Syllabus (Fourth Edition, 2023)
Topics
i. Describe the anatomy of the heart including the chambers, valves, pericardium, and the orientation of the heart.
ii. Describe the coronary circulation and its regulation.
iii. Describe the structure and functional significance of the excitatory, conductive, and contractile elements of the heart.
iv. Describe the normal pressure and flow patterns of the cardiac cycle.
v. Describe the foetal circulation.
vi. Describe the circulatory and respiratory changes that occur at birth.
Topics not covered in previous SAQs
i. Describe the anatomy of the heart including the chambers, valves, pericardium, and the orientation of the heart.
iii. Describe the structure and functional significance of the excitatory, conductive, and contractile elements of the heart.
iv. Describe the normal pressure and flow patterns of the cardiac cycle.
Learning Objectives for the First Part Examination in Intensive Care Medicine
- This will ensure that trainees, tutors, and examiners can work from a common base.
- All examination questions are based around this Syllabus.
- These learning objectives are designed to outline the minimum level of understanding required for each topic.
- The accompanying texts are recommended on the basis that the material contained within them provides sufficient information for trainees to meet the learning objectives.
- Trainees are strongly encouraged to explore the existing and evolving body of knowledge of the Basic Sciences as they apply to Intensive Care Medicine by reading widely.
- For all sections of the syllabus an understanding of normal physiology and physiology at extremes of age, obesity, pregnancy (including foetal) and disease (particularly critical illness) is expected.
- Similarly, for pharmacology, trainees are expected to understand a drug’s pharmacology in these contexts.
- An understanding of potential toxicity and relevant antidotes is also expected.
Definitions
Throughout the document specific wording has been used under the required abilities to indicate the level of knowledge and understanding expected and a glossary of these terms is provided.
Definitions
| Calculate | Work out or estimate using mathematical principles. |
| Classify | Divide into categories; organise, arrange. |
| Compare and contrast | Examine similarities and differences. |
| Define | Give the precise meaning. |
| Describe | Give a detailed account of. |
| Explain | Make plain. |
| Interpret | Explain the meaning or significance. |
| Outline | Provide a summary of the important points. |
| Relate | Show a connection between. |
| Understand | Appreciate the details of; comprehend. |
SAQs
i. Describe the anatomy of the heart including the chambers, valves, pericardium, and the orientation of the heart.
2023B 02
Outline the anatomy of the cardiac ventricles including the chambers, valves and conduction elements.
2019B 16
Compare the structure, function and coronary circulation of the right and left ventricles.
CICMWrecks Answer: Anatomy (Rt vs Lt)
RIGHT
VENTRICLE
LEFT
VENTRICLE
| Pathway | |
| RA → tricuspid valve → RV → pulmonary valve → Pulmonary trunk | LA → Mitral valve → LV → Aortic valve → Aorta |
| Valves | |
| TV: 3 triangular cusps (medial anterior, inferior) attached by the base to fibrous ring of TV orifice. Papillary muscles connect trabeculae to cusps PV: 3 cusps (posterior, right anterior, left anterior) | MV: large anterior and small posterior cusp Attach to 2 large papillary muscles (anterolateral, posteromedial) by chordae tendinae AV: 3 semilunar cusps (Rt posterior, left posterior, anterior). Aortic sinuses above |
| Portions | |
| Septal portion: 1) the inflow tract: supports the tricuspid valve, Inferior aspect have ‘trabeculae carnae’ 2) Infundibuloventricular crest: muscular, lies between AV and pulmonary orifices – separates inflow and outflow 3) the outflow tract (infundibulum) – smooth walled, directed up+right towards pulm trunk | Portions: 1) Large trabeculated sinus portion with MV 2) Small smooth outflow tract that supports AV located anterior to the anterior mitral leaflet and is part of the atrioventricular (AV) septum. |
| Rest | |
| Rest of RV wall is trabecular Moderator band: muscular bundle crossing ventricular cavity from Intrerventricular septum to anterior wall – conveys right branch of AV bundle to the ventricular muscle | Wall: thick trabeculae carnae mostly. Exception of fibrous vestibule immediately below aortic orifice The free wall and apical half of the septum contain fine internal trabeculations. |
| Dimension | |
| The wall of the right ventricle is thinner than that of the left (1/3rd) Thickest at base, thinner towards apex Cavity size 85ml (=LV) | Wall 3x the size of RV Cavity size equal |
| Functions | |
| Receives deoxygenated blood from RA Pumps into pulmonary circulation | Receives oxygenated blood from LA Pumps into aorta → systemic circulation |
| Main Function | |
| maintain adequate pulmonary perfusion pressure to deliver desaturated venous blood to the gas exchange membranes of the lungs maintain low systemic venous pressure to prevent tissue and organ congestion | Maintain adequate systemic perfusion pressure to deliver oxygenated blood to tissue |
| Pressures | |
| RV Sys 15-30 | LV Sys 100-140 |
| RV Dias 4-12 | LV Dias 3-12 |
| RVEDD 10-26mm | LVEDD 36-56mm |
| RVESD 10-26mm | LVESD 20-40mm |
Sources: Last’s Anatomy, Aneskey.com, Anatomy for anaesthetists
JC 2019
CICMWrecks Answer: Coronary Circulation (Rt vs Lt)
RIGHT
VENTRICLE
LEFT
VENTRICLE
- Supply:
- Right coronary artery and its branches
- conus artery supplies the infundibulum
- acute marginal arteries supply the anterior free wall
- posterior descending artery via septal branches supply the posterior 1/3 IV septum (PDA arises from RCA in Right dominant circulation and LCx in Left dominant circulation
- the other 2/3 of the IV septum is supplied by septal branches of the left anterior descending artery
- Supply: Left Main Coronary
- LAD (supplies the free wall and most of the papillary muscles)
- Diagonals
- Septal perforators
- LCx: inferolateral LV wall
- Obtuse Marginal branches
- LAD (supplies the free wall and most of the papillary muscles)
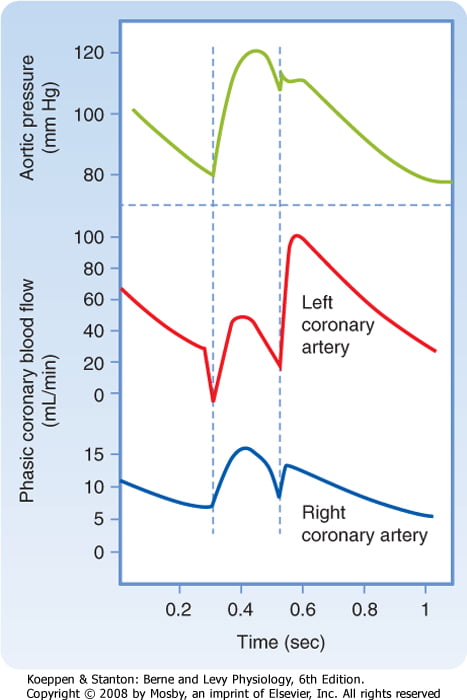
- RV Coronary blood flow
- RV pressures are low during both systole and diastole.
- flow during both systole and diastole
- LV Coronary blood flow
- The pressure inside the left ventricle is slightly higher than in the aorta during systole.
- Flow predominantly during diastole.
- Subendocardial flow ceases during systole.
Sources: Last’s Anatomy, Aneskey.com, Anatomy for anaesthetists
JC 2019
Examiner Comments
2023B 02: 11% of candidates passed this question.
This question expected an outline of the anatomy of the cardiac ventricles. Candidates that broke down the anatomy into subsections with correct and clear descriptions of each component were most successful. A potential structure to approach this question is included below;
– position, orientation, relations and characteristics of the chambers including ventricular interdepence
– internal ventricular structures including muscle type, septum, trabeculae, papillary muscules, infundibulum and moderator band
– valves and valvular rings’ position, structure and attachments
– conduction elements position and divisions
– blood and nerve supply
2019B 16: 27% of candidates passed this question.
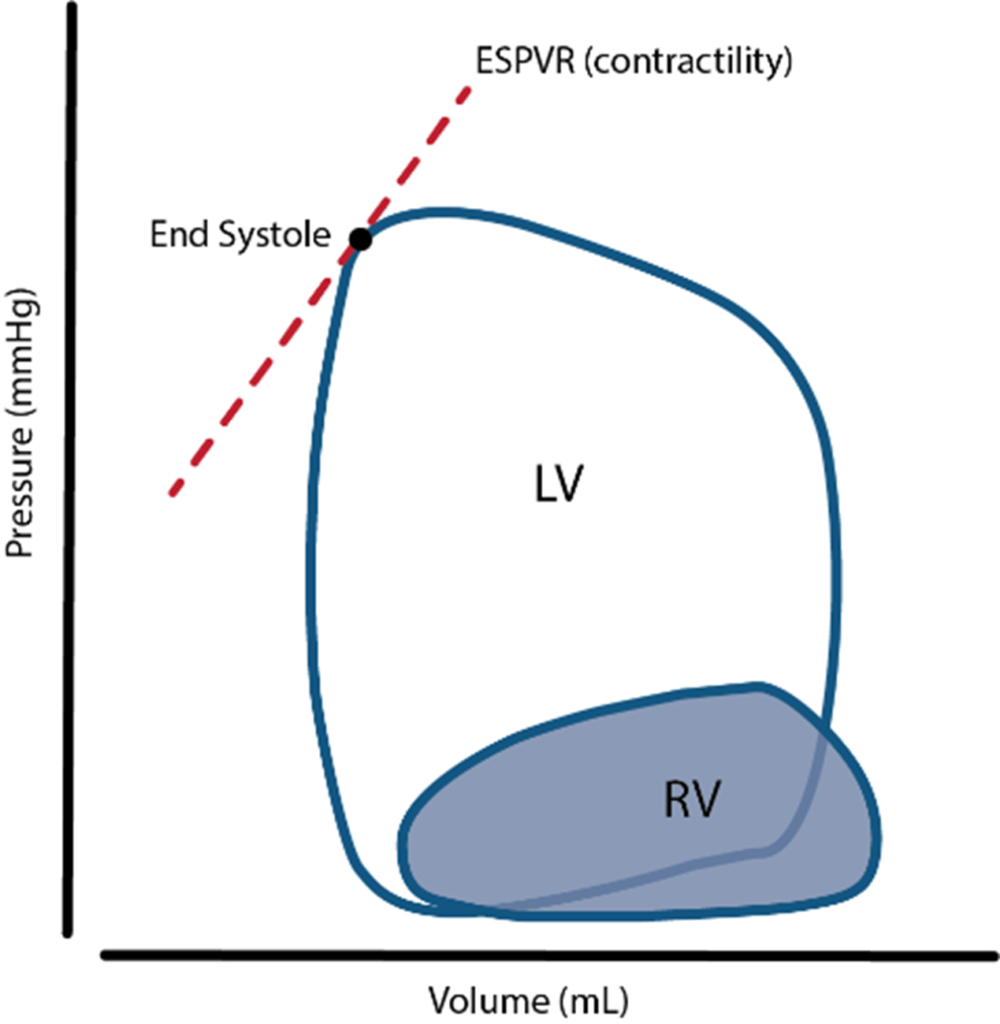
The question sought information on the structure (anatomy), function (physiology) and vascular supply of the right and left ventricle. Good answers provided detail in each section e.g. values for ventricular pressure rather than simply stating “high- and low-pressure systems”. Many marks may be gained by a simple anatomical description & labelled PV loop for each ventricle. Many candidates focussed solely on the coronary circulation, to which only a proportion of the marks were allocated.
ii. Describe the coronary circulation and its regulation.
See above for Coronary circulation of Right vs Left Ventricles
2023A 15 – 2021A 19 – 2014B 10
Describe the adult coronary circulation (50% marks) and its regulation (50% marks).
2018A 11
Describe the regulation of the coronary circulation.
2008B 11
Describe the adult coronary circulation (50% of marks).
Describe the physiological control of the coronary circulation (50% of marks).
CICMWrecks Answer
Arteries
- LCA to
- LCx to
- OM1
- OM2
- LAD has branches
- Diagonal 1 or 2
- LCx to
- RCA
- Right Ventricular
- Acute Marginal
- Posterior descending
Veins
- Great, small, middle
- Drain into the thebesian veins → ventricles directly
- Empty into the coronary sinus on the posterior wall or the RV
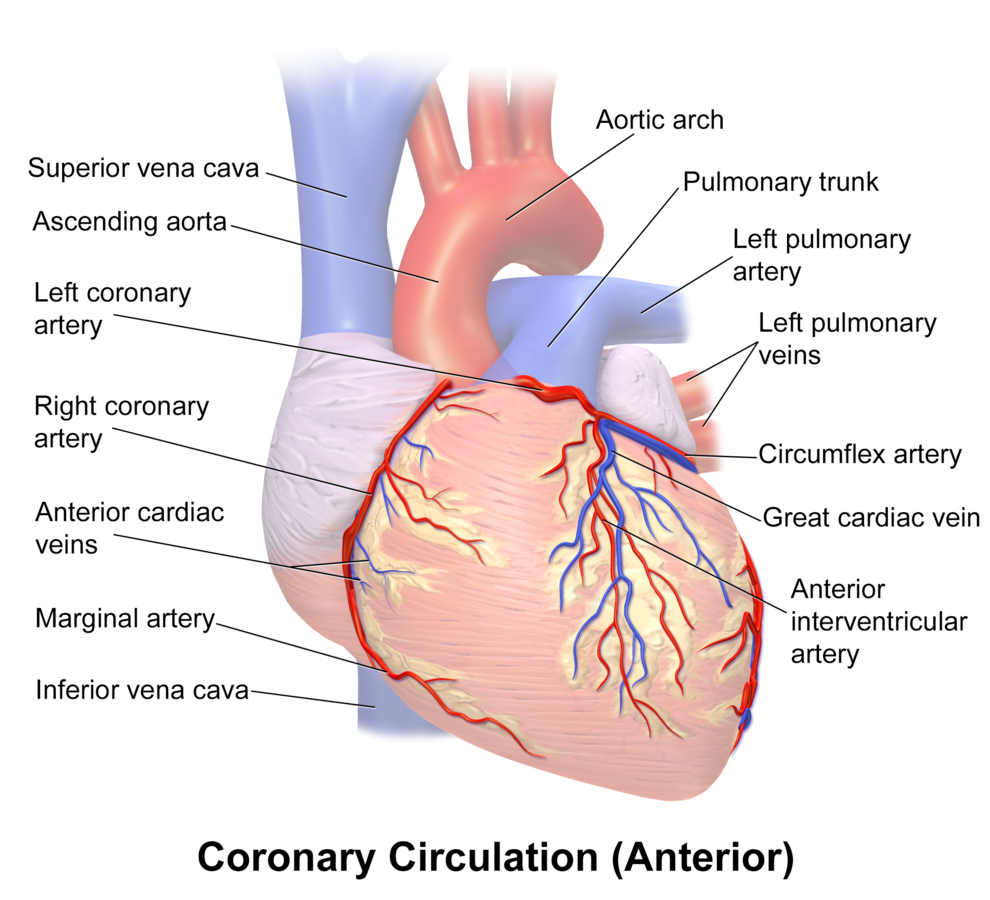
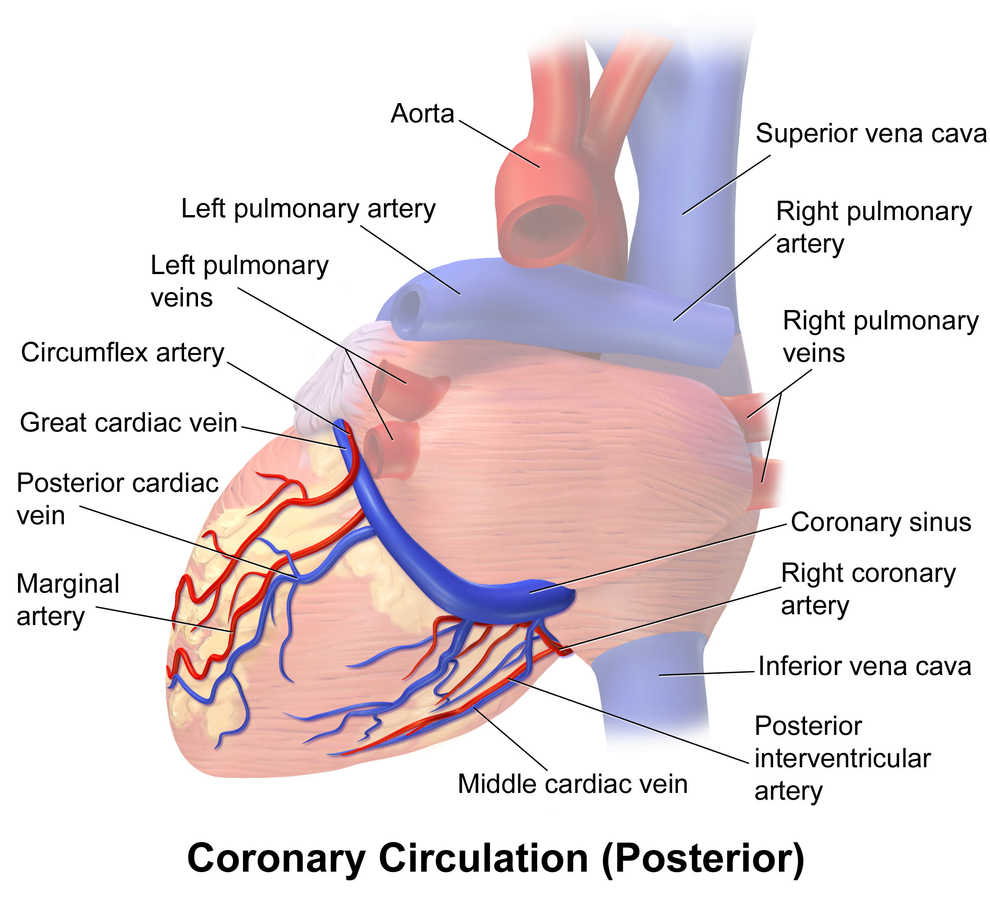
Regional Supply
| Artery | Anatomical region | ECG abnormality on occlusion |
|---|---|---|
| RCA | Down Anterior aspect of the heart, right of the pulmonary trunk Supplies RA SAN and AVN Posterior IVS | RCA occlusion causes → inferior: 2,3 aVF → true posterior: tall R in V1 |
| LCA | Left coronary artery ostia adjacent to left leaflet → Left Main → LCx and LAD Supplies LA, LV IVS AV Bundles | LCA occlusion → Lateral: 1, aVL, V1-V6 |
| LCx | LA and superior LV | anterolateral leads (1, aVL, V5 and V6) |
| LAD | RV, LV Anterior 2/3rds Interventricular Septum | Anteroseptal (V1 and V2) Anteroapical (V3 and V4) with some RCA supply. |
| Left Marginal | The continuation of the LCA after LAD branch Supplies LV laterally | Isolated Abnormalities rare V5, V6 |
| Right Marginal | The anterior branch of the RCA along the inferior border Supplies right ventricle and apex | Isolated Abnormalities rare RCA occlusion causes 2,3 aVF |
Coronary Blood Flow
- 80 mL/min/100 g
- or 200-250 mL/min
- 5% of CO at rest
- Can increase by 3-4 times (up to 400mL/min/100g)
High Extraction Ratio
High at rest (55-65%) body average of 25%
- Extraction ratio can only rise by factor of < 2 to 90%
- AV Δ O₂ = 11 mL/dL
- Coronary venous O₂ content = 5 mL/dL
- Coronary sinus SpO₂= 20mmHg
Coronary perfusion pressure (CPP)
- ADP = Ao Diastolic Prssure
- It is different throughout the cycle and b/w ventricles
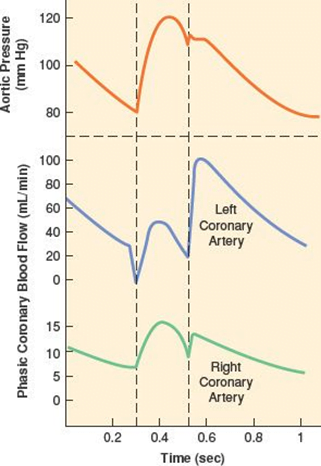
Phasic Supply as per diagram.
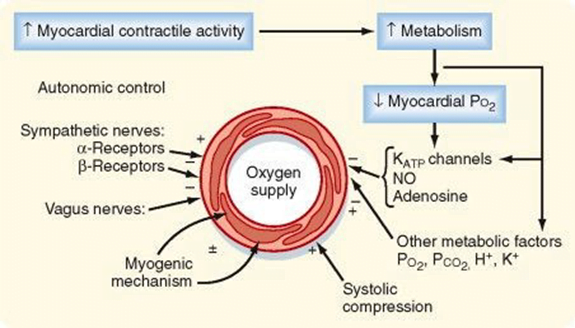
Determinants of Coro BF
- Physical Factors
- Extravascular compression (CPP factors)
- Neural and Neurohumoral Factors
- ↑ SNS tone →
- α receptor mediated vasoconstriction
- β receptor mediated vasodialtion
- ↑ force and rate of contractions → ↑ vasodialtor metabolite release
- Overall effect is dilation
- ↑ PSNS tone → KACh stimulation → mild ↓ Coronary vascular resistance
- ↑ SNS tone →
- Metabolic Factors (main)
- Vasodilatory
- ↑ Adenosine, H, K, CO2, Lactate
- NO → GTP
- ↑ O2 demand → ↓ ATP → ↑KATP channel activation → hyperpolarisation → vasodilation
- Vasodilatory
- Myogenic autoregulation (keep CPP 60-180 mmHg)
Gladwin 2016
Examiner Comments
2023A 15: 66% of candidates passed this question.
For this question a good answer should have encompassed a description of the following components; the arterial supply (epicardial, endocardial supplies), venous supply (major and minor venous drainage), the phasic ventricular blood supply, a description of and the relevance of the high oxygen extraction ratio, an emphasis on metabolic autoregulation whilst including any other mechanisms of physiological regulation.
Most candidates provided reasonable detail surrounding the arterial-circulation and the area of the heart these vessels supply. Less well described were the perforating branches, the capillary network and the venous drainage, these components were often incorrectly described or left out of the candidate answers. Most candidates correctly identified the phasic flow and the difference in flow that occurs between the right and left ventricle. Those candidates that used diagrams to explain this were rewarded when these diagrams were labelled and accurate with respect to their systolic and diastolic distinction. The control of regulation was less well answered with generic statements not specifically identifying the local metabolic controls importance over any other mechanism. Those answers that scored well coupled the metabolic control to the flow dependence highlighting the high oxygen extraction within the coronary circulation.
2021A 19: 62% of candidates passed this question.
Good candidates described normal blood flow to the coronary circulation, including differences between the right and left ventricles. Coronary artery anatomy was outlined, including the regions of the heart supplied and the concept of dominance. In addition to epicardial vessels, strong answers also outlined penetrating arteries, subendocardial supply and venous drainage. Regulation of coronary blood flow required an explanation of flow-dependence of the heart given its high oxygen extraction rate. Metabolic autoregulation and its mediators needed to be described, along with the physical factors driving coronary blood flow. Less important mechanisms such as the role of the autonomic nervous system were also described, with an emphasis on indirect effects over direct effects.
2018A 11: 46% of candidates passed this question.
Some answers suffered from listing things rather than describing things as the question required.
Better answers included a description of metabolic, physical and neuro-humoral factors and the relative importance of each.
Many described detailed anatomy which was not necessary.
2014B 10: 65% of candidates passed this question.
This question was generally well answered. Some candidates did not mention the factors which are peculiar to the coronary circulation and answered in a generic manner, as if for any vascular bed. The coronary circulation has a high O2-ER and flow-dependence. Many candidates seemed to lack a perspective that metabolic demand dominates control of the coronary arterial flow. The phasic nature of flow was best shown with a diagram and whilst “publication-level” graphs are not expected, the graph drawn must be factually correct and convey the principal similarities and differences. While this topic is covered in both Guyton and Ganong, additional detail can be found in the Mosby physiology monograph series: Cardiovascular Physiology, 10th Edition by Pappano and Wier,( the replacement of Berne and Levy).
2008B 11: 2 (40%) candidates passed this question
This question required the candidate to provide some detail why a given dose of intravenous anaesthetic administered for the purpose of induction may result in a variable response between individuals. A logical division into pharmacokinetic and pharmacodynamic factors pertaining to the drug and how these are impacted by patient physiology, citing appropriate examples, was expected. Extremes of age, pregnancy, low and high cardiac output states, sympathetic tone, body habitus and factors impacting on drug redistribution and elimination should have been addressed. Extra marks were awarded for relevant discussion of pharmacogenetics. Discussion of the “bolus effect” versus slow infusion of an induction drug, relative to these factors should have been included. Mention of drug interactions, idiosyncratic reactions and relevant pathophysiology impairing organ function reserve was appropriate. The consequences of variability in drug response in terms of over- / underdosing, haemodynamic compromise, respiratory depression, delayed recovery and allergic reactions needed emphasis to demonstrate understanding of the significance of predisposing factors.
Effective answers to this question utilised either clear headings, or a tabular format, dividing what is a large topic into discrete areas. The lack of a structured approach to this question was invariably unsuccessful.
Syllabus Ref: G2a 2.c,d,e,f,g
Suggested Reading: Pharmacology and Physiology in Anaesthetic Practice / R K Stoelting – 4th ed – 2006. Chapters 4,6.
iii. Describe the structure and functional significance of the excitatory, conductive, and contractile elements of the heart.
iv. Describe the normal pressure and flow patterns of the cardiac cycle.
v. Describe the foetal circulation.
2015A 02
Describe the Foetal Circulation and the changes that occur at birth
CICMWrecks Answer
Foetal Circulation
- Placenta
- Supplied by paired umbilical artery and drains to single umbilical vein
- Capillary networks in parallel à high flow, low resistance system, decreases overall systemic vascular resistance.
- Oxygenated blood (SpO2 80% PO2 35mmHg) from placenta returns to foetus via umbilical vein
- 60% of blood from umbilical vein bypasses liver via ductus venosus into IVC
- Blood in IVC from systemic circulation is hypoxaemic (SpO2 30%)
- Heart
- Blood from IVC enters right atrium and oxygenated blood, directed via the Eustachian valve, preferentially flows across foramen ovale to left ventricle à supplies ascending aorta (SpO2 65%, PaO2 25mmHg)
- This allows most oxygenated blood to supply the brain and coronary arteries
- Blood from SVC enters right atrium and continues to right ventricle and pulmonary arteries → flows into aorta via ductus arteriosus and predominantly supplies descending aorta (SpO2 60%, PaO2 20mmHg) and organs
- Blood from IVC enters right atrium and oxygenated blood, directed via the Eustachian valve, preferentially flows across foramen ovale to left ventricle à supplies ascending aorta (SpO2 65%, PaO2 25mmHg)
- Lungs
- High pulmonary vascular resistance due to;
- Unexpanded lungs
- Hypoxic pulmonary vasoconstriction
- Therefore blood in pulmonary artery preferentially perfuses systemic circulation via ductus arteriosus
- Only approx 12% of pulmonary arterial blood enters the pulmonary circulation
- High pulmonary vascular resistance due to;
Changes at birth
- Placenta
- Vasoconstriction occurs due to longitudinal stretch of umbelical vessels and increase in PaO2
- Augemented by clamping of vessels
- Loss of placenta increases systemic vascular resistance
- Increased left heart pressures
- Lungs
- After first breath…
- Hypoxic pulmonary vasoconstriction is relieved,
- Lung expands
- Recruitment of collapsed parallel capillary networks
- Dilation of existing vasculature
- Pulmonary blood flow increases 10-fold and pulmonary vascular resistance decreases
- Combined with decreased venous return (from placenta), decreases right heart pressures
- After first breath…
- Heart
- Foramen ovale
- Equilibration of right and left heart pressures closes flap of foramen ovale (occurs within minutes to hours)
- Pulmonary arterial blood flow further increases
- Ductus arteriosus
- The ductus arteriosus shunt become bi-directional
- Closure
- Due vasospasm caused by increased PO2
- Also, loss of PGE2 produced by placenta causes loss of vasodilation
- Occurs within 96 hours
- Foramen ovale
Sakurai 2016
Examiner Comments
2015A 02: 55 % of candidates passed this question.
This topic is well covered in standard texts and has been asked previously. Better answers displayed knowledge of the key concepts, such as the parallel circulations in the foetus and preferential flow of better oxygenated blood to the brain and upper limbs. Some candidates spent time on the maternal and placental circulations which were not required to answer the question asked.

Recent Comments