Syllabus (Fourth Edition, 2023)
Topics
i. Describe the measurement of intracranial pressure.
Topics not covered in previous SAQs
.
Learning Objectives for the First Part Examination in Intensive Care Medicine
- This will ensure that trainees, tutors, and examiners can work from a common base.
- All examination questions are based around this Syllabus.
- These learning objectives are designed to outline the minimum level of understanding required for each topic.
- The accompanying texts are recommended on the basis that the material contained within them provides sufficient information for trainees to meet the learning objectives.
- Trainees are strongly encouraged to explore the existing and evolving body of knowledge of the Basic Sciences as they apply to Intensive Care Medicine by reading widely.
- For all sections of the syllabus an understanding of normal physiology and physiology at extremes of age, obesity, pregnancy (including foetal) and disease (particularly critical illness) is expected.
- Similarly, for pharmacology, trainees are expected to understand a drug’s pharmacology in these contexts.
- An understanding of potential toxicity and relevant antidotes is also expected.
Definitions
Throughout the document specific wording has been used under the required abilities to indicate the level of knowledge and understanding expected and a glossary of these terms is provided.
Definitions
| Calculate | Work out or estimate using mathematical principles. |
| Classify | Divide into categories; organise, arrange. |
| Compare and contrast | Examine similarities and differences. |
| Define | Give the precise meaning. |
| Describe | Give a detailed account of. |
| Explain | Make plain. |
| Interpret | Explain the meaning or significance. |
| Outline | Provide a summary of the important points. |
| Relate | Show a connection between. |
| Understand | Appreciate the details of; comprehend. |
SAQs
i. Describe the measurement of intracranial pressure.
2022A 10 – 2016B 18
Discuss the determinants of intracranial pressure (80% of marks).
Outline how it can be measured (20% of marks).
CICMWrecks Answer: ICP
Definition:
- ICP: hydrostatic pressure within the cranial vault
- Normal value is 5-15 mmHg
- focal ischaemia when ICP > 20 mmHg
- global ischaemia when ICP > 50mmHg
Munro-Kellie Doctrine
- The rigid and closed cranial vault forms a fixed brain volume containing
- Brain parenchyma (80%, 1400 g)
- CSF (10%; 75 mL)
- Cerebral blood and vessels (10%; 75 mL)
- Δ’s in volume of any components → Δ’s in others or and increase in ICP
CSF Production / Absorption
CSF Production:
- 60-70% of the CSF is formed by the choroid plexuses
- 30-40% by the cerebral vessels lining the ventricular walls
- Normal rate is 20mL/hour
- Formation independent of ventricular pressure
- Mechanism
- From Coroid Plexus by net transport of Na+, K+, Cl-, HCO3- and water, from plasma to ventricles
- Na down Conc grad
- Others down electro chem grads
CSF Absorption:
- Absorbed through the arachnoid villi into the cerebral venous sinuses
- Absorption by bulk flow, is proportional to ventricular pressure
- If pressure < 7 cmH2O, CSF absorption ceases
- Above 7cmCSF absorption is linear
- At approximately 11 cmH2O, CSF Absorption = Formation

Control of ICP
- ICP is regulated via volume buffering
- i.e. increase in volume of one intracranial component leads to compensatory decrease in volume of other intracranial components
- When volume buffering mechanism is exhausted → rapid increase in ICP (decompensation)
- Movement of cerebral venous blood = rapid compensation, lower capacity
- Movement of CSF = gradual compensation, larger capacity
Determinants of ICP:
- Brain
- Age / Mass
- Space occupying lesions
- Cerebral Oedema
- CSF
- CSF production
- CSF Absorption
- Cerebral Blood Volume
- Cerebral autoregulation: Flow-metabolic coupling
- Cerebral metabolic rate
- Increase in systemic blood pressure / flow
- Venous Outflow obstruction
- Vasoactive agents
- Monro-Kellie Doctrine
- Loss of above – e.g. Fractures, surgery
Compensation for Elevated ICP (Intracranial Pressure)
Early compensation
- Δ CSF distribution and flow
- CSF is displaced to spinal subarachnoid space
- ↑’d resorption rate
Late compensation
- ↑ ICP → ↓ CBF → ↓ in cerebral blood volume → cerebral ischaemia
Decompensation
- ↑ICP → ↓ in cerebral tissue volume → brain herniation
- Cushing Reflex
- Hypertension, bradycardia and abnormal breathing associated with raised ICP
- Mechanism:
- Stage 1:
- ↑ ICP → ↓ blood supply to vasomotor area → Local hypoxia/hypercarbia → ↑ SNS >> ↑ PSPS vasomotor stimulation
- ↑ TPR → ↑ MAP
- ↑ HR → ↑ CO
- → compensatory ↑CBF
- Stage 2:
- ↑ CO → Baroreceptor stimulation → ↑ Vagus nerve stimulation → Bradycardia and ↓ contractility.
- Stage 1:
Gladwin / JC 2020
CICMWrecks Answer: Measurement of ICP
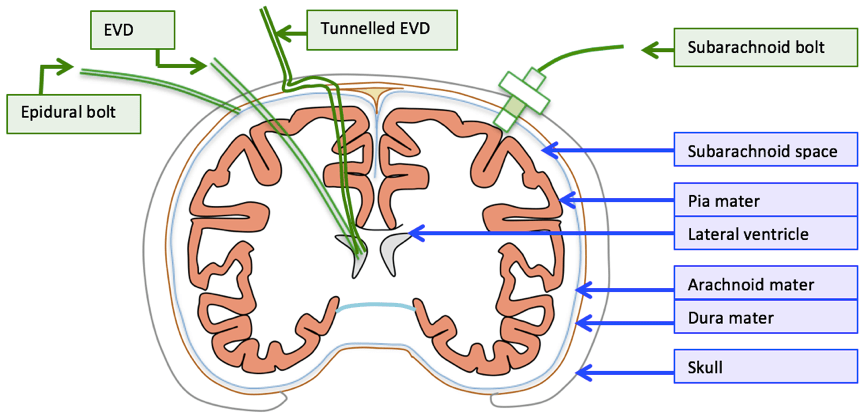
Methods of Measurement of ICP (Outline)
Invasive
| Method | Advantages | Disadvantages |
|---|---|---|
| Intraventricular catheter (EVD) | Provides ‘ture’ global ICP Allows for CSF drainage and administration of drugs In-vivo calibration possible via external pressure transducer | Infection Difficult iinsertion |
| Epidural catheter | Ease of insertion Minimal risk of infection (no penetration of dura) | Low accuracy |
| Lumbar CSF puncture | Extracranial procedure Can be performed ambulatory | May not reflect ICP Dangerous if ICP high |
| Catheter-tip micro transducers (subdural or intra-parenchymal) | Rare complications during procedure Low risk of infections Can be made permanent implants | Drift of transducer output over time In-vivo calibration not possible Inaccurate if intraparenchymal gradient exists |
Non-Invasive
Non-invasive methods like pupillometry, CT, MRI, TCD provide an adjunct to clinical examination of high ICP, but are not a surrogate for invasive ICP measurement.
Gladwin / JC 2020
Examiner Comments
2022A 10: 64% of candidates passed this question.
In the good answers to this question, and there were a number, the candidates included the volumes of the cranium and a correct description of the Monroe Kellie doctrine. A good answer should have included the compensations and consequences of increases in intra-cranial volumes; a discussion of all three components (brain tissue, blood, and CSF) and how they affect intracranial pressure; and then information on intra-ventricular and parenchymal devices in measuring ICP, briefly including their pros and cons. A common issue was writing quite a lot more than was needed on the relationship of cerebral blood flow to cerebral blood volume, and/or on the physiological consequences of raised ICP, which seemed to leave little time for discussion elsewhere. A few candidates did not provide any response for ICP measurement (worth 20% of the marks). Few candidates provided the intra-cranial elastance equation. A significant proportion of candidates missed out a part of the question, either the factors that affect CBV or ICP measurement.
2016B 18: 55% of candidates passed this question.
It was expected answers would include an explanation of the Monro-Kellie Doctrine. Many candidates gave insufficient details of compensatory mechanisms especially regarding decreased total cerebral blood volume (primarily venous) in response to increased intracranial pressure.
Most candidates had all the information but had difficulty synthesising the information to write a cohesive answer. Factors affecting ICP could be divided into factors affecting CBV, factors affecting CSF and factors affecting brain tissue. Under factors affecting CBV the effect of blood gases, autoregulation, temperature, metabolism, drugs and venous obstruction could have been detailed.
2020B 07
Compare and contrast external ventricular drains and intraparenchymal fibreoptic pressure monitors.
CICMWrecks Answer
| EVD | Intraparenchymal fiberoptic | |
| Description | • A flexible plastic catheter placed inside the lateral ventricles. • Can be either unilateral or bilateral placement • Gold standard for ICP monitoring | A think catheter inserted into parenchyma of the brain |
| Indication | • Hydrocephalus • Post surgical/trauma intracranial haemorrhage • Meningitis | same |
| Location of tip | Lateral ventricles | Below the dura – usually a few cms |
| Component | • Plastic catheter • Wheatstone bridge • Fluid filled non-compressible tubing • Pressurized fluid bag • Drainage bag • Monitor | • Microsensor – intracranial • Fiber Optic cable • Monitor |
| Principle | Pressure is transmitted to a Wheatstone bridge transducer via fluid filled non-compressible tubing | Changes in ICP move a displaceable mirror at the tip of the sensor to alter the intensity of light reflected back along the fiber optic cable |
| calibration | Able to be zero’d post insertion | Cannot be zero’d post insertion |
| Sources of error | • Migration of catheter • Blockage • Incorrect leveling to tragus • Damping and resonance | • “Drift” • Increased inaccuracy >72hrs • Only measures ICP locally |
| Advantage | • Has diagnostic values (CSF sampling, elevated ICP, new haemorrhage) as well as therapeutic values (drainage of excessive CSF, administration of medication) • Global measurement of ICP • Can be converted to cerebral shunt – long term treatment • Cheap | • Less expertise required for insertion • Less traumatic • Able to be placed in patients with small collapsed ventricles • Less infection risk • No risk of blockage |
| Disadvantage | • More skill required for insertion • More traumatic compared to bolt • Increased risk of ventriculitis • May be blocked • Complications: bleeding, malplacement, obstruction, migration, infection | • Only local ICP is measured • No therapeutic value: CSF cannot be drained • Less accurate due to drift and unable to be calibrated post insertion • Expensive |
Guo 2021
Examiner Comments
2024A 18: 38% of candidates passed this question.
This question required an accurate explanation of the mechanism of measurement for each device. A head to head comparison of the differences and similarities in utility, accuracy, global versus regional measurements, calibration, drift and dampening should follow. A comparison of potential complications was also expected.
2020B 07: 22% of candidates passed this question.
This question is ideally suited to a tabular format, where candidates are expected to highlight the significant similarities and differences as well as why a certain monitor may be chosen in preference to another rather than compile two lists written next to each other. To score well in this question, a statement of what could be measured (ICP: global vs local), a description of the measurement principles, along with other measurement related information like calibration and sources of error was required. Also sought was information regarding anatomical placement (e.g., lateral ventricle for EVD) and method of placement. Furthermore, a comparison with each other (e.g., higher infection/bleeding risk with EVD, greater risk of trauma due to size and insertion, expertise to insert, cost, therapeutic benefit, risk of blocking) was required for completion. Candidates who structured these elements into advantages and disadvantages were generally able to elucidate this information and score better.


Recent Comments