thermoneutral zone, differences with neonates, newborns, children, drugs |
| 2010B | |
| 2010A | |
| 2009B | temperature control and measurement |
| 2009A | |
| 2008B | |
| 2008A | |
| 2007B |

Recent Comments