Syllabus (Fourth Edition, 2023)
Topics
M1: Physiology of the Autonomic Nervous System
i. Describe the autonomic nervous system including anatomy, receptors and their subtypes and transmitters (including their synthesis, release, and fate).
M2: Pharmacology of the Autonomic Nervous System
i. Understand the pharmacology of drugs acting upon the autonomic nervous system.
ii. Describe the structure activity relationships of adrenergic and cholinergic drugs.
iii. Outline the mechanisms by which drugs may affect neurotransmission and noradrenaline effect at the sympathetic nerve terminal.
Topics not covered in previous SAQs
M2: Pharmacology of the Autonomic Nervous System
ii. Describe the structure activity relationships of adrenergic and cholinergic drugs.
iii. Outline the mechanisms by which drugs may affect neurotransmission and noradrenaline effect at the sympathetic nerve terminal.
Learning Objectives for the First Part Examination in Intensive Care Medicine
- This will ensure that trainees, tutors, and examiners can work from a common base.
- All examination questions are based around this Syllabus.
- These learning objectives are designed to outline the minimum level of understanding required for each topic.
- The accompanying texts are recommended on the basis that the material contained within them provides sufficient information for trainees to meet the learning objectives.
- Trainees are strongly encouraged to explore the existing and evolving body of knowledge of the Basic Sciences as they apply to Intensive Care Medicine by reading widely.
- For all sections of the syllabus an understanding of normal physiology and physiology at extremes of age, obesity, pregnancy (including foetal) and disease (particularly critical illness) is expected.
- Similarly, for pharmacology, trainees are expected to understand a drug’s pharmacology in these contexts.
- An understanding of potential toxicity and relevant antidotes is also expected.
Definitions
Throughout the document specific wording has been used under the required abilities to indicate the level of knowledge and understanding expected and a glossary of these terms is provided.
Definitions
| Calculate | Work out or estimate using mathematical principles. |
| Classify | Divide into categories; organise, arrange. |
| Compare and contrast | Examine similarities and differences. |
| Define | Give the precise meaning. |
| Describe | Give a detailed account of. |
| Explain | Make plain. |
| Interpret | Explain the meaning or significance. |
| Outline | Provide a summary of the important points. |
| Relate | Show a connection between. |
| Understand | Appreciate the details of; comprehend. |
SAQs
M1. Physiology of the Autonomic Nervous System
i. Describe the autonomic nervous system including anatomy, receptors and their subtypes and transmitters (including their synthesis, release, and fate).
2017B 07
Compare and contrast the sympathetic and parasympathetic nervous systems
CICMWrecks Answer
| Sympathetic nervous system | Parasympathetic nervous system | |
|---|---|---|
| Introduction | The sympathetic nervous system (SNS) is one of two main divisions of the autonomic nervous system (ANS). Its general action is to mobilize the body’s fight-or-flight response. | The parasympathetic nervous system is one of the two main divisions of the autonomic nervous system (ANS). Its general function is to control homeostasis and the body’s rest-and-digest response. |
| Function | Control the body’s response during perceived threat. Diffuse physiological accelerator | Control the body’s response while at rest. Acts as local brake |
| Activates response of | Fight-or-flight | Rest and digest |
| Neuron Pathways | Very short neurons, faster system | Longer pathways, slower system |
| Supplies | Viscera and skin | Only viscera |
| Sympathetic nervous system | Parasympathetic nervous system | |
|---|---|---|
| Originates in | Thoracic and lumbar regions of spinal cord | Sacral region of spinal cord, medulla, cranial nerves 3, 7, 9, and 10 |
| Pre-Ganglionic fibres | Cholinergic | Cholinergic |
| Ganglion | Sympathetic ganglion – Synapse between Short pre-ganglionic fibre Long post-ganglionic fibre | PNS Ganglion sit close to target organ. Long pre-ganglionic fibre Short post ganglionic fibre |
| Post-ganglionic | Release Norad Ach at Adrenal medulla & Sweat glands | All release Ach |
| Target organ receptors | Adrenoreceptors (Alpha 1&2, Beta 1&2) G protein coupled | Ach receptors: Muscarinic M1-5: G protein couples Nicotinic: Ion channel |
| Sympathetic nervous system | Parasympathetic nervous system | |
|---|---|---|
| General Body Response | Body speeds up, tenses up, becomes more alert. Functions not critical to survival shut down. | Counterbalance; restores body to state of calm. |
| Cardiovascular System (heart rate) | ↑↑↑ inotropy ↑↑↑ Chronotropy ↑↑↑ lusitropy ↑↑ dromotropy | ↓ inotropy (Atria > Vent) ↓↓↓ Chronotropy ↓ lusitropy (Atria > Vent) ↓↓↓ dromotropy |
| Vasculature | Constriction | |
| Pulmonary System (lungs) | Bronchial tubes dilate | Bronchoconstriction increased mucous production |
| Musculoskeletal System | Sweating, contraction, lipolysis | Muscles relax |
| Pupils | Dilate | Constrict, lacrimation |
| Gastrointestinal System | Decreased salivation and GIT motility, increased sphincter tone, gluconeogenesis | Increases stomach movement and secretions, decreased sphincter tone |
| Salivary Glands | Saliva production decreases | Saliva production increases |
| Endocrine | Adrenaline and noradrenaline release | No involvement |
| GU | Detrusor relaxation, sphincter contraction, ↑ uterine tone | Detrusor contraction, erection |
JC 2019
Examiner Comments
2017B 07: 75% of candidates passed this question.
This question was generally well answered A table or diagram lent structure to the answer. More complete answers included details on the function, anatomy, a description of the pre- and post-ganglionic fibres, ganglia, receptors and neurotransmitters involved. Whilst most commented on ‘fight or flight’ for the SNS and ‘rest and digest’ for the PNS, no candidate observed that the SNS is a diffuse physiological accelerator and that the PNS acts as a local brake. No candidate included the fact that the SNS supplies viscera and skin whilst the PNS only supplies the viscera. Many candidates failed to make reference to the fact that the postganglionic SNS receptor is G protein coupled and the PNS postganglionic receptor is Gcoupled on muscarinic receptors but operates an ion channel when nicotinic. Candidates may have scored higher if they had provided a little more detail in their answers.
2024A 05
Outline the anatomy of the sympathetic nervous system including:
(i) The origin (15% of marks).
(ii) Fibre types and their course (70% of marks).
(iii) Receptors and neurotransmitters (15% of marks).
2020B 05
Describe the anatomy (70% marks) and effects (30% marks) of the sympathetic nervous system.
2015A 20 – 2013B 17
Describe the anatomy of the sympathetic nervous system.
CICMWrecks Answer
Anatomy of SNS
- Posterior hypothalamus is the main site of sympathetic nervous outflow
- Receives input from cardiovascular centres of medulla and pons
- Sympathetic innervation from Sympathetic trunks
- Paired bundle of sympathetic neurons run lateral from vertebral bodies from T1 to L2
- Consists of two neurons in series
- Short Pre-ganglionic neuron → Sympathetic ganglion → Long Post-ganglionic neuron
Origin
- Origin: Preganglionic fibres originate in the grey matter of the spinal cord lateral horn
- Nerve Fibres and Pathway: Leave the spinal cord through ventral roots (with spinal nerves)
- Leave spinal nerves, travel as white rami communicantes (short myelinated B fibres)
- Meet with the ganglia of the sympathetic trunk
- Synapse with post-ganglionic neurons
- Neurotransmitter: Preganglionic neurotransmitter is acetylcholine
- Receptor: nicotinic receptors
Sympathetic trunk:
4 parts
- Cervical part
- Head
- Neck
- Thorax
- Thoracic part (T1-T5)
- Aortic plexus
- Pulmonary plexus
- Cardiac plexus
- Thoracic splanchnic nerves
- Lumbar sympathetic ganglia
- Coeliac plexus
- Pelvic part
- Hypogastric plexus
- Pelvic plexus
Post-ganglionic
- Nerve Fibres and Pathway: Post-ganglionic neurons leave the ganglia as grey rami communicantes
- Long unmyelinated C fibres
- Rejoin the spinal nerves to travel to target organs
- Neurotransmitter: Postganglionic neurotransmitter is noradrenaline
- (acetylcholine in muscles, sweat glands and hair follicles)
- Receptor: Adrenergic alpha and beta receptors on target organs/vessels
Exception is adrenal medullary outflow:
- Modified post-ganglionic cells release adrenaline into circulation
- Innervated directly by pre-ganglion sympathetic fibres
Effects of SNS
| Function | Control the body’s response during perceived threat. Diffuse physiological accelerator |
| Activates response of | Fight-or-flight |
| General Body Response | Body speeds up, tenses up, becomes more alert. Functions not critical to survival shut down. |
| Cardiovascular System | ↑↑↑ Chronotropy, ↑↑↑ inotropy, ↑↑↑ lusiotropy, ↑↑ dromotropy |
| Vasculature | Constriction |
| Pulmonary System | Bronchial tubes dilate |
| Musculoskeletal System | Sweating, contraction, lipolysis |
| Pupils | Dilate |
| Gastrointestinal System | Decreased salivation and GIT motility, increased sphincter tone, gluconeogenesis |
| Salivary Glands | Saliva production decreases |
| Endocrine | Adrenaline and noradrenaline release |
| GU | Detrusor relaxation, sphincter contraction, ↑ uterine tone |
Mooney / JC 2020
Examiner Comments
2024A 05: 54% of candidates passed this question.
The question provided the headings that candidates would be expected to provide information on and those that used these headings to structure their answers provided good overall responses. A definition of the SNS and effects of activation was not required. Candidates were expected to outline SNS anatomy with respect to origin (pre-ganglionic neurons in the grey matter of the lateral horn of the spinal cord, T1 to L2), fibre types including a description of short pre-ganglionic myelinated b fibres, the sympathetic chain and the long post-ganglionic unmyelinated C fibres. Receptors and neurotransmitters included nicotinic Ach receptors in the ganglion and adrenergic alpha and beta receptors on target organs/vessels. A brief discussion of the arrangement at the adrenal medulla was also expected.
2020B 05: 51% of candidates passed this question.
Most candidates had a suitable structure to their answers, those without a clear organisation of thought tended to gain fewer marks. In many cases incorrect information or limited detail, particularly around the anatomical organisation prevented higher marks.
2015A 20: 25 % of candidates passed this question.
A definition of the sympathetic system, followed by a systematic description of the central sympathetic centres; what happens at the spinal cord; the anatomy of the pre and post ganglionic fibres would have been awarded with a pass mark. Additional information about the sympathetic ganglia and the neurotransmitters involved would have rounded off a good answer.
Many answers lacked anatomical detail and described the actions (function) of the sympathetic system which was not asked for.
Most answers lacked any structure. The most common reason for not passing this question was that significant sections of the anatomy from central to peripheral were not mentioned. Most had a simple sketch understanding of the question asked but could not add enough of the next layer to be awarded a pass mark.
2013B 17: 3 candidates passed (11.1%).
Knowledge of the anatomy of the sympathetic nervous system is important in helping to understand its physiology, and the pharmacology of drugs that affect it. Such information is widely available within most physiology, and even pharmacology texts when mentioning the sympathetic nervous system. In general candidates lacked depth and often were inaccurate in their description. A systematic approach (e.g. spinal levels, pre-ganglionic, post-ganglionic, etc.) was often lacking.
2011B 23
Outline the production, release, and fate of noradrenaline at the sympathetic nerve terminal.
CICMWrecks Answer
Sympathetic Nervous System
- Short pre-ganglionic B fibres terminating at the paravertebral sympathetic chain → Synapse with postganglionic fibres and release Ach
- Long post-ganglionic fibres innervating target tissues → Release noradrenaline (Except sweat glands and adrenals)
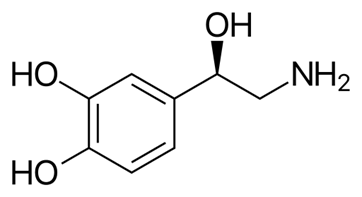
Noradrenaline
- Naturally occuring catecholamine derived from catecholamine
- Direct α adrenoceptor agonist with partial β adrenoceptor agonism
- Peripheral vasoconstriction with increased MAP and diastolic pressures
Production
- Derived from tyrosine
- Tyrosine → L-DOPA (Tyrosine hydroxylase)
- L-DOPA → Dopamine (Dopa decarboxylase)
- Dopamine → Nordrenaline (Dopamine hydroxylase)
- Noradrenaline → Adrenaline (PMNT)

- Enzymes required for noradrenaline synthesis present widely in peripheral sympathetic neurons
- Tyrosine hydroxylase is the rate limiting step and can be upregulated by PKA phosphorylation
- Noradrenaline stored in vesicles in post-ganglionic sympathetic nerve terminals – Vesicular Monoamine Transporter (VMAT2)
Release
- On action potential arrival at sympathetic nerve terminal
- Specific mechanisms for catecholamine release are unknown, however thought to be due to increased [Ca2+] at the nerve terminal in response to action potential
- Vesicles fuse with cell membrane and contents released into the nerve-effector junction
Fate
- Noradrenaline released from nerve terminal binds to adrenergic G Protein Coupled Receptors on target tissues causing various sympathetic effects
- Noradrenaline binds to prejunctional α2 receptors preventing further noradrenaline release
- NET proteins cause re-uptake of noradrenaline into nerve terminals where they may be metabolized by monoamine oxidase (MAO) enzymes or repackaged into neurotransmitter vesicles
- Noradrenaline can diffuse away from the junctional cleft into the systemic circulation and metabolized by Catechol O-Methyl Transferase (COMT) enzymes in liver and other tissues
- Metabolites → VMA and Normetadrenaline → renal elimination
Sakurai 2016
Examiner Comments
2011B 23: 10 (40%) of candidates passed this question.
The question consisted of three parts (production, release and fate of noradrenaline). The context was the sympathetic nerve terminal. The synthesis of Noradrenaline from Tyrosine was expected. Better answers mentioned the roles of Tyrosine Hydrolase, DOPA Decarboxylase and DOPA Beta-hydroxylase. Candidates were expected to describe the storage of Noradrenaline in vesicles and Ca++-mediated exocytosis in response to an action potential. Noradrenaline binds to post-synaptic and pre-synaptic receptors. Re-uptake, metabolism by MAO and COMT, and diffusion away from the synaptic cleft should have been discussed. An accurate diagram could be used to enhance the answer.
2017A 01 – 2014B 04
Outline the anatomy and physiology of the parasympathetic nervous system.
CICMWrecks Answer
Parasympathetic Nervous System
- The parasympathetic nervous system is one of the two main divisions of the autonomic nervous system (ANS).
- Its general function is to control homeostasis and the body’s rest-and-digest response.
- Control the body’s response while at rest. Acts as local brake
- Activates response of Rest and digest
Parasympathetic (Cranio-sacral) Efferents
- Arises from neurons in cranial (III, VII, IX, X) or sacral segments of spinal cord (S2~S4)
- Pre-ganglionic neuron
- Long fibre
- Ganglia located near or within effector organs
- Post-ganglionic neuron
- Short
- Release Acetylcholine
Cranial:
| Ganglion / Target Organ | Effect | |
|---|---|---|
| CN III | Ciliary ganglion from occulomotor nucleus | • Pupil constriction, lacrimation |
| CN VII | Chorda tympani Submaxillary ganglion | secretion of saliva |
| CN IX | Parotid gland | secretion of saliva |
| CN X | Respiratory: Pulmonary plexus | Bronchoconstriction increased mucous production |
| Cardiovascular: – SA node – AV node | ↓ inotropy (Atria > Vent) ↓↓↓ Chronotropy ↓ lusitropy (Atria > Vent) ↓↓↓ dromotropy | |
| stomach to proximal two-thirds of the transverse colon | Increased gastric motility, secretions Relaxation of pyloric sphincter |
Sacral:
| Ganglion / Target Organ | Effect | |
|---|---|---|
| 2nd, 3rd, 4th sacral segments | Hypogastric plexus – Descending colon – Rectum – Bladder – Uterus | Contracts muscular wall of rectum Relaxes internal sphincter of anus Contracts detrusor muscle |
Effector
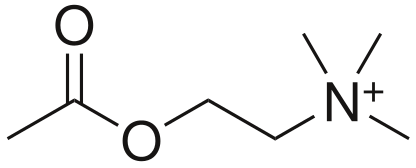
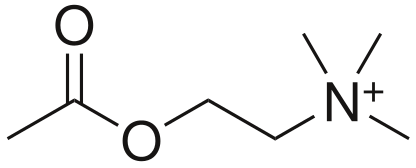
- Acetylcholine (CCOOCCNH3)
- Formed for Choline and Acetyl CoA
- Receptors
- Muscarinic
- G Protein Coupled
- Nicotinic
- Ligand gated ion channels
- Muscarinic
- Metabolism
- Acetylcholinesterase
Mooney / JC 2019
Examiner Comments
2017A 01: 0% of candidates passed this question.
Generally there was a lack of detailed knowledge, incorrect facts and at times confusion between the sympathetic and parasympathetic nervous system functions. A lack of anatomical detail was common (the origin of preganglionic cell bodies was not described clearly, and parasympathetic ganglia were not often named and located). It was expected an answer would mention the central role of Acetylcholine as a neurotransmitter at preganglionic and post ganglionic neurons in the parasympathetic system. Target organs were identified correctly but the exact action was not specified e.g. pupillary constriction vs. dilatation, GI sphincter/bladder – contraction vs. relaxation. Detail concerning receptor physiology was not required. This is a question covering a core topic that no candidate passed. An overview of the arrangement and function of the autonomic nervous system is provided in several core physiology texts, including Ganong and Guyton.
2014B 04: 0% of candidates passed this question.
Generally there was a lack of detailed knowledge, incorrect facts and at times confusion between the sympathetic and parasympathetic nervous system functions. A lack of anatomical detail was common (the origin of preganglionic cell bodies was not described clearly, and parasympathetic ganglia were not often named and located). It was expected an answer would mention the central role of Acetylcholine as a neurotransmitter at preganglionic and post ganglionic neurons in the parasympathetic system. Target organs were identified correctly but the exact action was not specified e.g. pupillary constriction vs. dilatation, GI sphincter/bladder – contraction vs.
relaxation. Detail concerning receptor physiology was not required. This is a question covering a core topic that no candidate passed. An overview of the arrangement and function of the autonomic nervous system is provided in several core physiology texts, including Ganong and Guyton.
2023B 20
Outline the anatomy (60% marks) and synaptic physiology (40% marks) of the vagus nerve.
CICMWrecks Answer
Vagus Nerve Anatomy
| Nuclei | Dorsal motor nucleus – sends parasympathetic fibers to the GI tract, lungs Nucleus ambiguus – sends efferent motor and parasympathetic fibers to the heart Solitary nucleus – receives special gustatory afferent from the tongue and visceral afferent fibers from organs Spinal trigeminal nucleus – receives general sensory afferent fibers from outer ear, dura of posterior cranial fossa, mucosa of larynx |
| Course | Exits brain from medulla oblangata – series of rootlets in retro-olivary groove → Travels laterally and exits skull via jugular foramen → Sensory ganglia consist of superior and inferior ganglionic swelling → Joined by cranial root of accessory nerve (CN XI) → Passes down the neck in carotid sheath (between Carotid artery and Internal Jugular Vein) → Enters thorax at base of neck → Left: travels ant to aortic arch, behind Lt main bronchus and into oesophagus → Right: travels behind oesophagus and Rt main bronchus →Both enter abdomen through oesophageal hiatus in diaphragm |
| Branches | In the jugular fossa: meningeal, auricular branches In the neck: pharyngeal, superior laryngeal, recurrent laryngeal nerves; superior cardiac branches In the thorax: inferior cardiac nerve, anterior bronchial branches, posterior bronchial branches, esophageal branches In the abdomen: gastric, celiac and hepatic branches |
| Field of innervation | General sensory afferent fibers – sensory information from larynx, auricle, external acoustic meatus, dura mater of the posterior cranial fossa General visceral afferent – information from the aortic body, esophagus, lungs, bronchi, heart, intestines Special afferent – information about taste General visceral efferent – parasympathetic division that simulates smooth muscle and glands of the pharynx, larynx, thoracic and abdominal organs. – Heart via cardiac plexus: SA node: Rt vagus. AV node, ventricles: Lt vagus. – Lungs via pulmonary plexus – Gut (from stomach to proximal to splenic flexure) via gastric plexus Branchial efferent – innervate muscles of mastication and tensor vali palatini |
| Communications | Trunk and ganglia with CN IX,XI,XII, superior sympathetic ganglion and 1st and 2nd cervical nerves Auricular branch with CN VII Pharyngeal plexus with IX and superior cervical ganglion Cardiac, pulmonary, oesophageal and gastric branches with sympathetic outflow to viscera (Superficial and deep Cardiac plexuses receives branches from cardiac nerves of vagus, recurrent laryngeal nerves and cervical ganglia of sympathetic trunk.) |
Physiology
- 75% of all parasympathetic fibres are in vagus nerve
- Pre-ganglionic fibre
- Long fibre
- Release Acetylcholine to stimulate post-ganglionic neuron at nicotinic ACh receptor
- activation is tonic
- Ganglia located near or within effector organs
- Post-ganglionic fibre
- Short
- Release Acetylcholine to stimulate muscarinic ACh receptor
Effector
- Acetylcholine (CCOOCCNH3)
- Formed for Choline and Acetyl CoA
- Receptors
- Muscarinic
- G Protein Coupled
- Nicotinic
- Ligand gated ion channels
- Muscarinic
- Metabolism
- Acetylcholinesterase
Muscarinic ACh receptor
- Known as muscarinic because muscarine also agonises this receptor
- Metabotropic, G-protein coupled
- Phosphorylate various second messengers
- Mediate slow metabolic response via second messenger cascades
- 5 subtypes: M1-M5
- M1,M3,M5 – excitatory (Gq: IP3/DAG → ↑Ca++)
- M2, M4 – Inhibitory (Gi: ↓cAMP)
- Receptor at parasympathetic postganglionic terminals
- M1: ANS
- M2: Cardiac
- M3: Lungs
| Ganglion / Target organ | Receptor | Signal | Effect |
|---|---|---|---|
| Respiratory: Pulmonary plexus | M3 (Gq) | IP3/DAG ↑Ca++ | Bronchoconstriction increased mucous production |
| Cardiovascular: – SA node – AV node | M2 (Gi) | ↓cAMP ↑ K+(G) | ↓ inotropy (Atria > Vent) ↓↓↓ Chronotropy ↓ lusitropy (Atria > Vent) ↓↓↓ dromotropy |
| stomach to proximal two-thirds of the transverse colon | M1 (Gq) | IP3/DAG ↑ Ca++ | Increased gastric motility, secretions Relaxation of pyloric sphincter |
Examiner Comments
2023B 20: 25% of candidates passed this question.
The vagus nerve anatomy was best broken down into a description of the fibers it carries (visceral, parasympathetic and somatic sensory fibres) and then origin and course from the parasympathetic, sensory and motor nuclei in the medulla as the tenth cranial nerve to its branches; the pharyngeal, cardiac, pulmonary and laryngeal branches. Pre and post-ganglionic physiology involved a detailed description of the Muscarinic Ach receptor and events. This would also include the 5 subtypes of the muscarinic receptor, with the locations and downstream effects of the M1-M3 locations being the most important to note.
M2. Pharmacology of the Autonomic Nervous System
i. Understand the pharmacology of drugs acting upon the autonomic nervous system.
2019B 19
Describe the pharmacology of atropine.
Examiner Comments
2019B 19: 53% of candidates passed this question.
Most candidates used a good structure to compose their answer. Better candidates understood that CNS effects occur as atropine is a tertiary amine that crosses the blood brain barrier. The mechanism of action was required. Indications for use should have included bradycardia, organophosphate poisoning, drying of secretions etc. Reasonably extensive details regarding pharmacodynamics was expected, including potential toxic effects. There was limited knowledge regarding pharmacokinetics.
2011A 03
Compare and contrast the pharmacology of intravenously administered atropine and glycopyrrolate
Examiner Comments
2011A 13: 6 (50%) of candidates passed this question.
Most candidates exhibited a structural approach with reasonable understanding of the pharmacology of atropine although there was a lack of precision (anticholinergic is correct, competitive muscarinic antagonist is more precise). Some answers did not contrast glycopyrrolate adequately. The phrase ‘hepatic metabolism, renal excretion’ needed to be accompanied with detail if marks were to be awarded.
2018A 14
Classify anticholinesterase drugs according to chemical interaction with an example of each (30% of marks). Outline the pharmacodynamic effects of anticholinesterase drugs and their clinical indications (70% of marks).
2015A 21
Describe the pharmacodynamic effects and indications for the use of anticholinesterase drugs.
CICMWrecks Answer
Background
- Acetylcholinesterase (AChE) is an enzyme that hydrolyse acetylcholine (ACh) into choline & acetate
- AChE is found in synaptic clefts and is responsible for the termination of synaptic transmission
- Common action of anti-cholinesterases = allow build up of Ach and prevent it from being destroyed.
Naturally Occuring Cholinesterases
Two types of naturally occurring cholinesterases:
- Achesterase – nerve endings & in RBCs
- Non-specific or pseudocholinesterases – destroy other esters – tissues & plasma
Anticholinesterase drugs
AntiAchE drugs are administered in anaesthesia when spontaneous recovery from NDNMB is occurring to accelerate it.
Classification:
Drugs are classified by the way in which they inhibit the activity of AchE.
3 main types of anticholinesterase:
- Reversible antagonist via electrostatic binding
- ie. edrophonium
- causes electrostatic attachment to the anionic site of the enzyme -> stabilising the H+ bond at the esteratic site -> edrophonium-AchE complex prevents Ach from binding
- Reversible antagonist via covalent bonding [Formation of carbamyl esters (carbamates)]
- ie. neostigmine, physostigmine & pyridostigmine
- antagonise AchE enzyme by being competitive substrate for Ach -> forms a carbamyl-ester complex at the esteratic site of enzyme.
- longer lasting bond (15-30min)
- Irreversible antagonist via covalent bonding
- ie. organophosphate anticholinesterase drugs (echothiopate), insecticides & nerve gases
- combine with Ach at the esteraic site to form a stable covalent bond -> does not undergo hydrolysis.
- synthesis of a new AchE is required.
Pharmacodynamic effects
Anticholinesterase drugs inhibit AChE, thereby increase the concentration of ACh at both nicotinic and muscarinic ACh receptors
Muscarinic effects occur at lower doses than nicotinic effects
Muscarinic effects
- CVS – bradycardia ± hypotension
- RESP – bronchoconstriction ± bronchospasm
- CNS – miosis, cholinergic syndrome – confusion, agitation, nausea/vomiting
- GIT – hypersalivation, ↑GIT motility, nausea/vomiting, diarrhoea
- GUT – urination, incontinence
- OTHER – lacrimation, diaphoresis
Mnemonic: SLUDGE-BM: Salivation/Sweating, Lacrimation, Urination, Diaphoresis/Diarrhoea, GI upset, Emesis, Bradycardia/bronchospasm, Miosis
Nicotinic effects
- Reversal of non-depolarising neuromuscular blockers
- Prolongs effect of suxamethonium (depolarising NMB)
- Anticholinesterase overdose → excess synaptic ACh → depolarisation block ± fasciculation
Clinical uses
- Reversal of non-depolarising neuromuscular blocker
- Mechanism – anticholinesterase drugs ↑ synaptic ACh → competes with ND-NMB in synapse for nAChR → reversal of neuromuscular block
- Drugs – usu. neostigmine, administered together with glycopyrrolate or atropine
- Diagnosis and treatment of myasthenia gravis
- Mechanism – anticholinesterase drugs ↑ synaptic ACh → competes with myasthenia auto-antibodies for post-synaptic nAChR → ↑muscle strength
- Drugs – e.g. edrophonium for diagnosis, pyridostigmine for maintenance
- Treatment of cognitive impairment in neurodegenerative diseases (e.g. Alzheimer’s disease, Lewy body dementia, etc)
- Mechanism – ↑ synaptic ACh in CNS → ↑ cholinergic transmission
- Drugs – e.g. rivastigmine, galantamine, donepezil
- Treatment of glaucoma
- Mechanism – constriction of sphincter pupillae and ciliary muscles → miosis → facilitate outflow of aqueous humor → IOP decreases
- Drugs – e.g. echothiophate eye drops, physostigmine
- Treatment of anticholinergic syndrome
- Anticholinergic syndrome caused by: anti-histamines, anti-parkinsonians, atropine, anti-spasmodics, mydriatics, skeletal muscle relaxants, plants
- CLINICAL FEATURES: delirium, tachycardia, dry and flushed skin, dilated pupils, myoclonus, hyperthermia, urinary retention, bowel sounds, seizures, dysrhythmias(tachy)
- Mechanism – increase synaptic ACh
- Drugs – e.g. physostigmine (tertiary amine + lipophilic → readily crosses BBB)
JC 2019
Examiner Comments
2018A 14: 32% of candidates passed this question.
Many candidates who scored poorly confused anticholinesterase drugs with anticholinergic drugs. Some described pharmacokinetics when it was not asked. Similarly, treatment of organophosphate poisoning and/or cholinergic crisis was not asked for in the question.
2015A 21: 25 % of candidates passed this question.
It was expected the answer would provide a structured approach to describing the pharmacodynamics (what the drug does to the body) of this discreet class of drugs. A brief acknowledgement of the drugs in this class followed by a catalogue of the various clinical uses of this class of drugs would be a good start. If this was followed up with a description of the effects of these drugs on the CVS, GIT, Salivary glands, eye, NMJ and the lungs a good mark would have been awarded.
A number of candidates described the actions at the receptors in detail which did not attract marks. The extensive range of clinical uses for this class of drugs was poorly appreciated. Few answers demonstrated any understanding of the PD effects of the drug class. There was generally a good knowledge of representative drugs within this class. Failing to achieve a pass mark reflected scant/brief answers that just did not cover enough of the expected material.
2009A 20
Describe the pharmacological basis of the management of organophosphate poisoning.
CICMWrecks Answer
Organophosphate posisoning
SOURCE – insecticides, exposure to nerve agents (most commonly seen in farming settings)
PATHOPHYSIOLOGY
- Organophosphates form a covalent bond with acetylcholinesterase, inhibiting the metabolism of acetylcholine.
- This results in high levels of Ach at the neuromuscular junction (both nicotinic and muscarinic receptors), causing a cholinergic crisis
SYMPTOMS
- SLUDGE (salivation, urination, defaecation, gastrointestinal motility, emesis)
- CNS – confusion, anxiety, tremors, seizures
- CVS – bradycardia, hypotension
- RESP – respiratory impairment due to muscle weakness, difficulty clearing secretions
MANAGEMENT
- Remove the patient from the source of poisoning
- PPE for staff – mask, goggles, neoprene gloves and gowns rather than latex as hydrocarbons can penetrate latex
- ABC’s and resuscitation as required
- Decontamination –
- activated charcoal / gastric lavage / whole bowel irrigation unlikely to be effective due to rapid absorption of organophosphates.
- Clothes should be removed and discarded and the patient bathed with soap and water to remove organophosphates from skin.
- Irrigate the eyes if ocular exposure has occurred.
- Symptom control
- Anti muscarinic agents –
- atropine in large doses will reduce the antimuscarinic effects by competitively antagonizing Ach at the receptor.
- ETG suggests 1.2-3mg boluses, aiming SBP>80mmHg, HR >80bpm and absence of wheeze, doubling the dose every 5 mins until atropinisation is achieved, followed by an infusion.
- Glycopyrrolate can be used to reduce secretions post initial atropinisation, however does not cross the BBB so will have no effect on the central cholinergic effects
- There is no antinicotinic agent so supportive care only for muscle weakness.
- Benzodiazepines for seizure control
- Anti muscarinic agents –
- Definitive treatment
- Cholinesterase regenerator (an oxime such as pralidoxime) may reactive AchE and prevent the organophosphate-acetylocholinesterase complex ageing and becoming an irreversible bond if given within 48 hrs
Examiner Comments
2009A 20: Pass rate: 40%
Organophosphates (OGP) bind irreversibly to acetyl cholinesterase. They produce a cholinergic crisis and muscle paralysis due to excess Acetyl choline (ACh) at all muscarinic and nicotinic receptors.
Candidates were required to discuss the pharmacology relevant to treating OGP poisoning, including active decontamination/staff protection due to high lipid solubility, use of antimuscarinics with central and peripheral action to treat cholinergic symptoms, supportive therapy for muscle weakness (there is no antinicotinic agent available which does not exacerbate muscle weakness), and finally the use of the cholinesterase regenerator, Pralidoxime, which may prevent the OGP-AChE complex ageing and becoming an irreversible bond if given in a timely fashion.
Good answers included a discussion of the mechanism of action of the therapeutic agents, the time course of therapy, the large doses/infusions of atropine required and the titration of therapy to reversal of muscarinic effects. Long lists of signs and symptoms were not required to pass this question.
Syllabus H2b2c
Reference: Rang Dale Ritter 6th edition p 164-166, Katzung 10th edition p 116-117, 968.

Recent Comments