Syllabus (Fourth Edition, 2023)
Topics
O1: Gastrointestinal Physiology
i. Describe the composition, volumes, and regulation of gastrointestinal secretions.
ii. Describe the control of gastrointestinal motility, including (oesophageal) sphincter function.
iii. Outline the digestion and absorption of fat, protein, and carbohydrates.
iv. Outline the absorption of water, electrolytes, and vitamins.
v. Outline the gastrointestinal blood supply.
O2: Gastrointestinal Pharmacology
i. Describe the pharmacology of aperients, laxatives and drugs that affect gastrointestinal motility.
ii. Describe the pharmacology of drugs that influence gastric fluid pH and volume.
iii. Describe the pharmacology of drugs with anti-emetic activity.
iv. Describe the pharmacology of octreotide, vasopressin and terlipressin.
Topics not covered in previous SAQs
O1: Gastrointestinal Physiology
iii. Outline the digestion and absorption of fat, protein, and carbohydrates.
iv. Outline the absorption of water, electrolytes, and vitamins.
Learning Objectives for the First Part Examination in Intensive Care Medicine
- This will ensure that trainees, tutors, and examiners can work from a common base.
- All examination questions are based around this Syllabus.
- These learning objectives are designed to outline the minimum level of understanding required for each topic.
- The accompanying texts are recommended on the basis that the material contained within them provides sufficient information for trainees to meet the learning objectives.
- Trainees are strongly encouraged to explore the existing and evolving body of knowledge of the Basic Sciences as they apply to Intensive Care Medicine by reading widely.
- For all sections of the syllabus an understanding of normal physiology and physiology at extremes of age, obesity, pregnancy (including foetal) and disease (particularly critical illness) is expected.
- Similarly, for pharmacology, trainees are expected to understand a drug’s pharmacology in these contexts.
- An understanding of potential toxicity and relevant antidotes is also expected.
Definitions
Throughout the document specific wording has been used under the required abilities to indicate the level of knowledge and understanding expected and a glossary of these terms is provided.
Definitions
| Calculate | Work out or estimate using mathematical principles. |
| Classify | Divide into categories; organise, arrange. |
| Compare and contrast | Examine similarities and differences. |
| Define | Give the precise meaning. |
| Describe | Give a detailed account of. |
| Explain | Make plain. |
| Interpret | Explain the meaning or significance. |
| Outline | Provide a summary of the important points. |
| Relate | Show a connection between. |
| Understand | Appreciate the details of; comprehend. |
SAQs
O1: Gastrointestinal Physiology
i. Describe the composition, volumes, and regulation of gastrointestinal secretions.
2009A 19
Describe the functions of the gastric secretions.
CICMWrecks Answer
Functions of Gastric Secretions: Gastric Juice
1. Gastric Acid
- Activation of pepsin (from pepsinogen I) → protein digestion
- Facilitates protein digestion by ↓ pH alone
- Defence against micro-organisms
- Facilitates iron absorption in duodenum
- Stimulates biliary/pancreatic juice secretion (via duodenal CCK/secretin)
- –ve feedback on further HCl secretion
2. Pepsinogen
- Pepsinogen undergoes autocatalytic cleavage by acidic pH of stomach → forms pepsin → proteolytic enzyme that aids protein digestion
3. Intrinsic Factor
- glycoprotein that facilitates Vitamin B12 (cobalamin) absorption
4. Mucous in alkaline-rich fluid
- Forms “gastric mucosal barrier” → keeps H+ out of mucosa (prevents autodigestion by HCl → ulceration) and Na+ in it (maintains potential difference across mucosal surface)
- Lubricates food
- Traps bacteria
5. Gastric Lipase and Amylase
- Aid digestion of fats and CHO (minor role only)
Functions of Gastric Secretions: Non-Gastric Juice
1. Gastrin
- ↑ gastric HCl secretion (1500x more potent vs. histamine) → stimulates parietal cells directly and indirectly (via histamine from ECL cells)
- ↑ pepsinogen secretion from chief cells
- +ve trophic effect on small intestinal/colonic mucosa and parietal cell mass
- ↑ gastric and intestinal motility
- ↑ LOS contraction (preventing reflux)
- ↑ GB contractions and pancreatic secretions
2. Histamine
- MAJOR stimulus for gastric HCl secretion → acts via H2R (Gs) on parietal cells
3. Somatostain
- Potent inhibitor of gastric acid secretion (acts directly on parietal cells and indirectly by inhibiting gastrin release from G-cells)
- Inhibiting secretion of most GI hormones (Eg. gastrin, VIP, GIP, secretin)
- Inhibits pancreatic exocrine secretion
- Inhibits gastric motility (including ↓ gastric emptying rate)
- Inhibits gallbladder contraction
- Inhibits intestinal absorption of nutrients
JC 2019
Examiner Comments
2009A 19: Pass rate: 40%
Candidates were expected to list and briefly define the role of the various substances produced and secreted by the stomach. These included the hormones gastrin and somatostatin, the enzymes pepsin, lipase and gelatinase, the electrolytes Na+, K+ and HCO3- , HCl and water, prostaglandins and mucus, and intrinsic factor. For example: HCl secreted by parietal cells to produce a very acidic environment pH 1-3.5. This optimizes proteolytic activity of pepsin, has a direct proteolytic role, aids ferric iron conversion to the more soluble ferrous ion, and is important for bactericidal activity and innate immunity. It also stimulates pancreatic and biliary secretions.
Good answers divided the functions into digestive, hormonal, mucosal protection, immunity etc. Marks were not gained for mention of the secretions of other GIT organs.
SyllabusQ12b
Reference: Guyton and Hall 11th edition p791-799
2020B 16
Describe the formation of gastric acid (50% marks) and the regulation of gastric acid secretion (50% marks).
CICMWrecks Answer
Volume and composition of gastric juice:
- 2-2.5 L/day of gastric juice is produced
- It contains:
- H2O and electrolytes (> 99.5%)
- Gastric juice is slightly hyperosmotic (325 mOsm/L) with ↑ H+ (150-170 mmol/L), ↑ Cl- (190 mmol/L), and ↑ K+ (10 mmol/L), but ↓ Na+ (2-4 mmol/L) → cf. plasma
- It is also more acidic (pH 1-1.5) → due to ↑ H+ content
- Solid material (< 0.5%)
- Digestive enzymes – Pepsin, Gastric lipase, Gastric amylase
- Mucous in alkaline fluid (HCO3 – -rich)
- Intrinsic factor
- H2O and electrolytes (> 99.5%)
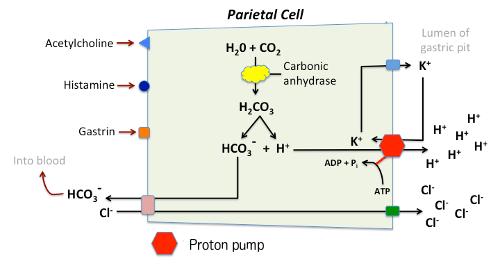
Gastric Acid Secretion:
Parietal cells contain an H+-K+ ATPase (exchange) pump – GPCR – cAMP dependent
- This pump is activated in response to increased levels of intracellular Ca2+ from stimulation by:
- ACh
- Histamine (H2)
- Gastrin
- Inhibited by:
- Low gastric pH
- Somatostatin
Process:
- H+ is produced by action of carbonic anhydrase on CO2 and water, with ‘waste’ HCO3– removed from the cell in exchange for Cl–.
- Respiratory quotient of the stomach may become negative due to consumption of CO2
- HCO3– :
- transported out of the basolateral membrane in exchange for chloride.
- Outflow into blood results in a slight elevation of blood pH known as the “alkaline tide”. This process serves to maintain intracellular pH in the parietal cell.
- Chloride and potassium ions are transported into the lumen of the cannaliculus by conductance channels, and such is necessary for secretion of acid.
- Hydrogen ion is pumped out of the cell, into the lumen, in exchange for potassium through the action of the proton pump; potassium is thus effectively recycled.
Regulation of gastric juice secretion:
- Cephalic phase → 50% of gastric juice secretions
- Initiated by thought, sight, taste and smell of food
- Mediated via vagal (ACh) outflow
- Gastric phase → ~ 50% of gastric juice secretions (prolonged secretion at a slower rate)
- Initiated by entry of food into stomach
- Mediated by – (i) Local and vago-vagal reflexes → due to distension of body (of stomach), and (ii) Gastrin release from G-cells → due to antral distension
- Intestinal phase → < 1% gastric juice secretion
- Initiated by chyme entering duodenum
- Mediated by enterogastric neural (ANS/ENS) and hormonal (CCK, VIP, GIP, Etc.) reflexes
JC 2019
Examiner Comments
2020B 16: 26% of candidates passed this question.
The is question was divided into two sections offering equal marks. The first section required a description of the generation and transport of both H+ and Cl into the stomach lumen by the parietal cell. The contributions of basolateral and luminal ion channels, the role of carbonic anhydrase and accurate description of the net flux was expected for full marks. The second section required comments on the roles of neural and endocrine regulation. Increased acid secretion via acetylcholine (via muscarinic M3), histamine (via H2) and gastrin were expected as was reduced secretion via secretin and somatostatin. Better responses were able to combine and integrate these into cephalic, gastric, and intestinal phases. The nature and function of other gastric secretions and the role of pharmacologic agents was not asked for and therefore not awarded any marks.
2024B 05 – 2019B 13
Describe the exocrine functions of the pancreas.
CICMWrecks Answer
Exocrine pancreas
- produces 1.5L/day pancreatic juice
- Pancreatic juice – digestive enzymes and bicarbonate
- Enzymes: synthesized and secreted from the exocrine acinar cells
- Bicarbonate: secreted from epithelial cells lining small pancreatic ducts
Contents
- Digestive Enzymes:
- Proteases: trypsin and chymotrypsin: proteolysis
- Pancreatic Lipase: Hydrolysis of triglycerides
- Amylase: Hydrolysis of carbohydrates
- Other Pancreatic Enzymes: Ribonuclease, deoxyribonuclease, gelatinase and elastase
- Bicarbonate and water:
- Bicarbonate neutralizes acid coming into small intestine from stomach
- Produced by carbonic anhydrase → secreted into the lumen of the duct → pancreatic juice
Control of pancreatic exocrine secretions
- Vagus nerve:
- Low level stimulus via Ach in response to anticipation of meal
- Enteric endocrine system:
- Cholecystokinin:
- secreted in duodenum
- Stimulated by partially digested proteins and fats
- CCK released into blood → binds to pancr acinar cells
- secreted in duodenum
- Secretin:
- Secreted in proximal small intestine
- In response to acid in duodenum
- Stimulates duct cells to secrete water and bicarb
- Secreted in proximal small intestine
- Gastrin:
- Secreted by stomach
- in response to gastric distension and irritation
- Stimulates acinar cells to secrete digestive enzymes
- Secreted by stomach
- Cholecystokinin:
Occurs in three phases: cephalic → Gastric → Intestinal
JC 2019
Examiner Comments
2024B 05: 42% of candidates passed this question.
Unfortunately, this question had an error in the wording. It should have read “Describe the exocrine secretions of the pancreas including their function and regulation”. This error was considered during marking. Despite this most candidates realised that the functions of the exocrine pancreas are secretory and went onto to provide an overview of the exocrine pancreatic cells and their secretions including the usual volume per day. Expected information included descriptions of the digestive enzymes and their role in protein, fat and CHO digestion and a description of bicarbonate formation and its functions including stomach acid neutralisation and optimisation of pH for enzyme function. Regulation of secretion was best described using the structure of digestive phases; cephalic, gastric and intestinal and the events linked to each. Extra detail on the hormonal and PNS factors, their effects and how they’re stimulated elevated the answer.
2019B 13: 33% of candidates passed this question.
Most candidates were able to mention some pancreatic enzymes, though often in insufficient detail to attract full marks. The amount, type, pH, etc. of pancreatic secretions was often not included. Many candidates did not describe the stimuli for pancreatic secretion. Better answers described the cephalic, gastric and intestinal phases of pancreatic secretion.
2023A 06
Describe pancreatic secretions and their regulation.
CICMWrecks Answer
Pancreatic Secretions
| EXOCRINE SECRETIONS | HCO3– | |
| Water | ||
| Enzymes | Proteases | |
| Amylase | ||
| Lipase | ||
| Others | ||
| ENDOCRINE SECRETIONS | Insulin | |
| Glucagon | ||
| Somatostatin | ||
Pancreas: Exocrine Secretions
Contents
- Digestive Enzymes:
- Proteases: trypsin and chymotrypsin: proteolysis
- Pancreatic Lipase: Hydrolysis of triglycerides
- Amylase: Hydrolysis of carbohydrates
- Other Pancreatic Enzymes: Ribonuclease, deoxyribonuclease, gelatinase and elastase
- Bicarbonate and water:
- Bicarbonate neutralizes acid coming into small intestine from stomach
- Produced by carbonic anhydrase → secreted into the lumen of the duct → pancreatic juice
Control of pancreatic exocrine secretions
- Vagus nerve:
- Low level stimulus via Ach in response to anticipation of meal
- Enteric endocrine system:
- Cholecystokinin:
- secreted in duodenum
- Stimulated by partially digested proteins and fats
- CCK released into blood → binds to pancr acinar cells
- secreted in duodenum
- Secretin:
- Secreted in proximal small intestine
- In response to acid in duodenum
- Stimulates duct cells to secrete water and bicarb
- Secreted in proximal small intestine
- Gastrin:
- Secreted by stomach
- in response to gastric distension and irritation
- Stimulates acinar cells to secrete digestive enzymes
- Secreted by stomach
- Cholecystokinin:
Occurs in three phases: cephalic → Gastric → Intestinal
Pancreas: Endocrine Secretions
Insulin
- Peptide hormone produced in beta cells of Islets of Langerhans in pancreas
- Proinsulin: insulin precursor; A + B chain joined by 2 disulphide bridges + C peptide
- Insulin: formed when C peptide is cleaved by endopeptidases → insulin + free C peptide are packaged in vesicles
- Exocytosis:
- Primary trigger = ↑BSL
o ↑BSL → ↑facilitated diffusion of glucose through GLUT2 transmembrane channels into B-islet cells → ↑metabolic activity of cell → ↑formation of ATP - ATP-gated K channels on beta islet cell membrane are closed by ↑ATP levels → ↓ K flux → membrane depolarisation → triggers opening of voltage gated Ca2+ channels → Ca2+ influx triggers insulin containing vesicle exocytosis
- Primary trigger = ↑BSL
- Plasma insulin secretion occurs in 2 phases
- ↑BSL → rapid ↑insulin concentration as vesicles with pre-formed insulin empty contents
- When all vesicles have emptied → B islet cells release insulin as it is synthesised
- Physiological effects:
- Facilitation of glucose uptake: GLUT4 in adipose tissue, skeletal muscle, heart – require insulin to facilitate cellular glucose uptake. NB brain has GLUT-1 and liver has GLUT-2 which are not insulin dependent
- Storage of metabolic substrates: hepatic glycogenesis, FA synthesis in liver, ↑esterification of FAs (to make TGs) in adipose tissue
- Inhibition of endogenous glucose production: insulin inhibits lipolysis + glycogenolysis + gluconeogenesis
- Cellular uptake of amino acids and K
- ↑amino acid uptake → promotes protein synthesis
- ↑K uptake: prevents hyperkalaemia following meal
Glucagon
- peptide hormone produced by alpha cells of islets of Langerhans
- unlike insulin, the have no glucose sensing apparatus
- Secretion:
- stimulated by hypoglycaemia: hypoglycaemia-induced ↑ANS activity (i.e. indirect) + ↑adrenaline
- inhibited by: insulin, somatostatin, ↑freeFA and ketone body concentrations
- Actions: ↑plasma glucose conc by: promoting gluconeogenesis+glycogenolysis, inhibits glycolysis in liver. Important during starvation
Somatostatin
- secreted by delta cells in pancreatic islets (and pyloric antrum, duodenum)
- inhibitory hormone
- Stimuli for release: (i) ↑ plasma levels of glucose, a.a. and FA, and (ii) Acidic gastric environment
- inhibited by vagus nerve
- Effects:
- ↓ secretion of pancreatic hormones (insulin, glucagon, pancreatic polypeptide)
- ↓ GH release from pituitary
- ↓ gastric, duodenal and GB motility
- ↓ secretion and absorption in GIT (Eg. gastric acid secretion)
Pancreatic polypeptide
- Polypeptide secreted by F-cells of Islets of Langerhans
- influence GIT function (Ie. ↑enzyme secretion, ↓ intestinal motility, Etc.)
Examiner Comments
2023A 06: 21% of candidates passed this question.
It was vital to recognise and describe both the exocrine and endocrine secretions of the pancreas and their regulation. Insulin, glucagon, and somatostatin are all secreted from the pancreas and their omission was the most common reason for not passing this question. Many candidates unfortunately wrote solely on exocrine secretions. Satisfactory answers provided a moderate amount of detail on both the endocrine (insulin, glucagon and somatostatin) and exocrine (bicarbonate and digestive enzymes; trypsin/chymotrypsin, pancreatic amylase and lipase) secretions of the pancreas including what determines their secretion.
2015A 06
Outline the physiology of pancreatic secretion (80% of marks)
and outline the pharmacology of octreotide (20% of marks)
CICMWrecks Answer: Pancreas Secretions
Pancreatic Secretion
| EXOCRINE SECRETIONS | HCO3– | |
| Water | ||
| Enzymes | Proteases | |
| Amylase | ||
| Lipase | ||
| Others | ||
| ENDOCRINE SECRETIONS | Insulin | |
| Glucagon | ||
| Somatostatin | ||
Exocrine Secretions
- produced by acinar and ductal cells
- ~1.5L per day
- HCO3–
- alkalinize gastric contents
- enzyme carbonic anhydrase
- Water
- Enzymes
- Proteases: Trypsinogen → Trypsin (by enterokinase in gut), Chymotrypsinogen → Chymotrypsin. Proteolysis.
- Amylase: Hydrolysis of glycogen, starch, and complex carbohydrate.
- Lipase: Hydrolysis of dietary triglycerides.
- Others: ribonuclease, deoxyribonuclease, gelatinase and elastase
Endocrine Secretions
- Insulin
- polypeptide hormone
- synthesized from proinsulin in RER of B cells in Islets of Langerhans
- Excreted via exocytosis in response to ↑intracellulae Ca2+
- Minimal protein binding, tiny Vd 0.075 L/kg
- Metabolized in liver, muscle, kidney byt Glutathione insulin transhydrogenase
- Renal elimination of inactive metabolites
- Circulatory hald life ~5mins
- Increased anabolism, decreased catabolism
- maintains normal blood glucose levels by facilitating cellular glucose uptake, regulating carbohydrate, lipid and protein metabolism
- promotes cell division and growth through its mitogenic effects
- Glucagon
- polypeptide hormone
- synthesized in pancreatic A cells
- secreted into portal vein
- Circulating half life ~5mins
- Metabolized in liver (1st pass) – low circulating level
- Glycogenolysis, gluconeogenesis, glucose release, ketone formation
- Lipolysis
- Inotopy, increases metabolic rate
- Stimulates somatostatin, insulin release
- Somatostatin
- polypeptide hormone
- Inhibits Glucagon, Insulin, other pancreatic peptides
- may function as CNS neurotransmitter
CICMWrecks Answer: Pharmacology of Octreotide
Pharmacology of Octreotide
Examiner Comments
2015A 06: 38 % of candidates passed this question.
An outline of exocrine function should have included the sources of secretions, secretions involved in the digestion of proteins, carbohydrates and fats, the roles of trypsin inhibitors and bicarbonate secretion and the regulation of enzyme and bicarbonate secretion.” Knowledge of endocrine physiology was good whereas the depth of knowledge regarding exocrine function was generally shallow with many errors.
Only some general facts around the pharmacology of octreotide were required to pass this section of the question. Responses revealed limited knowledge and contained many errors.
ii. Describe the control of gastrointestinal motility, including (oesophageal) sphincter function.
2018B 08
Describe gastric emptying (40% of marks) and outline its regulation (60% of marks).
2014B 24 – 2010B 21 – 2007B 10
Describe the control of gastric emptying.
CICMWrecks Answer
Physiology of Gastric Emptying
Gastric emptying
- Fluids have half-time of 30mins in stomach
- Solids have half-time of 2 hours in stomach
Gastric receipt of food bolus:
- Peristaltic wave moves down the oesophagus, propelling food bolus
- Controlled by mesenteric plexus with input from vagus nerve
- Upon swallowing, the lower oesophageal sphincter and stomach relax until the oesophageal peristaltic wave has passed
- Following food bolus passage, the LOS tone increases to prevent reflux
- Food bolus reaching the stomach causes a vagal-mediated relaxation of the stomach, to accommodate gastric distension and food storage
Gastric mixing and emptying:
- Spontaneous mixing waves move down the stomach every 15-20 seconds
- Stronger waves propel gastric contents towards the pylorus (pyloric pump)
- High pyloric sphincter tone
- Allows through well-mixed liquid chyme
- Restricting gastric emptying of solids, causing mixing (retropulsion)
Control
Gastric emptying is controlled by the balance between stimulatory gastric factors and inhibitory duodenal factors
Factors promoting gastric emptying:
- Increased stomach wall stretch
- Stimulates pyloric pump
- Reduces pyloric tone
- Parasympathetic vagal stimulation
- Stimulates pyloric pump
- Gastrin
- Stimulates pyloric pump
- From G cells in antrum
- In response to presence of protein (esp. meat) in stomach
- Motilin
- Stimulates pyloric pump
- During fasting
- Stimulates pyloric pump
- From M cells in duodenum (external antigen stimulus)
- Carbohydrate: rapid emptying
Factors inhibiting gastric emptying:
- Nervous reflexes via enteric nervous system, local sympathetic trunk, and the vagal nerve to the brainstem
- in response to local conditions in the duodenum: Distension, Irritation, Acidity of chyme, Hyper- or hypo- tonicity of chyme, Breakdown products, Especially AA and FA
- Inhibit pyloric pump
- Increase pyloric sphincter tone
- Hormones (inhibit pyloric pump)
- Cholecystokinin (CCK)
- From I cells of duodenum
- In response to presence of fat and proteins
- Secretin
- From S cells of duodenum
- In response to presence of acids
- Gastric inhibitory peptide (GIP)
- From K cells of duodenum
- In response to presence of fats, proteins and carbohydrate
- Cholecystokinin (CCK)
- Other Factors :
- Sympathetic stimulus:
- Decreases contractility and reduces gastric emptying
- Dopamine:
- Decreases intragastric pressure and lower oesophageal sphincter tone
- reduces gastric emptying
- Sympathetic stimulus:
Alternate: This section can also be approached as:
- Local factors
- Gastric Factors: pump, Stomach wall distension, Amino acid
- Duodenal Factors: Type of food, stretch of wall, irritation, hyperosmolaroty, acidity, amino acid and FA content
- Neural factors
- Symptathetic
- Parasympathetic
- Hormonal factors
- Dopamine
- Gastrin
- Motilin
- Secretin
- CCK
- Somatostatin
- GIP
Mooney / Sakurai / JC 2019
Examiner Comments
2018B 08: 24% of candidates passed this question.
Candidates were required to provide a description of gastric emptying (40% marks). Although the question showed the allocation of marks, many candidates did not provide sufficient detail for this section. This required some description of what gastric emptying is (the co-ordinated emptying of chyme from the stomach into the duodenum).
Better answers provided detail regarding the process of gastric emptying in the fed and fasted state and differentiated between liquids, solids, carbohydrate, protein and fats. Factors regulating emptying included an outline of peristaltic waves, the basal electrical rhythm and its modulation, the migratory motor complex (MMC) and its modulation, neural input, stretch and hormonal control.
Many candidates erred by answering the question “the regulation of gastric secretions” rather than the question (the regulation of gastric emptying). Although they scored well for hormonal control, they missed out on marks for the other factors relevant to the regulation of gastric emptying.
2014B 24: 23% of candidates passed this question.
An understanding of the physiology of gastric emptying has direct relevance to intensive care practice as it influences enteral feed tolerance, helps inform regarding risk of aspiration and has important pharmacologic implications.
Candidates’ answers were superficial and the role of intrinsic reflexes and local hormonal responses poorly understood and described. A simple and clear coverage is provided in Principles of Physiology for the Anaesthetist / P. Kam, I. Power – 3rd Ed.
2010B 21: 8 (53%) of candidates passed this question.
This was another important, relevant and essential aspect of basic physiology, for which candidates tended to lack sufficient breath and depth of the required knowledge. For a good answer candidates were expected to mention liquids empty much faster (and in an exponential fashion) than solids (which have a linear pattern), rate of emptying depends on the pressure gradient generated by the antrum against pyloric resistance. Antral pump activity is of most importance and that it is influenced by signals from both the stomach (eg distension) and the duodenum (volume, osmolarity, pH) and humoral factors (gastrin, cholecystikinin, secretin) and nervous stimulation (general parasympathetic nervous stimulation enhances gastric motility and sympathetic stimulation opposes it).
Syllabus: Q2d
References: Guyton and Hall Textbook of Medical Physiology, Chp 63, Power and Kam, Principles of Physiology for the Anaesthetists, pg 193
2007B 10: 2 candidate (28%) passed this question.
The main points expected for a pass were
- An appreciation that the aim of controlling gastric emptying is to present the food to the small bowel for absorption in a controlled manner
- That there are both gastric neural and hormonal mechanisms e.g. Gastric volume and the hormone gastrin
- There are duodenal neural and hormonal mechanisms e.g. composition of the chyme, secretin and cholecystokinin and the influence of duodenal distension
- Extra points were given for mentioning the effect of sympathetic stimulation and pregnancy on gastric emptying
Common problems were not enough knowledge, naming hormones but not saying what theirs action was and including drugs.
2012B 08
Describe the physiology of gastric emptying (80% of marks).
Outline the gastrointestinal effects of erythromycin (20% of marks)
CICMWrecks Answer: Gastric Emptying
Physiology of Gastric Emptying
Gastric emptying
- Fluids have half-time of 30mins in stomach
- Solids have half-time of 2 hours in stomach
Gastric receipt of food bolus:
- Peristaltic wave moves down the oesophagus, propelling food bolus
- Controlled by mesenteric plexus with input from vagus nerve
- Upon swallowing, the lower oesophageal sphincter and stomach relax until the oesophageal peristaltic wave has passed
- Following food bolus passage, the LOS tone increases to prevent reflux
- Food bolus reaching the stomach causes a vagal-mediated relaxation of the stomach, to accommodate gastric distension and food storage
Gastric mixing and emptying:
- Spontaneous mixing waves move down the stomach every 15-20 seconds
- Stronger waves propel gastric contents towards the pylorus (pyloric pump)
- High pyloric sphincter tone
- Allows through well-mixed liquid chyme
- Restricting gastric emptying of solids, causing mixing (retropulsion)
Control
Gastric emptying is controlled by the balance between stimulatory gastric factors and inhibitory duodenal factors
Factors promoting gastric emptying:
- Increased stomach wall stretch
- Stimulates pyloric pump
- Reduces pyloric tone
- Parasympathetic vagal stimulation
- Stimulates pyloric pump
- Gastrin
- Stimulates pyloric pump
- From G cells in antrum
- In response to presence of protein (esp. meat) in stomach
- Motilin
- Stimulates pyloric pump
- During fasting
- Stimulates pyloric pump
- From M cells in duodenum (external antigen stimulus)
- Carbohydrate: rapid emptying
Factors inhibiting gastric emptying:
- Nervous reflexes via enteric nervous system, local sympathetic trunk, and the vagal nerve to the brainstem
- in response to local conditions in the duodenum: Distension, Irritation, Acidity of chyme, Hyper- or hypo- tonicity of chyme, Breakdown products, Especially AA and FA
- Inhibit pyloric pump
- Increase pyloric sphincter tone
- Hormones (inhibit pyloric pump)
- Cholecystokinin (CCK)
- From I cells of duodenum
- In response to presence of fat and proteins
- Secretin
- From S cells of duodenum
- In response to presence of acids
- Gastric inhibitory peptide (GIP)
- From K cells of duodenum
- In response to presence of fats, proteins and carbohydrate
- Cholecystokinin (CCK)
- Other Factors :
- Sympathetic stimulus:
- Decreases contractility and reduces gastric emptying
- Dopamine:
- Decreases intragastric pressure and lower oesophageal sphincter tone
- reduces gastric emptying
- Sympathetic stimulus:
Alternate: This section can also be approached as:
- Local factors
- Gastric Factors: pump, Stomach wall distension, Amino acid
- Duodenal Factors: Type of food, stretch of wall, irritation, hyperosmolaroty, acidity, amino acid and FA content
- Neural factors
- Symptathetic
- Parasympathetic
- Hormonal factors
- Dopamine
- Gastrin
- Motilin
- Secretin
- CCK
- Somatostatin
- GIP
Mooney / Sakurai / JC 2019
CICMWrecks Answer: GI Effects of Erythromycin
Erythromycin
- Action:
- Agonist at motilin receptors on GI muscle
- Enchances motilin release from M cells in duodenum
- Promotes onset, frequency and duration of migrating motor complex
- Increases lower oesophageal tone
- May eliminate normal gut flora
Examiner Comments
2012B 08: 9 (41%) of candidates passed.
This question was best answered by using a classification system, or systematic approach to gastric emptying. Receptive relaxation (triggered by movement of food through the pharynx and oesophagus), vagally mediated relaxation of fundus and upper body of stomach, the pyloric pump (being intense peristalsis in lower body of the stomach that results in stomach emptying) and the pyloric sphincter (a circular muscle that allows water and fluids to easily pass through but restricts solids until it is mixed in chime to almost fluid consistency).
Candidates were also expected to mention regulatory factors e.g. food volume through myenteric reflexes / gastrin stimulatory motor effects and enhanced pyloric pump, acidity and osmolality of chyme in duodenum, presence of breakdown products of protein and fat through enteric nervous system, sympathetic and parasympathetic nervous systems and hormones such as cholecystokinin, secretin and gastric inhibitory peptide. Erythromycin is a commonly used prokinetic and some knowledge of effects was expected (e.g. the fact that it stimulates motilin receptors on GI smooth muscle and promote onset, frequency and duration of migrating motor complex, from stomach and spreading caudally thus increasing gastric emptying).
2011B 08
Explain the physiological factors that prevent gastro-oesophageal reflux.
CICMWrecks Answer
- Main barrier to reflux is the lower oesophageal sphincter (LOS).
- Sphincter pressure maintained at 15-25 mmHg > gastric pressure.
- Factor which maintain sphincter pressure are Anatomical, neurological and hormonal.
Anatomical factors which Minimse GOR:
- Functional anatomy of LOS
- Internal (Circular SM) and external sphincters (in continuity with diaphragm)
- Small portion of distal oesophagus is intra-abdominal
- ↑ Intra-abdominal pressure → ↑ distal LOS pressure → ↑ LOS barrier pressure
Neuronal factors which minimise GOR:
- Vagal (ACh) outflow
- Contracts the ”internal sphincter”
- ↑ circular SM tone → ↑ LOS pressure → ↑ LOS barrier pressure
- Phrenic nerve stimulation
- Contracts ”external sphincter” via ”pinch-cock” mechanism
- ↑ LOS pressure → ↑ LOS barrier pressure
Hormonal Factors which limit GOR:
- ↑ LOS tone → ↑ LOS barrier pressure
- Gastrin, CCK, motilin, α-adrenergic stimulation
- ↓ LOS tone → ↓ LOS barrier pressure
- Secretin, VIP, GIP, glucagon, progesterone, and prostaglandins
Gladwin 2016
Examiner Comments
2011B 08: 3 (12%) of candidates passed this question.
For a good answer candidates were expected to give a description of the lower oesophageal sphincter (the intrinsic and extrinsic sphincters and flap-valve), that it maintains a resting pressure of 15-25 mmHg above gastric pressure which prevents gastro-oesophageal reflux, which relaxes after swallowing, that the resting tone is maintained by myogenic and neurogenic mechanisms and the effects of hormones upon the sphincter (ie gastrin, motilin and α adrenergic stimulation increases and secretin, glucagon, VIP and GIP decrease tone).
Syllabus: Q1 2f
Recommended sources: Ganong Review of Medical Physiology Chp 26.
2010A 22
Describe the physiology of vomiting.
CICMWrecks Answer
Physiology of Vomiting
Vomiting
- Involuntary, forceful and rapid expulsion of gastric contents through the mouth
Triggers
- Excessive GI tract distension
- Stimulation of CTZ
- Directly by certain drugs eg apomorphine, morphin
- Rhythmic motion of the body stimulating the vestibular labyrinth of the inner ear
- Cerebral excitation secondary to odours, pain, stress
Central control of vomiting
- Vomiting center (5HT3, NK1, Muscarinic and Histamine), near NTS
- Inputs
- Chemoreceptor trigger zone (NK1, 5HT3, Dopamine), area postrema outside BBB
- Vestibular system (Histamine and Muscarinic) via CNVIII
- GI Tract (5HT3, stretch and chemoreceptors) via vagal
- Higher centres
- Efferent arc
- via CN V,VII,IX,X,XII and spinal nerves to abdominal wall musles and diaphragm
- Inputs
| Afferent signal | Sensor | Efferent signal | Effect |
|---|---|---|---|
| Chemo/ baroreceptor input Drugs Stim from NTS Stim from GIT (5HT3) | CTZ (area postrema) | 5HT3, D2 and Opioid neurons | Direct stimulation of vomit centre in lateral reticular formation |
| Surgery/ Rhythmic motions | Labyrinths | ACh and H1 neurons | |
| Memory/ Emotions Sensory (sight, smell, taste) | Cortex | ||
| Severe painful stimuli | Pain | H1 neurones | |
| Irritation Manipulation during surgery Distension | GIT | NK1, NAdr, ACh neurons | |
| Via CNX, to NTS | Stimulation of CTZ then Vomit centre | ||
| Via 5HT3 to CTZ | CTZ to vomit centre | ||
| Manipulation of pharynx via CN9 to.. | NTS | Direct to CTZ | To vomit centre |
Vomiting act
- Antiperistalsis as the prelude to vomiting
- At the onset of vomiting, strong intrinsic contractions occur in both the duodenum and the stomach
- Partial relaxation of the lower oesophageal sphincter (LOS)
- Deep inspiration
- Raising of the hyoid bone and larynx to open the upper oesophageal sphincter
- Glottic closure
- Lifting of the soft palate to close the posterior nares
- Strong down ward contraction of diaphragm and simultaneous contraction of all the abdominal wall muscles
- Complete relaxation of the LOS
Gladwin / Sakurai 2016
Examiner Comments
2010A 22: 8 (80%) of candidates passed this question
For a good answer, candidates were expected to take the following approach and
content of information.
Triggers or initiators of vomiting include:
- Excessive distension or irritation of the upper GI tract, in particular the duodenum
- Stimulation of the chemoreceptor trigger zone (CTZ)
- Directly by certain drugs eg apomorphine, morphin
- Rhythmic motion of the body stimulating the vestibular labyrinth of the inner ear
- Cerebral excitation of vomiting by stimuli such as disquieting scenes, odors
Neuronal pathways:
Stimuli of the GI tract conveyed by vagal and sympathetic afferents to the bilateral vomiting centre within the medulla. Efferent arc from the vomiting centre via the 5th,7th,9th,10th and 12th cranial nerves, and spinal nerves to the abdominal wall muscles (and the diaphragm).
Vomiting act:
- Antiperistalsis as the prelude to vomiting
- At the onset of vomiting, strong intrinsic contractions occur in both the duodenum and the stomach
- Partial relaxation of the lower oesophageal sphincter (LOS)
- Deep breath
- Raising of the hyoid/larynx to open the upper oesophageal sphincter14
- Glottic closure
- Lifting of the soft palate to close the posterior nares
- Strong down ward contraction of diaphragm and simultaneous contraction of all the abdominal wall muscles
- Complete relaxation of the LOS
Most candidates answered this question well. Antiemetic drugs and their mechanism of action gained no marks.
Syllabus: Q1.2e
Reference: Textbook of Medical Physiology, Guyton Pg 768
2022A 14
Describe the neural integration of vomiting, highlighting the site and mechanism of action of antiemetics.
CICMWrecks Answer: Physiology of Vomiting
Physiology of Vomiting
Vomiting
- Involuntary, forceful and rapid expulsion of gastric contents through the mouth
Triggers
- Excessive GI tract distension
- Stimulation of CTZ
- Directly by certain drugs eg apomorphine, morphin
- Rhythmic motion of the body stimulating the vestibular labyrinth of the inner ear
- Cerebral excitation secondary to odours, pain, stress
Central control of vomiting
- Vomiting center (5HT3, NK1, Muscarinic and Histamine), near NTS
- Inputs
- Chemoreceptor trigger zone (NK1, 5HT3, Dopamine), area postrema outside BBB
- Vestibular system (Histamine and Muscarinic) via CNVIII
- GI Tract (5HT3, stretch and chemoreceptors) via vagal
- Higher centres
- Efferent arc
- via CN V,VII,IX,X,XII and spinal nerves to abdominal wall musles and diaphragm
- Inputs
| Afferent signal | Sensor | Efferent signal | Effect |
|---|---|---|---|
| Chemo/ baroreceptor input Drugs Stim from NTS Stim from GIT (5HT3) | CTZ (area postrema) | 5HT3, D2 and Opioid neurons | Direct stimulation of vomit centre in lateral reticular formation |
| Surgery/ Rhythmic motions | Labyrinths | ACh and H1 neurons | |
| Memory/ Emotions Sensory (sight, smell, taste) | Cortex | ||
| Severe painful stimuli | Pain | H1 neurones | |
| Irritation Manipulation during surgery Distension | GIT | NK1, NAdr, ACh neurons | |
| Via CNX, to NTS | Stimulation of CTZ then Vomit centre | ||
| Via 5HT3 to CTZ | CTZ to vomit centre | ||
| Manipulation of pharynx via CN9 to.. | NTS | Direct to CTZ | To vomit centre |
Vomiting act
- Antiperistalsis as the prelude to vomiting
- At the onset of vomiting, strong intrinsic contractions occur in both the duodenum and the stomach
- Partial relaxation of the lower oesophageal sphincter (LOS)
- Deep inspiration
- Raising of the hyoid bone and larynx to open the upper oesophageal sphincter
- Glottic closure
- Lifting of the soft palate to close the posterior nares
- Strong down ward contraction of diaphragm and simultaneous contraction of all the abdominal wall muscles
- Complete relaxation of the LOS
Gladwin / Sakurai 2016
CICMWrecks Answer: Anti-emetics
Anti-emetic Agents
| CLASS | EXAMPLES | MECHANISM OF ACTION |
|---|---|---|
| Anticholinergics | Hyoscine Atropine | – M1-Ach-R antagonism (NTS, CTZ, VC) – Small antihistamine and D2 antagonist effects |
| Antihistamines (H1) | Cyclizine Promethazine | – H1 antagonism- VC, vestibular nucleus and CTZ – Anti-muscarinic effects- NTS, CTZ, vomit center – D2 antagonism (GIT, CTZ) |
| 5-HT3 Antagonists | Ondansetron | – Peripheral in GIT – Central at VC and CTZ |
| Dopamine Antagonists | 1. Phenothiazines – Prochlorperazine (stemetil) 2. Butyrophenones – Droperidol, domperidone 3. Benzamides – Metoclopramide | – Decreased sensitivity of visceral afferents to vomit center – Central D2 blockade increased threshold at CTZ Other effects: – Inhibition of 5-HT3 – Anti-H1 effects |
| Steroids | Dexamethasone | – Proposed to act centrally to inhibit prostaglandin synthesis and inhibit endorphin receptors |
| Miscellaneous | 1. Propofol 2. Benzos 3. Cannabinoids 4. NK1- Receptor antagonists (aprepitant) | – Propofol and BZD- GABAergic inhibition of VC – Cannabinoids- Direct CTZ and VC inhibition – NK1 antagonists inhibit VC |
Examiner Comments
2022A 14: 60% of candidates passed this question.
The examiners commented that a well-drawn and labelled diagram was a very useful adjunct to answering this question. Consideration of stimulus, sensors, integrators/processors, and effectors was also useful to ensure that all components of the question were covered by a candidate’s answer.
Incorrect facts or a lack of detail about the various receptors and their locations was a common theme in answers that scored poorly. Classes of antiemetics, with specific drugs given as examples, were expected to gain marks.
2014A 03
Describe the neural integration of vomiting. (60% of marks)
Describe the pharmacology of ondansetron. (40% of marks)
CICMWrecks Answer: Physiology of Vomiting
Physiology of Vomiting
Vomiting
- Involuntary, forceful and rapid expulsion of gastric contents through the mouth
Triggers
- Excessive GI tract distension
- Stimulation of CTZ
- Directly by certain drugs eg apomorphine, morphin
- Rhythmic motion of the body stimulating the vestibular labyrinth of the inner ear
- Cerebral excitation secondary to odours, pain, stress
Central control of vomiting
- Vomiting center (5HT3, NK1, Muscarinic and Histamine), near NTS
- Inputs
- Chemoreceptor trigger zone (NK1, 5HT3, Dopamine), area postrema outside BBB
- Vestibular system (Histamine and Muscarinic) via CNVIII
- GI Tract (5HT3, stretch and chemoreceptors) via vagal
- Higher centres
- Efferent arc
- via CN V,VII,IX,X,XII and spinal nerves to abdominal wall musles and diaphragm
- Inputs
| Afferent signal | Sensor | Efferent signal | Effect |
|---|---|---|---|
| Chemo/ baroreceptor input Drugs Stim from NTS Stim from GIT (5HT3) | CTZ (area postrema) | 5HT3, D2 and Opioid neurons | Direct stimulation of vomit centre in lateral reticular formation |
| Surgery/ Rhythmic motions | Labyrinths | ACh and H1 neurons | |
| Memory/ Emotions Sensory (sight, smell, taste) | Cortex | ||
| Severe painful stimuli | Pain | H1 neurones | |
| Irritation Manipulation during surgery Distension | GIT | NK1, NAdr, ACh neurons | |
| Via CNX, to NTS | Stimulation of CTZ then Vomit centre | ||
| Via 5HT3 to CTZ | CTZ to vomit centre | ||
| Manipulation of pharynx via CN9 to.. | NTS | Direct to CTZ | To vomit centre |
Vomiting act
- Antiperistalsis as the prelude to vomiting
- At the onset of vomiting, strong intrinsic contractions occur in both the duodenum and the stomach
- Partial relaxation of the lower oesophageal sphincter (LOS)
- Deep inspiration
- Raising of the hyoid bone and larynx to open the upper oesophageal sphincter
- Glottic closure
- Lifting of the soft palate to close the posterior nares
- Strong down ward contraction of diaphragm and simultaneous contraction of all the abdominal wall muscles
- Complete relaxation of the LOS
Gladwin / Sakurai 2016
CICMWrecks Answer: Pharmacology of Ondansetron
Pharmacology of Ondansetron
Examiner Comments
2014A 03: 58% of candidates passed this question.
Candidates who failed the question did not answer the actual question. They did not discuss the neural integration but instead listed various inputs into the CTZ and vomiting centre. It was expected candidates could detail the pathways involved (afferent and efferent limbs) and describe the relationship with the coordinating centres. For example, afferent pathways to the vomiting centre include stretch and chemoreceptors located throughout the GIT via vagal and sympathetic nerves, pharyngeal touch receptors via glossopharyngeal nerves etc. Again structuring pharmacology answers was often poor.
iii. Outline the digestion and absorption of fat, protein, and carbohydrates.
iv. Outline the absorption of water, electrolytes, and vitamins.
v. Outline the gastrointestinal blood supply.
2021A 07
Outline the anatomy of the blood supply (arteries and veins) of the gastrointestinal system (oesophagus to anus)
2018A 07
Outline the blood supply to the gastrointestinal system (arteries and veins).
CICMWrecks Answer
Blood supply to the Gastrointestinal system
- Portal circulatory system + arterial blood flow into liver
- 1100ml of portal blood + 400ml from hepatic artery = 1500ml (30% CO)
- Oxygen consumption – 20-35% of total body needs
Arterial Supply
| Aorta | Division / Branches | Organ supplied | |||
|---|---|---|---|---|---|
| Thoracic A. | Subclavian A. | Thyrocervical trunk | Inf. Thyroid A. | Cervical Oesophagus | |
| Bronchial A. | branches | Thoracic Oesophagus | |||
| direct branches | |||||
| Abdominal Aorta / Coeliac | Inf. Phrenic A. | Abdominal Oesophagus | |||
| Anterior branches of Abdominal Aorta | COELIAC TRUNK | Lt. GASTRIC A. | |||
| Foregut (Stomach → major duodenal papilla | |||||
| SPLENIC A. | Short Gastric A.s | ||||
| Lt. Gastroepiploic A. | |||||
| COMMON HEPATIC A. | Hepatic A. Proper | Lt. Hepatic A. | |||
| Rt. Hepatic A. | |||||
| Gastroduodenal A. | Rt. Gastroepiploic A. (gastro-omental) | ||||
| Sup. Pancreatoduodenal A. | |||||
| Supraduodenal A. | |||||
| SUPERIOR MESENTERIC ARTERY | Inf. Pancreaticoduodenal A. | Midgut (Major duodenal papilla → 2/3 of transverse colon) | |||
| Jejunal and Ileal A.s | |||||
| Middle colic A. | |||||
| Rt colic A. | |||||
| Ileocolic A. | |||||
| INFERIOR MESENTERIC ARTERY | Lt colic A. | (2/3 transverse colon → rectum) | |||
| several sigmoid A.s | |||||
| Superior rectal A. | |||||
| Distal Abdominal Aorta | Internal Iliac A. | Middle Rectal A. | Rectum | ||
| Internal Pudendal A. | Inferior Rectal A. | ||||
Venous Drainage
| Organs drained | Branches / Tributaries | IVC | |||
|---|---|---|---|---|---|
| Liver | Hepatic V.s | IVC | |||
| Fundus + L greater curvature Stomach | Short gastric V.s | Splenic V | Portal Vein | Liver parenchyma → Hepatic Veins → IVC | |
| Greater curvature Stomach | Lt. gastro-omental V. | ||||
| Pancreas | Pancreatic V. | ||||
| colon | Lt. colic V. | IMV | |||
| sigmoid | Sigmoid V. | ||||
| rectum | Superior rectal V. | ||||
| Rectum, Colon | direct | ||||
| Rt greater curvature Stomach | Rt gastro-omental V. | SMV | |||
| Pancreas, duodenum | Ant sup pancreatocoduodenal V. | ||||
| Ant and Post inferior pancreaticoduodenal V.s | |||||
| Jejunum | Jejunal V. | ||||
| Ileum | Ileal V. | ||||
| Ileum, colon, cecum | Ileocolic V. | ||||
| ascending colon | Rt. colic V. | ||||
| transverse colon | Middle colic V. | ||||
| pancreas, duodenum | Post Sup pancreaticoduodenal V. | ||||
| stomach | Rt. gastric V. | ||||
| stomach | Lt. gastric V. | ||||
| gall bladder | cystic veins | ||||
| Skin of umbilical region | para-umbilical vein | ||||
Portosystemic Anastomosis
- Areas:
- Lower end of oesophagus
- Upper part of anal canal
- Umbilicus
- Retroperitoneal Bare area of liver
- The gastroesophageal junction around the cardia of the stomach-where the left gastric vein and its tributaries form a portosystemic anastomosis with tributaries to the azygos system of veins of the caval system.
- The anus-the superior rectal vein of the portal system anastomoses with the middle and inferior rectal veins of the systemic venous system.
- The anterior abdominal wall around the umbilicus-the para-umbilical veins anastomose with veins on the anterior abdominal wall.
Examiner Comments
2021A 07: 48% of candidates passed this question.
This question was answered best if the main arteries and veins were discussed first and then their corresponding supply outline in reasonable detail. Very few candidates were able to achieve this. Listing the names of vessels with no context and in a random non-sequential order did not attract many marks. The physiology of the blood supply to the liver also did not attract marks.
2018A 07: 7% of candidates passed this question.
An outline of the blood supply from the oesophagus down to the anus was expected. Very few candidates knew the branches of the main 3 arteries and which portion of the gastrointestinal system they supplied. Concepts related to control of blood flow and autoregulation of blood flow were not asked and therefore marks were not awarded for this information.
O2: Gastrointestinal Pharmacology
i. Describe the pharmacology of aperients, laxatives and drugs that affect gastrointestinal motility.
2012B 08
Describe the physiology of gastric emptying (80% of marks).
Outline the gastrointestinal effects of erythromycin (20% of marks)
CICMWrecks Answer: Gastric Emptying
Physiology of Gastric Emptying
Gastric emptying
- Fluids have half-time of 30mins in stomach
- Solids have half-time of 2 hours in stomach
Gastric receipt of food bolus:
- Peristaltic wave moves down the oesophagus, propelling food bolus
- Controlled by mesenteric plexus with input from vagus nerve
- Upon swallowing, the lower oesophageal sphincter and stomach relax until the oesophageal peristaltic wave has passed
- Following food bolus passage, the LOS tone increases to prevent reflux
- Food bolus reaching the stomach causes a vagal-mediated relaxation of the stomach, to accommodate gastric distension and food storage
Gastric mixing and emptying:
- Spontaneous mixing waves move down the stomach every 15-20 seconds
- Stronger waves propel gastric contents towards the pylorus (pyloric pump)
- High pyloric sphincter tone
- Allows through well-mixed liquid chyme
- Restricting gastric emptying of solids, causing mixing (retropulsion)
Control
Gastric emptying is controlled by the balance between stimulatory gastric factors and inhibitory duodenal factors
Factors promoting gastric emptying:
- Increased stomach wall stretch
- Stimulates pyloric pump
- Reduces pyloric tone
- Parasympathetic vagal stimulation
- Stimulates pyloric pump
- Gastrin
- Stimulates pyloric pump
- From G cells in antrum
- In response to presence of protein (esp. meat) in stomach
- Motilin
- Stimulates pyloric pump
- During fasting
- Stimulates pyloric pump
- From M cells in duodenum (external antigen stimulus)
- Carbohydrate: rapid emptying
Factors inhibiting gastric emptying:
- Nervous reflexes via enteric nervous system, local sympathetic trunk, and the vagal nerve to the brainstem
- in response to local conditions in the duodenum: Distension, Irritation, Acidity of chyme, Hyper- or hypo- tonicity of chyme, Breakdown products, Especially AA and FA
- Inhibit pyloric pump
- Increase pyloric sphincter tone
- Hormones (inhibit pyloric pump)
- Cholecystokinin (CCK)
- From I cells of duodenum
- In response to presence of fat and proteins
- Secretin
- From S cells of duodenum
- In response to presence of acids
- Gastric inhibitory peptide (GIP)
- From K cells of duodenum
- In response to presence of fats, proteins and carbohydrate
- Cholecystokinin (CCK)
- Other Factors :
- Sympathetic stimulus:
- Decreases contractility and reduces gastric emptying
- Dopamine:
- Decreases intragastric pressure and lower oesophageal sphincter tone
- reduces gastric emptying
- Sympathetic stimulus:
Alternate: This section can also be approached as:
- Local factors
- Gastric Factors: pump, Stomach wall distension, Amino acid
- Duodenal Factors: Type of food, stretch of wall, irritation, hyperosmolaroty, acidity, amino acid and FA content
- Neural factors
- Symptathetic
- Parasympathetic
- Hormonal factors
- Dopamine
- Gastrin
- Motilin
- Secretin
- CCK
- Somatostatin
- GIP
Mooney / Sakurai / JC 2019
CICMWrecks Answer: GI Effects of Erythromycin
Erythromycin
- Action:
- Agonist at motilin receptors on GI muscle
- Enchances motilin release from M cells in duodenum
- Promotes onset, frequency and duration of migrating motor complex
- Increases lower oesophageal tone
- May eliminate normal gut flora
Examiner Comments
2012B 08: 9 (41%) of candidates passed.
This question was best answered by using a classification system, or systematic approach to gastric emptying. Receptive relaxation (triggered by movement of food through the pharynx and oesophagus), vagally mediated relaxation of fundus and upper body of stomach, the pyloric pump (being intense peristalsis in lower body of the stomach that results in stomach emptying) and the pyloric sphincter (a circular muscle that allows water and fluids to easily pass through but restricts solids until it is mixed in chime to almost fluid consistency).
Candidates were also expected to mention regulatory factors e.g. food volume through myenteric reflexes / gastrin stimulatory motor effects and enhanced pyloric pump, acidity and osmolality of chyme in duodenum, presence of breakdown products of protein and fat through enteric nervous system, sympathetic and parasympathetic nervous systems and hormones such as cholecystokinin, secretin and gastric inhibitory peptide. Erythromycin is a commonly used prokinetic and some knowledge of effects was expected (e.g. the fact that it stimulates motilin receptors on GI smooth muscle and promote onset, frequency and duration of migrating motor complex, from stomach and spreading caudally thus increasing gastric emptying).
ii. Describe the pharmacology of drugs that influence gastric fluid pH and volume.
2010A 10
Outline the mechanism of action of drugs commonly used to prevent stress ulceration in intensive care.
CICMWrecks Answer
- Options for preventing ulceration:
- 1) Prevent acid secretion
- 2) Eliminate acid already present
- 3) Protect mucosa from acid
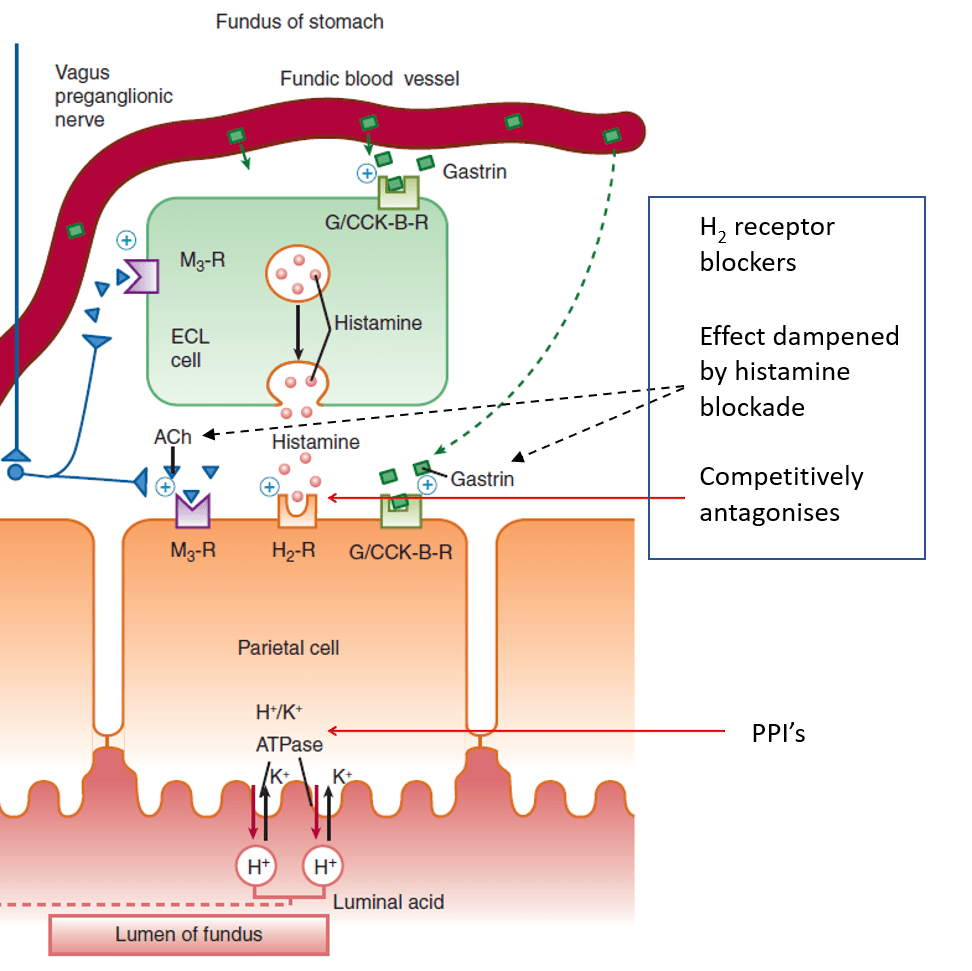
- H2-receptor antagonists:
- Competitively (and selectively) antagonise H2 receptors on parietal cells
- Dampened parietal cell response to ACh and gastrin when histamine blocked
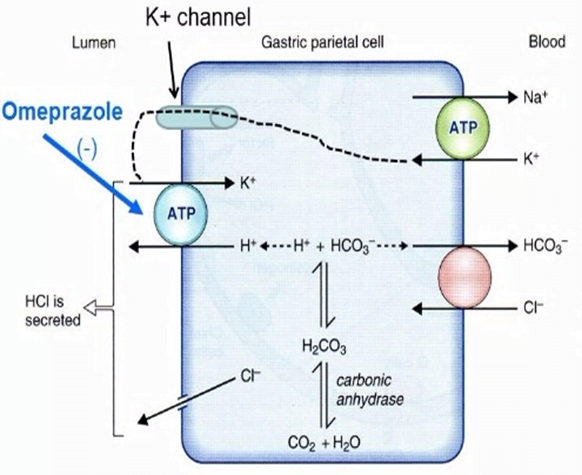
- Proton pump inhibitors:
- Prodrug
- Intestinal absorption into parietal canaliculi
- Converted to active form
- Binds covalently to H+/K+ ATPase
- Sucralfate
- Sucrose sulphate– / aluminium+ salt, which dissociates
- Sucrose sulphate binds to positively charged proteins on damaged mucosa
- Forms a barrier, protecting them from acid
- Stimulates mucosal prostaglandin and bicarbonate secretion
- Antacids
- Weak bases, reacting with HCl to form a salt and water
- Sodium bicarbonate:
- NaHCO3 + HCl -> NaCl + H2O + CO2
- Belching, and NaCl may be an issue in CKD / CCF
- Calcium carbonate:
- CaCO3 + 2HCl -> CaCl2 + H2O + CO2
- Belching, calcium toxicity, metabolic acidosis
- Magnesium and aluminium hydroxide:
- No belching (no CO2+)
- No absorption of the metal
- Magnesium salts cause diarrhoea, aluminium salts cause constipation
Mooney 2016
Examiner Comments
2010A 10: 6 (60%) of candidates passed this question
For a good answer candidates were expected to mention the following key broad points, being there are drugs that act by decreasing acid production in the stomach, drugs that act as mucosal protectors and drugs that reduce intra gastric acidity. Based upon that candidates would be expected to mention and outline the mechanism of action of H2 receptor antagonists, H+K/=ATPase (proton pump) inhibitors, sucralfate’s mechanism of action and antacids. Candidates who structured their answer tended to provide more complete answers and score better. Candidates
who failed did so because of a lack of sufficient knowledge of the mechanism of action of the drugs.
Syllabus: Q2, 2a. b,c
References: Basic and Clinical Pharmacology Katzung 10th Ed pg 1009.
Pharmacology Rang & Dale 6th Ed p 526-7, 255, 497, 587
2011A 22 – 2008A 18
Compare and contrast the pharmacology of drugs that alter the pH of gastric fluid
CICMWrecks Answer
Mechanism of Gastric Acid Secretion
- Simulation of secretion via
- ↑Gastrin via gastrin receptors
- ↑Ach via M1 rexeptors
- Histamine via H2 Receptors
- receptors located on the basolateral membrane
- Ach and gastrin → ↑ in intracellular [Ca2+]
- H2 receptors are coupled via Gs to adenyl cyclase
- ↑ in Ca2+ and cAMP → ↑ protein kinase activity → ↑ hydrogen pump activity in the luminal membrane
Drug Classes
- PROTON PUMP INIHBITORS (eg, pantoprazole)
- All are prodrugs
- MOA
- Converted to its active form in the low pH of stomach
- Accumulates in the parietal cells after absorption
- Binds to the H/K-ATPase anti-porter
- Inhibiting the proton pump and causing potent and long lasting suppression of basal and stimulated gastric acid secretion.
- PD:
- ↓ acidity/gastric secretions, no change emptying/LOS tone
- PK
- A:
- pKa ~4, lipophilic weak bases thus diffuse into acidic environments well (ie: parietal cell) thus attack secreting not quiesent pumps
- ~50% oral bioavailability, best on empty stomach
- D: High protein binding >90%
- M: rapid first pass metabolism
- E: t1/2 1.5hrs but irreversible H/KATPase bond lasts ~24hrs
- HISTAMINE-2 RECEPTOR ANTAGONISTS (eg; ranitidine)
- Bind to the H2 receptor on the basolateral surface of the parietal cell to reduce H2-stimulated acid secretion from the H/K ATPase on the luminal side of the cell.
- ↓ acidity/gastric secretions, no change emptying/LOS tone
- PK
- well orally absorbed, 50% first pass metabolism
- poorly protein bound 15%
- hepatic metabolism, does not induce p450
- MUSCARINIC ANTAGONISTS (eg, pirenzipine)
- Relatively specific M3 receptor antagonist which reduces the acetylcholine-mediated stimulation of the proton pump
- ANTACIDS (eg, Mylanta, Gastrogel).
- Weak bases which usually contain aluminium and/or magnesium compounds to chelate H+ ions
Gladwin 2016
Examiner Comments
2011A 22: 2 (17%) of candidates passed this question.
Moderately well answered overall, however many candidates lacked a systematic approach to their comparison of the pharmacology of drugs that alter the pH of gastric fluid. Few candidates discussed pharmacokinetics in sufficient detail, with only a very limited discussion comparing the absorption, metabolism and elimination of even common drugs. Relevant information such as bioavailability, duration of effect, and available formulations with dosing was often lacking. Similarly, little attention was given to important drug interactions. Many candidates included drugs which are used for gastric problems or mucosal protection, but do not specifically influence gastric pH e.g. sucrulfate. Some candidates gave unnecessarily detailed accounts of the physiology of gastric fluid production and the acid-base mechanisms involved. All candidates provided details of H2 blockers and PPIs, but often did not list representative examples or compare the effects on basal versus stimulated acid secretion. Many candidates also discussed antacids, but did not indicate their
mechanisms of action properly and did not outline potential adverse effects. Some candidates included prostaglandin analogues and anticholinergic drugs for completeness and were able to indicate their roles in affecting gastric acid secretion.
Syllabus: Q2a 2b,c
Recommended sources: Basic and Clinical Pharmacology, Katzung, Chp 62
2008A 18: 1 candidate (33%) passed this question.
The main points candidates were expected to mention were the major drug groups (antacids, H2 antagonists, proton pump blockers), describe their mechanism of action; briefly mention relevant pharmacokinetics and then briefly discuss the potential problems and interactions when using them. Additional credit was given for answers providing more detail. Many answers did not mention antacids or prostaglandin analogues, choosing only to discuss H2 receptor blockers and proton pump blockers. Even then, many answers included incorrect pharmacokinetic data. Drug interactions were rarely mentioned. A discussion of normal gastric acid secretion was not asked for and was not rewarded with marks.
Syllabus Q2a
2016B 08
Compare and contrast the pharmacology of ranitidine and omeprazole.
Examiner Comments
2016B 08: 14% of candidates passed this question.
These agents are both commonly used in the ICU. The expectation was weighted towards the interesting and important aspects of pharmacology as outlined for category B drugs.
It was expected candidates could detail that both drugs are used to suppress acid secretion in the stomach. Ranitidine is a competitive, reversible inhibitor of the action of histamine at the histamine H2 receptors found in gastric parietal cells. This results in decreased gastric acid secretion and gastric volume, and reduced hydrogen ion concentration.
In contrast to Omeprazole which is a proton pump inhibitor that irreversibly blocks
the hydrogen potassium ATPase the gastric parietal cells.
Some general description of dosing, route of administration, pharmacokinetics and possible adverse effects was expected.
iii. Describe the pharmacology of drugs with anti-emetic activity.
2016A 23 – 2009B 14
Classify anti-emetic agents by describing their mechanism of action and provide examples.
CICMWrecks Answer
Anti-emetic Agents
| CLASS | EXAMPLES | MECHANISM OF ACTION |
|---|---|---|
| Anticholinergics | Hyoscine Atropine | – M1-Ach-R antagonism (NTS, CTZ, VC) – Small antihistamine and D2 antagonist effects |
| Antihistamines (H1) | Cyclizine Promethazine | – H1 antagonism- VC, vestibular nucleus and CTZ – Anti-muscarinic effects- NTS, CTZ, vomit center – D2 antagonism (GIT, CTZ) |
| 5-HT3 Antagonists | Ondansetron | – Peripheral in GIT – Central at VC and CTZ |
| Dopamine Antagonists | 1. Phenothiazines – Prochlorperazine (stemetil) 2. Butyrophenones – Droperidol, domperidone 3. Benzamides – Metoclopramide | – Decreased sensitivity of visceral afferents to vomit center – Central D2 blockade increased threshold at CTZ Other effects: – Inhibition of 5-HT3 – Anti-H1 effects |
| Steroids | Dexamethasone | – Proposed to act centrally to inhibit prostaglandin synthesis and inhibit endorphin receptors |
| Miscellaneous | 1. Propofol 2. Benzos 3. Cannabinoids 4. NK1- Receptor antagonists (aprepitant) | – Propofol and BZD- GABAergic inhibition of VC – Cannabinoids- Direct CTZ and VC inhibition – NK1 antagonists inhibit VC |
Examiner Comments
2016A 23: 52% of candidates passed this question.
Successful candidates were those who discussed the multiple locations in the vomiting pathway where a drug acts, the receptors involved and discussed 5 or more classes. Several approaches can be taken to this topic. Classification by drug group works well and then allows more detail to be provided about possible receptor activity.
For example:
Anithistamines: Promethazine H1 ++++ M ++ D2 ++ 5-HT3
Anitcholinergics: Scopalamine H1 + M ++++ D2 + 5-HT3
Benzamines: Metoclopromide H1 + M — D2 +++ 5-HT3 ++,
Neuroleptics: Droperidol H1 + M – D2 +++ 5-HT3 +,
5-HT3 Antagonists: Ondansetron H1 – M – D2 – 5-HT3 ++++, Granisetron H1 ++++ M ++
D2 ++ 5-HT3 ; Glucocorticoids: Dexamethasone H1 – M – D2 – 5-HT3 -,
Propofol: GABBA
Cannabinoids: direct on vomiting center.
An alternative approach involves a discussion of the distribution of receptor sites: nucleus vestibularis H1 M, area postrema (chemoreceptor trigger zone) 5-HT3 D2 M1 H1, nucleus tractus solitarius 5-HT3 D2 M H2 and then discuss which drugs act where. This material has also been previously covered in the viva examination and knowledge of both drug properties and receptor distribution is often required.
Few answers detailed relative activity at various receptors types – “+” scale illustrated above would be sufficient to convey an understanding to the examiners.
2009B 14: 3 (33%) of candidates passed this question.
Antiemetics can be classified by their receptor actions including, dopamine antagonists, serotonin antagonists, antihistamines, anticholinergics, antimotilinic etc or by their drug type – butyrophenones, phenothiazines, benzamides etc. Marks were divided between each class, and for “other/novel” antiemetics – such as, steroids, GABA agonists, alpha 2 agonists, mu receptor antagonists, canabinoids, propofol and NK1 receptor antagonists.
Candidates were expected to mention the drug type, receptor interaction, the location of the receptors and the pathways inhibited by the drug – central CTZ, vestibular nuclei, solitary tract nucleus, vagal afferents or GIT motility and secretions. Most drugs work at one or more of these sites and marks were awarded for mention of this. Commonest errors were omission of adequate detail in each class. Antihistamines, anticholinergics and “others/novel” were frequently omitted.
Syllabus – Q12e and Q2b2a
Reference: Chp 37 Goodman and Gillman
2022A 14
Describe the neural integration of vomiting, highlighting the site and mechanism of action of antiemetics.
CICMWrecks Answer: Physiology of Vomiting
Physiology of Vomiting
Vomiting
- Involuntary, forceful and rapid expulsion of gastric contents through the mouth
Triggers
- Excessive GI tract distension
- Stimulation of CTZ
- Directly by certain drugs eg apomorphine, morphin
- Rhythmic motion of the body stimulating the vestibular labyrinth of the inner ear
- Cerebral excitation secondary to odours, pain, stress
Central control of vomiting
- Vomiting center (5HT3, NK1, Muscarinic and Histamine), near NTS
- Inputs
- Chemoreceptor trigger zone (NK1, 5HT3, Dopamine), area postrema outside BBB
- Vestibular system (Histamine and Muscarinic) via CNVIII
- GI Tract (5HT3, stretch and chemoreceptors) via vagal
- Higher centres
- Efferent arc
- via CN V,VII,IX,X,XII and spinal nerves to abdominal wall musles and diaphragm
- Inputs
| Afferent signal | Sensor | Efferent signal | Effect |
|---|---|---|---|
| Chemo/ baroreceptor input Drugs Stim from NTS Stim from GIT (5HT3) | CTZ (area postrema) | 5HT3, D2 and Opioid neurons | Direct stimulation of vomit centre in lateral reticular formation |
| Surgery/ Rhythmic motions | Labyrinths | ACh and H1 neurons | |
| Memory/ Emotions Sensory (sight, smell, taste) | Cortex | ||
| Severe painful stimuli | Pain | H1 neurones | |
| Irritation Manipulation during surgery Distension | GIT | NK1, NAdr, ACh neurons | |
| Via CNX, to NTS | Stimulation of CTZ then Vomit centre | ||
| Via 5HT3 to CTZ | CTZ to vomit centre | ||
| Manipulation of pharynx via CN9 to.. | NTS | Direct to CTZ | To vomit centre |
Vomiting act
- Antiperistalsis as the prelude to vomiting
- At the onset of vomiting, strong intrinsic contractions occur in both the duodenum and the stomach
- Partial relaxation of the lower oesophageal sphincter (LOS)
- Deep inspiration
- Raising of the hyoid bone and larynx to open the upper oesophageal sphincter
- Glottic closure
- Lifting of the soft palate to close the posterior nares
- Strong down ward contraction of diaphragm and simultaneous contraction of all the abdominal wall muscles
- Complete relaxation of the LOS
Gladwin / Sakurai 2016
CICMWrecks Answer: Anti-emetics
Anti-emetic Agents
| CLASS | EXAMPLES | MECHANISM OF ACTION |
|---|---|---|
| Anticholinergics | Hyoscine Atropine | – M1-Ach-R antagonism (NTS, CTZ, VC) – Small antihistamine and D2 antagonist effects |
| Antihistamines (H1) | Cyclizine Promethazine | – H1 antagonism- VC, vestibular nucleus and CTZ – Anti-muscarinic effects- NTS, CTZ, vomit center – D2 antagonism (GIT, CTZ) |
| 5-HT3 Antagonists | Ondansetron | – Peripheral in GIT – Central at VC and CTZ |
| Dopamine Antagonists | 1. Phenothiazines – Prochlorperazine (stemetil) 2. Butyrophenones – Droperidol, domperidone 3. Benzamides – Metoclopramide | – Decreased sensitivity of visceral afferents to vomit center – Central D2 blockade increased threshold at CTZ Other effects: – Inhibition of 5-HT3 – Anti-H1 effects |
| Steroids | Dexamethasone | – Proposed to act centrally to inhibit prostaglandin synthesis and inhibit endorphin receptors |
| Miscellaneous | 1. Propofol 2. Benzos 3. Cannabinoids 4. NK1- Receptor antagonists (aprepitant) | – Propofol and BZD- GABAergic inhibition of VC – Cannabinoids- Direct CTZ and VC inhibition – NK1 antagonists inhibit VC |
Examiner Comments
2022A 14: 60% of candidates passed this question.
The examiners commented that a well-drawn and labelled diagram was a very useful adjunct to answering this question. Consideration of stimulus, sensors, integrators/processors, and effectors was also useful to ensure that all components of the question were covered by a candidate’s answer.
Incorrect facts or a lack of detail about the various receptors and their locations was a common theme in answers that scored poorly. Classes of antiemetics, with specific drugs given as examples, were expected to gain marks.
2012A 23
Classify antiemetic drugs and give an example from each group (60% of marks).
Outline the gastrointestinal effects of metoclopramide (40% of marks).
CICMWrecks Answer: Anti-emetics
Anti-emetic Agents
| CLASS | EXAMPLES | MECHANISM OF ACTION |
|---|---|---|
| Anticholinergics | Hyoscine Atropine | – M1-Ach-R antagonism (NTS, CTZ, VC) – Small antihistamine and D2 antagonist effects |
| Antihistamines (H1) | Cyclizine Promethazine | – H1 antagonism- VC, vestibular nucleus and CTZ – Anti-muscarinic effects- NTS, CTZ, vomit center – D2 antagonism (GIT, CTZ) |
| 5-HT3 Antagonists | Ondansetron | – Peripheral in GIT – Central at VC and CTZ |
| Dopamine Antagonists | 1. Phenothiazines – Prochlorperazine (stemetil) 2. Butyrophenones – Droperidol, domperidone 3. Benzamides – Metoclopramide | – Decreased sensitivity of visceral afferents to vomit center – Central D2 blockade increased threshold at CTZ Other effects: – Inhibition of 5-HT3 – Anti-H1 effects |
| Steroids | Dexamethasone | – Proposed to act centrally to inhibit prostaglandin synthesis and inhibit endorphin receptors |
| Miscellaneous | 1. Propofol 2. Benzos 3. Cannabinoids 4. NK1- Receptor antagonists (aprepitant) | – Propofol and BZD- GABAergic inhibition of VC – Cannabinoids- Direct CTZ and VC inhibition – NK1 antagonists inhibit VC |
CICMWrecks Answer: GI Effects of Metoclopramide
Gastrointestinal effects of Metoclopramide
- Selective stimulation of gastric muscarinic receptors
- acts primarily by augmenting release of ACh and perhaps by inhibition of 5-HT release
- Coordinated gastric, pyloric and duodenal activity contraction (accelerates gastric emptying)
- Increased amplitude and frequency of Longitudinal muscle contraction
- Lowers threshold for peristaltic reflex to occur
- Reduces intestinal muscle fatigue
- Direct action on smooth muscle to increase tone (including increased LOS)
- relaxes the pyloric sphincter
Examiner Comments
2012A 23: 4 (40%) of candidates passed.
Antiemetics, as a topic has been frequently asked, in various formats in the past. Candidates who performed well had a good depth and breadth of knowledge as well as sufficient integration of knowledge to be able to classify and understand the basis to the various classifications. Essentially it was expected that candidates mention the classifications of Anticholinergics, Antihistamines, Anti 5HT, Antidopaminergics (benzamides, butyrophenones, phenothiazines), Steroids and other agents with known antiemetic activity (e.g. propofol, benzodiazepines, etc). In relation to metoclopramide it was expected that candidates would mention that it lowers pressure threshold for occurrence of intestinal peristaltic reflex, reduces intestinal muscle fatigue, enhances frequency and amplitude of longitudinal muscle contraction, coordinates gastric, pyloric and duodenal activity to improve GI motility, mechanism of action appears to depend on intramural cholinergic neuron, acts primarily by augmenting release of ACh and perhaps by inhibition of 5-HT release, increases lower oesophageal sphincter pressure, relaxes the pyloric sphincter and antagonize the inhibitory neurotransmitter, dopamine.
2014A 03
Describe the neural integration of vomiting. (60% of marks)
Describe the pharmacology of ondansetron. (40% of marks)
CICMWrecks Answer: Physiology of Vomiting
Physiology of Vomiting
Vomiting
- Involuntary, forceful and rapid expulsion of gastric contents through the mouth
Triggers
- Excessive GI tract distension
- Stimulation of CTZ
- Directly by certain drugs eg apomorphine, morphin
- Rhythmic motion of the body stimulating the vestibular labyrinth of the inner ear
- Cerebral excitation secondary to odours, pain, stress
Central control of vomiting
- Vomiting center (5HT3, NK1, Muscarinic and Histamine), near NTS
- Inputs
- Chemoreceptor trigger zone (NK1, 5HT3, Dopamine), area postrema outside BBB
- Vestibular system (Histamine and Muscarinic) via CNVIII
- GI Tract (5HT3, stretch and chemoreceptors) via vagal
- Higher centres
- Efferent arc
- via CN V,VII,IX,X,XII and spinal nerves to abdominal wall musles and diaphragm
- Inputs
| Afferent signal | Sensor | Efferent signal | Effect |
|---|---|---|---|
| Chemo/ baroreceptor input Drugs Stim from NTS Stim from GIT (5HT3) | CTZ (area postrema) | 5HT3, D2 and Opioid neurons | Direct stimulation of vomit centre in lateral reticular formation |
| Surgery/ Rhythmic motions | Labyrinths | ACh and H1 neurons | |
| Memory/ Emotions Sensory (sight, smell, taste) | Cortex | ||
| Severe painful stimuli | Pain | H1 neurones | |
| Irritation Manipulation during surgery Distension | GIT | NK1, NAdr, ACh neurons | |
| Via CNX, to NTS | Stimulation of CTZ then Vomit centre | ||
| Via 5HT3 to CTZ | CTZ to vomit centre | ||
| Manipulation of pharynx via CN9 to.. | NTS | Direct to CTZ | To vomit centre |
Vomiting act
- Antiperistalsis as the prelude to vomiting
- At the onset of vomiting, strong intrinsic contractions occur in both the duodenum and the stomach
- Partial relaxation of the lower oesophageal sphincter (LOS)
- Deep inspiration
- Raising of the hyoid bone and larynx to open the upper oesophageal sphincter
- Glottic closure
- Lifting of the soft palate to close the posterior nares
- Strong down ward contraction of diaphragm and simultaneous contraction of all the abdominal wall muscles
- Complete relaxation of the LOS
Gladwin / Sakurai 2016
CICMWrecks Answer: Pharmacology of Ondansetron
Pharmacology of Ondansetron
Examiner Comments
2014A 03: 58% of candidates passed this question.
Candidates who failed the question did not answer the actual question. They did not discuss the neural integration but instead listed various inputs into the CTZ and vomiting centre. It was expected candidates could detail the pathways involved (afferent and efferent limbs) and describe the relationship with the coordinating centres. For example, afferent pathways to the vomiting centre include stretch and chemoreceptors located throughout the GIT via vagal and sympathetic nerves, pharyngeal touch receptors via glossopharyngeal nerves etc. Again structuring pharmacology answers was often poor.
2012B 17
Classify the 5HT receptors and give examples of pharmacological agents that affect them (60% of marks).
Outline the pharmacology of ondansetron (40% of marks).
CICMWrecks Answer: 5HT receptors and agents
5HT Receptors
5-HT receptor subtypes comprise the largest known neurotransmitter-receptor family.
- 4 5-HT receptor families recognized
- All members of GPCR superfamily except 5HT3
- 5HT3 is a ligand gated ion channel that conducts Na and K
- Overall effects
- CNS
- Vasoconstriction
- Increased inotropy and chronotropy
- Resp
- Bronchial smooth muscle constriction
- CNS
- Sleep-wake cycle
- Temperature regulation
- Appetite
- Mood
- Impulsivity
- Anxiety and Depression
- Sexual behaviour
- CNS
| Mechanism | Sites of Action | Effect | Drugs | |
|---|---|---|---|---|
| 5HT1 | – GiPCR – Some subtypes also act as ligand gated ion channels | Inhibitory autoreceptor on serotonergic cells Endothelium | – Inhibition of serotonin secretion – Endothelial No release | Agonist – Sumitriptan (migraine) – Ergotamine – LSD |
| 5HT2 | Gq or G11PCR | CNS – Pre-frontal – Parietal – Somatosensory – Choroid plexus GI Tract Platelets | – Platelet aggregation and vasoconstriction | Agonist – LSD Antagonist – Clozapine – Risperidone |
| 5HT3 | Ligand gated Na and K channel | CNS – Area Postrema (CTZ) – NTS (Vomiting centre) GI Tract – Parasympathetic nerve terminals | Emesis | Antagonist Ondansetron |
| 5HT4 | GsPCR | CNS GI Tract – Myenteric plexus – Secretory cells | GI peristalsis and secretion |
- Additional receptors cloned
- 5HT5~7 (GsPCR) Unknown clinical relenvance
- Other drugs with effects on serotonergic system
- Increase serotonin release
- MDMA
- Decrease serotonin reuptake
- Tramadol
- 1R2R(+) Tramadol
- SSRI
- Tricyclic Antidepressants
- Tramadol
- Decrease serotonin metabolism
- MAO Inhibitors
- Increase serotonin release
Mooney 2016
CICMWrecks Answer: Pharmacology of Ondansetron
Pharmacology of Ondansetron
Examiner Comments
2012B 17: 10 (45.4%) of candidates passed.
The 5HT (5 Hydroxytryptamine or serotonin) receptor is a monoamine neurotransmitter synthesized from tryptophan, and is an important receptor in the body.. It is found in the CNS, gastrointestinal tract, platelets and mast cells. There are 7 main receptor subtypes (GProtein coupled are 5HT1, 5HT2, 5HT4 and 5HT7 and ligand-gated ion channel 5HT3). Drugs may affect them by acting on serotonergic transmission (degradation inhibitors – MAOI e.g. selegiline, storage inhibitors- amphetamine, reuptake inhibitors – SSRI’s or tricyclic antidepressants), serotonin agonists (selective-5HT1B, 5HT1D e.g. triptans for migraine, non-selective, e.g. ergotamine), serotonin antagonists (ketanserin, clozapine, ondansetron).
Ondansetron is a commonly used anti-emetic. Candidates were expected to mention, that it is a selective antagonist at the 5HT3 receptor centrally and peripherally. To outline “pharmacology” it was also expected that answers would mention that it comes in a variety of formulations and to outline its fundamental pharmacokinetic properties.
iv. Describe the pharmacology of octreotide, vasopressin and terlipressin.
2015A 06
Outline the physiology of pancreatic secretion (80% of marks)
and outline the pharmacology of octreotide (20% of marks)
CICMWrecks Answer: Pancreas Secretions
Pancreatic Secretion
| EXOCRINE SECRETIONS | HCO3– | |
| Water | ||
| Enzymes | Proteases | |
| Amylase | ||
| Lipase | ||
| Others | ||
| ENDOCRINE SECRETIONS | Insulin | |
| Glucagon | ||
| Somatostatin | ||
Exocrine Secretions
- produced by acinar and ductal cells
- ~1.5L per day
- HCO3–
- alkalinize gastric contents
- enzyme carbonic anhydrase
- Water
- Enzymes
- Proteases: Trypsinogen → Trypsin (by enterokinase in gut), Chymotrypsinogen → Chymotrypsin. Proteolysis.
- Amylase: Hydrolysis of glycogen, starch, and complex carbohydrate.
- Lipase: Hydrolysis of dietary triglycerides.
- Others: ribonuclease, deoxyribonuclease, gelatinase and elastase
Endocrine Secretions
- Insulin
- polypeptide hormone
- synthesized from proinsulin in RER of B cells in Islets of Langerhans
- Excreted via exocytosis in response to ↑intracellulae Ca2+
- Minimal protein binding, tiny Vd 0.075 L/kg
- Metabolized in liver, muscle, kidney byt Glutathione insulin transhydrogenase
- Renal elimination of inactive metabolites
- Circulatory hald life ~5mins
- Increased anabolism, decreased catabolism
- maintains normal blood glucose levels by facilitating cellular glucose uptake, regulating carbohydrate, lipid and protein metabolism
- promotes cell division and growth through its mitogenic effects
- Glucagon
- polypeptide hormone
- synthesized in pancreatic A cells
- secreted into portal vein
- Circulating half life ~5mins
- Metabolized in liver (1st pass) – low circulating level
- Glycogenolysis, gluconeogenesis, glucose release, ketone formation
- Lipolysis
- Inotopy, increases metabolic rate
- Stimulates somatostatin, insulin release
- Somatostatin
- polypeptide hormone
- Inhibits Glucagon, Insulin, other pancreatic peptides
- may function as CNS neurotransmitter
CICMWrecks Answer: Pharmacology of Octreotide
Pharmacology of Octreotide
Examiner Comments
2015A 06: 38 % of candidates passed this question.
An outline of exocrine function should have included the sources of secretions, secretions involved in the digestion of proteins, carbohydrates and fats, the roles of trypsin inhibitors and bicarbonate secretion and the regulation of enzyme and bicarbonate secretion.” Knowledge of endocrine physiology was good whereas the depth of knowledge regarding exocrine function was generally shallow with many errors.
Only some general facts around the pharmacology of octreotide were required to pass this section of the question. Responses revealed limited knowledge and contained many errors.
2017A 20
Describe the pharmacology of vasopressin (70% of marks) and its analogues (30% of marks).
2013A 22
Describe the actions of endogenous vasopressin. (60% of marks)
List the vasopressin analogues and their uses. (40% of marks)
Examiner Comments
2017A 20: 28% of candidates passed this question.
A pharmacology answer template outlining pharmacokinetics and dynamics was required. Candidates failed to score marks for describing the physiology of vasopressin secretion. A number of answers demonstrated limited knowledge about its indications for use and its potential adverse effects.
2013A 22:
Overall the first section was not answered in sufficient detail. Aspects such as the antidiuretic effects of vasopressin were often overlooked. Some candidates spent more time on outlining the clinical contexts in which vasopressin is used (which did not score marks), rather than the physiology (which did score marks). DDAVP was the most common analogue mentioned, with the others often being omitted (e.g. terlipressin, ornipressin, etc.).
VIVAs
| 2023B | |
| 2023A | |
| 2022B | |
| 2022A | |
| 2021B | Functions of stomach. PPI action |
| 2021A | Nausea and Vomiting. Sequential muscle contractions during vomiting |
| 2020B | |
| 2019B | |
| 2019A | |
| 2018B | |
| 2018A | Define vomiting. Describe the inputs to the vomiting centre. |
| 2017B | |
| 2017A | |
| 2016B | |
| 2016A | glucose and lipid metabolism, daily nutritional requirement, insulin physio |
| 2015B | |
| 2015A | |
| 2014B | |
| 2014A | |
| 2013B | Physiology of swallowing, food passage, stages, cough reflex an dinnervation of larynx, LES, Metochlopramide |
| 2013A | |
| 2012B | |
| 2012A | |
| 2011B | |
| 2011A | |
| 2010B | |
| 2010A | |
| 2009B | |
| 2009A | |
| 2008B | Prokinetics, Laxatives, Octreotide |
| 2008A | |
| 2007B |

Recent Comments