Syllabus (Fourth Edition, 2023)
Topics
i. Describe the principles of pulse and tissue oximetry, co-oximetry including calibration, sources of errors and limitations.
ii. Describe the principles of capnography, including calibration, sources of errors limitations.
iii. Describe the methods of measurement of oxygen and carbon dioxide tension in blood.
iv. Describe the principles of measuring oxygen concentration.
Topics not covered in previous SAQs
iv. Describe the principles of measuring oxygen concentration.
Learning Objectives for the First Part Examination in Intensive Care Medicine
- This will ensure that trainees, tutors, and examiners can work from a common base.
- All examination questions are based around this Syllabus.
- These learning objectives are designed to outline the minimum level of understanding required for each topic.
- The accompanying texts are recommended on the basis that the material contained within them provides sufficient information for trainees to meet the learning objectives.
- Trainees are strongly encouraged to explore the existing and evolving body of knowledge of the Basic Sciences as they apply to Intensive Care Medicine by reading widely.
- For all sections of the syllabus an understanding of normal physiology and physiology at extremes of age, obesity, pregnancy (including foetal) and disease (particularly critical illness) is expected.
- Similarly, for pharmacology, trainees are expected to understand a drug’s pharmacology in these contexts.
- An understanding of potential toxicity and relevant antidotes is also expected.
Definitions
Throughout the document specific wording has been used under the required abilities to indicate the level of knowledge and understanding expected and a glossary of these terms is provided.
Definitions
| Calculate | Work out or estimate using mathematical principles. |
| Classify | Divide into categories; organise, arrange. |
| Compare and contrast | Examine similarities and differences. |
| Define | Give the precise meaning. |
| Describe | Give a detailed account of. |
| Explain | Make plain. |
| Interpret | Explain the meaning or significance. |
| Outline | Provide a summary of the important points. |
| Relate | Show a connection between. |
| Understand | Appreciate the details of; comprehend. |
SAQs
i. Describe the principles of pulse and tissue oximetry, co-oximetry including calibration, sources of errors and limitations.
2021A 17
Describe the principles of measurement of arterial haemoglobin O2 saturation using a pulse oximeter (60% marks). Outline the limitations of this technique (40% marks).
2014A 07
Outline the principles underlying pulse oximetry. ( 80% of marks)
Briefly describe the effect of an elevated level of the following upon pulse oximetry values. (20% of marks) a. Carboxyhaemoglobin b. Methaemoglobin
2013B 05
Describe the principles of measurement of arterial haemoglobin O2 saturation using a pulse oximeter. (60% of marks) Outline the limitations of this technique. (40% of marks)
2008A 03
Describe the principles of measurement of arterial haemoglobin oxygen saturation using a pulse oximeter. Outline the limitations of this technique.
CICMWrecks Answer
Principles
Beer-Lambert Law
- Incidence of light is inversely proportional to the path distance and concentration of light absorbing particles within the path.
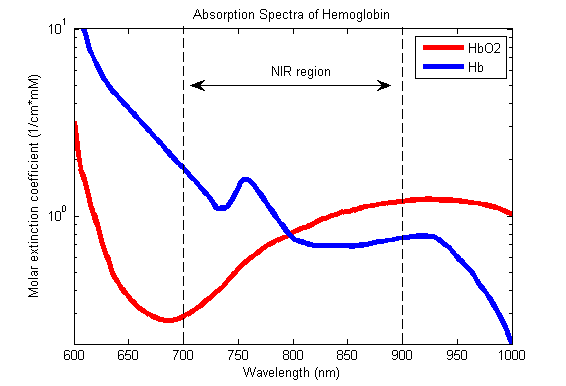
Hb absorbance at 660nm and 940nm utilized
- 660nm maximally absorbed by deoxyhaemoglobin
- Ratio of absorbance at 660nm and 940nm utilized to calculate SpO2
using healthy volunteers derived R values
Sats 100% R = 0.4
Sats 85% R = 1.0
Sats 50% R = 2
Sats 0% R = 3.4
Pulse oximeter
- Light emitter
- Produces infra-red light at 660nm and 950nm
- Light detector
- Detects light at 660nm and 950nm
- Processor
- Calculates SpO2 using the ratio of absorbance at 660nm and 950nm
- Light detected (incidence) represents light passing through both pulsatile (arterial) blood and non-pulsatile elements (venous blood and other tissues)
- Processor differentiates light incidence during maxima and minima of pulse wave and calculates SpO2 from pulsatile blood only giving SaO2
Limitations
| PATIENT FACTORS | ||
| Low or High SpO2 | Low SpO2 | Normal or High SpO2 |
| Met-Hb Sulph-Hb | Poor perfusion of finger Movement artifact Venous pulsations Fingernail polish Intravenous pigmented dyes Haemoglobinopathy Anaemia with co-existing hypoxia | Carbon Monoxide poisoning |
| EQUIPMENT FACTORS | ||
| – Ambient light interference – Poorly fitting probe – Assay calibrated using healthy volunteers only down to SpO2 80%. Unknown significance if tested SpO2 less than 80% | ||
| PHYSIOLOGICAL FACTORS | ||
| – Due to O2 dissociation curve, insensitive to changes above PaO2 80mmHg – Does not measure tissue oxygenation | ||
Absorption spectra confounded by:
- Carboxyhaemoglobin
- Absorbs 660nm, not at 940nm
- R closer to 0.4
- causes the pulse oximeter to read artificially high
- Methemoglobin
- though it absorbs 660nm light, it also absorbs 940nm light to a greater degree
- R closer to 1
- causes the SpO2 to trend towards 85%
Sakurai 2016
Examiner Comments
2021A 17: 74% of candidates passed this question.
Most candidates provided a reasonable structured sequence of how a pulse oximeter generates a value. Nearly all candidates described the Beer-Lambert laws correctly, but few specifically described the basic principles of absorption spectrophotometry. Most candidates had a reasonable list of extrinsic factors that can interfere with pulse oximeter performance, but few described the intrinsic/inherent limitations of the device that can cause SpO2 to be different to SaO2, such as functional versus fractional saturation.
2014A 07: 34% of candidates passed this question.
Explanation of several crucial principles was expected for a good answer. These would include that Haemoglobin can be measured and quantified with a light absorbance technique; based on the Beer Lambert law (a description of this was required). In addition, oxygenated haemoglobin must be distinguished from reduced haemoglobin (the 2 dominant species of Hb) and that the oximeter determines pulsatile from non pulsatile blood. The oximeter accounts for ambient light and that “R”, a ratio of absorbances during pulsatile and non pulsatile flow is calculated and compared within a computer algorithm to standardised values of SaO2 to deliver a final value.
Mention of limitations was not required except to answer the second part of question. Common omissions included failure to describe accurately the Beer Lambert Law, and no explanation of how pulsatile component was detected, or ambient light accounted for. Many candidates understood the clinical inaccuracy associated with CO and Met HB, but failed to identify the spectrophotometric reason and application of the R value for this discrepancy.
2013B 05: 18 candidates passed (66.7%).
A lack of understanding of the physics behind pulse oximetry was a common area of weakness amongst most candidates. Candidates were expected to mention the underlying principle of the “Beer Lambert” Law, absorption spectra and that the differential absorption of light at different wavelengths by different haemoglobin species is used to determine the fractions of haemoglobin types. Limitations should include mention of errors due to calibration as well as sources of false positive and false negative
readings.
2008A 03: No candidates (0%) passed this question.
The main points expected for a pass included a brief description of the following:
• The system components
• The principles of light absorbance and the Beer-Lambert Law
• The differential absorbance of Hb species in red/infrared spectrum, and their use to calculate the amount of reduced and oxygenated Hb present
• LED emitting 660/940/off cycles at 450-900Hz, averages data over several cycles to eliminate ambient light, and detect pulsatile and non pulsatile elements
• Pulse added absorption of each cycle compared as ratio “R” at different wavelengths
• Calibration curve to compare “R” to SaO2 data from healthy volunteers
• The limitations of the technique including:
– quality of product, bias, precision and accuracy
– insensitivity to PaO2
– false readings and their causes
Diagrams gained marks only with sufficient labelling and explanation.
Syllabus S2f
2021B 13
Describe the factors that affect mixed venous oxygen saturation.
2017A 19
Define mixed venous PO2 (20% of marks).
Outline the factors that affect this value (80% of marks).
2008A 10
Briefly describe the factors that influence the partial pressure of Oxygen in mixed venous blood.
CICMWrecks Answer
Mixed Venous Blood
- Mixed Venous Blood = blood taken from the pulmonary artery
- Normal mixed venous partial pressure of oxygen = 40mmHg -> 75% saturation
- Majority of oxygen in blood bound to haemoglobin
- Hb has 4 haem molecules, each can bind one oxygen molecule
- Affinity of Hb for oxygen changes with oxygen saturation, due to conformational change in the haem group on oxygen binding
- Affinity for oxygen decreased by: low pH, high CO2, high temperature, 1-3-DPG
Factors
- Complex interplay of factors which affect Venous Oxygen Partial pressure of oxygen and hence content
- Modified Fick principle: Mixed venous oxygen content = oxygen delivery – oxygen extraction
Oxygen Content
- = 20ml/100ml in arterial blood, 15ml/100ml in venous blood
- Vast majority of oxygen carried by haemoglobin, tiny dissolved portion
- Non-linear relationship between dissolved O2 and O2 content
- PO2 is the fraction of dissolved O2
- PO2 determines Sats based on Oxygen-Haemoglobin Dissociation Curve
Oxygen Delivery
= Cardiac output x Arterial oxygen content
Oxygen Demand
= Cardiac output x Arteriovenous O2 content difference
Oxygen flux
Hence SvO2 and pvO2 are surrogate markers for Oxygen flux
- O2 Delivery
- 1000ml/min in health
- Decrease in cardiac output: ↓HR, ↓SV (↓preload, ↓contractility, ↑afterload)
- Decrease in functional Hb: anaemia, carbon monoxide, congenital abnormalities of haemoglobin
- Decrease in oxygen saturation: V/Q mismatch, anatomical shunt, hypoventilation, low FiO2 (e.g. at altitude), right-shift of oxygen dissociation curve (low pH etc. – see above)
- Oxygen extraction:
- 250ml/min
- Increased by:
- increased tissue metabolism (e.g. sepsis, pregnancy, malignancy, post-operative catabolic state etc.)
- right shift of oxygen dissociation curve (see above)
Mooney / JC 2020
Examiner Comments
2021B 13: 49% of candidates passed this question
Mixed venous oxygen saturation is used as a surrogate marker for the overall balance between oxygen delivery and oxygen consumption. A good answer stated this, described the importance of where it is measured and went on to describe the various factors that affect oxygen delivery and consumption.
Descriptions of the factors that affect oxygen saturation of haemoglobin, partial pressure of oxygen in the blood and position of oxygen-haemoglobin dissociation curve were necessary to score well. Important omissions were factors that increased and decreased oxygen consumption. While many candidates were able to correctly write the equations for oxygen content and oxygen flux, they then failed to describe how the variables within these equations were related to mixed venous oxygen saturation.
2017A 19: 37% of candidates passed this question.
This question was in two parts – the first part was worth 20% and candidates were expected to provide a definition of mixed venous blood as well as the partial pressure of oxygen in mixed venous blood (including normal range). Good answers also provided the varying PO2 from different tissue beds that make up mixed venous blood, where the ‘mixing’ occurs (the right ventricle) and where it is sampled (pulmonary artery).
For the second part of the question, worth 80% of the marks, good answers included the relationship between mixed venous PO2 and mixed venous O2 content (including the shape and position of the HbO2 dissociation curve); the variables encompassed in the modified Fick equation; arterial oxygen content and its determinants; oxygen consumption (VO2); and cardiac output (CO). Including an outline of how each affects the value of mixed venous PO2. A number of candidates wrote about mixed venous oxygen saturation. Other common errors were: missing a number of key factors that affect PO2; and using an incorrect form and/or content of the modified Fick equation.
2008A 10: 1 candidate (33%) passed this question.
The main points candidates were expected to cover included:
- A discussion of the non-linear relationship between O2 content and partial pressure and the factors which affect this relationship. No candidate included this.
- Modification of the Fick equation as it relates mixed-venous oxygen to delivery and consumption.
- The components of delivery should have been described and use of the O2 flux equation would have been helpful. Additional marks were available for describing how these might change in physiological and pathological states.
Candidates frequently interchanged content and partial pressure, without clearly displaying how these are related. Normal values were not provided. The O2 flux equation, when included, was often written incorrectly. No consideration was given to normal variations, such as pregnancy or exercise
Reference: Nunn 5th edition pages 267 to 269, page 493
Syllabus: B1h Gas transport in the blood 2a
2019A 08
Compare and contrast the measurement (40% of marks) and interpretation (60% of marks) of both central venous and mixed venous oxygen saturations.
CICMWrecks Answer
Physiology
Oxygen Delivery
= Cardiac output x Arterial oxygen content
Oxygen Demand
= Cardiac output x Arteriovenous O2 content difference
Oxygen flux
Hence SvO2 is a surrogate marker for Oxygen flux
| Decrease in ScvO 2 or SvO 2 | Increase in ScvO 2 or SvO 2 |
|---|---|
| O2 consumption ↑ Stress, Pain Hyperthermia Shivering | O2 delivery ↑ CaO2 ↑ Cardiac output ↑ |
| O2 delivery ↑ CaO2 ↓ (anemia, hypoxia) Cardiac output ↓ | O2 consumption ↓ Analgesia, Sedation Mechanical ventilation Hypothermia |
Measurement: Co-oximetry
Co-oximetry:
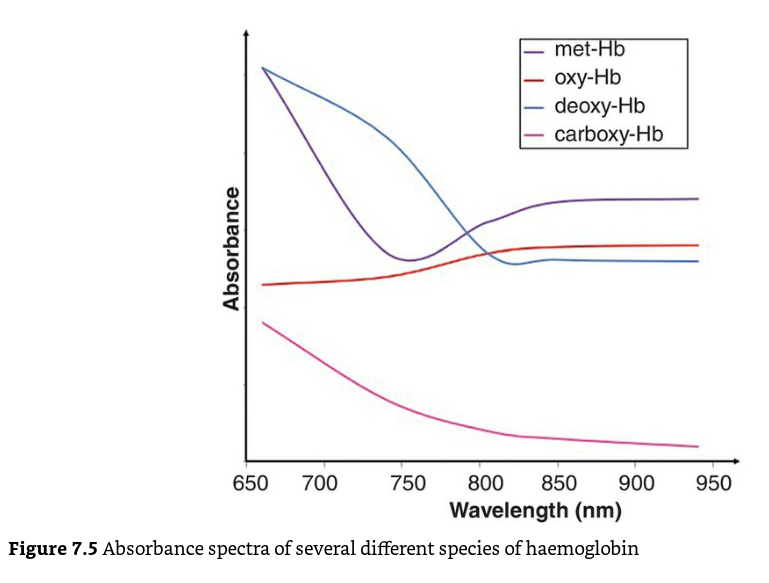
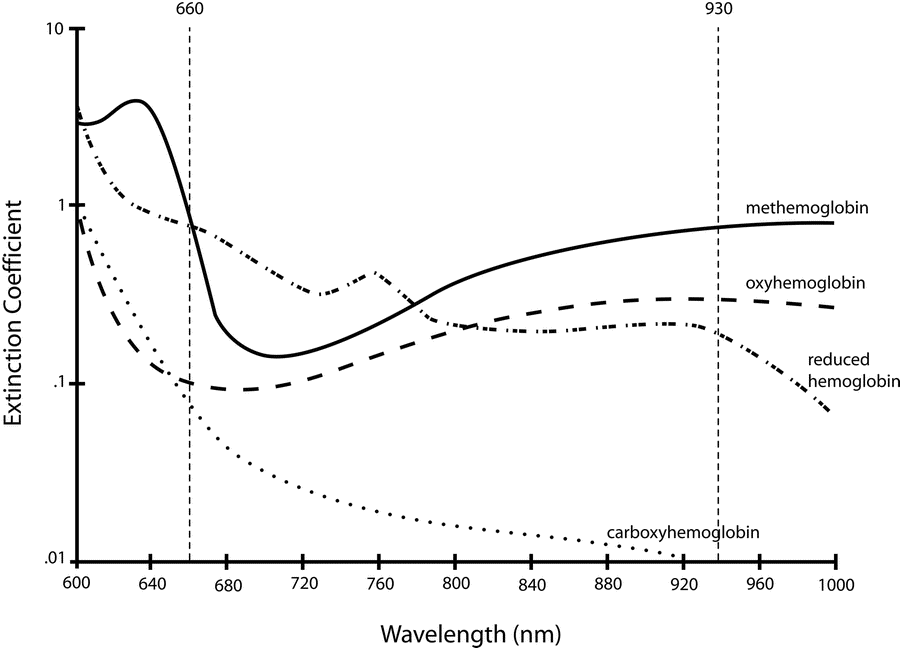
- A co-oximeter is a blood gas analyzer that, in addition to the status of gas tensions provided by traditional blood gas measurements, measures concentrations of oxygenated hemoglobin (oxyHb), deoxygenated hemoglobin (deoxyHb or reduced Hb), carboxyhemoglobin (COHb), and methemoglobin (MetHb) as a percentage of the total hemoglobin concentration in the blood sample
- Different haemoglobin species have different absorption spectra.
Mechanism / Measurement
- Uses Beer-Lambert law to detect different Hb species.
- “Incidence of light is inversely proportional to the path distance and concentration of light absorbing particles within the path”
- multi-wavelength spectrophotometry (measures the absorption of light passing through blood from several dozens of wavelengths)
- Complex, but straightforward internal computations
- enables the instrument to distinguish between oxy-Hb, deoxy-Hb, and carboxyhemoglobin,-COHb, methemoglobin -metHb, other hemoglobin moieties and ‘background’ light-absorbing species
- This is reported as the fractional oxyhaemoglobin content (FO2Hb), which is defined below
- The FO2Hb measure provides a more accurate picture of the availability of oxygen to the tissues in the presence of haemoglobin variants.
- If the original blood sample contained no carboxy-Hb or met-Hb, then the values for FO2Hb and SaO2 would be identical.
Mixed venous vs Central venous O2 Sats
| Mixed Venous Oxygen Sats SvO2 or SmvO2 | Central Venous oxygen sats ScvO2 | |
|---|---|---|
| Measure of Oxygen flux [matching between delivery (DO2), and consumption (VO2)] | Surrogate for SvO2 | |
| Blood drawn from | Proximal Pulmonary Artery More invasive Intermittent only | SVC Less Invasive Can be continuous or intermittent |
| Clinical picture | Average venous oxygenation Balance between systemic delivery and consumption | Venous oxygen saturations of blood from upper body |
| Physiology | SvO2 > ScvO2 as it contains blood from both SVC and IVC Normally 65-70% <65% – impaired tissue oxygenation >80% – hyperoxic or cytotoxic states, shunting | ScvO2 < SvO2 as it contains predominantly SVC blood (which has lower sats than IVC) Normally ~65% <50% tissue hypoxia >75% high flow states |
| Advantages | Systemic picture | No PA catheter required Easily performed in ICU through CVC |
| Disadvantages | Arrhythmias Catheter knotting Perforation of PA Infection | Unreliable correlation with systemic oxygenation in advance sepsis/septic shock Complications of CVC |
| Situations where this value is higher than the other | Normal states | a) Anaesthesia – because of increase in CBF & depression of metabolism b) Patients with head injury where cerebral metab is depressed c) Shock: because of diversion of blood from splanchnic circulation, there is increased O2 extraction and therefore IVC saturation decreases. |
| Other Data Generated | Qt, PA pressures, derived indices and body temperature measurements | CVP |
| Evidence | Study by Gattinoni – only RCT as far as SvO2 is concerned showed no benefit from SVO2 monitoring Study by Jones – showed trending lactate clearance was non-inferior | Study by Rivers- early goal directed therapy improved outcome in septic shock. Newer studies – ProMISE, ProCESS, ARISE have shown no benefit (or harm) from EGDT. |
Sources/Further Reading:
Bloos, F., Reinhart, K. Venous oximetry. Intensive Care Med 31, 911–913 (2005). https://doi.org/10.1007/s00134-005-2670-9
CICM Examiner’s Report Fellowship Paper 2 2006
JC 2020
Examiner Comments
2019A 08: 8% of candidates passed this question.
Many candidates did not appreciate that ScvO2 refers to SVC / RA junction venous oximetry and not femoral or peripheral venous oximetry. Methods of measurement such as co-oximetry and reflectance spectrophotometry needed to be explained. Marks were awarded for the normal values. Discussion of the relationship between ScvO2 and SmvO2 and changes during shock attracted marks. Better answers quoted the modified Fick equation and related this to cardiac output and factors affecting oxygen consumption versus delivery.
2018A 08
Outline the principle of co-oximetry (40% of marks), describe what a co-oximeter is able to measure (30% of marks), and compare its limitations to those of a pulse oximeter (30% of marks).
CICMWrecks Answer
Pulse oximeters assumes that only oxy-Hb and deoxy-Hb are present in the blood. It cannot differentiate other species of haemoglobin such as carboxyhaemoglobin (carboxy-Hb) or methaemoglobin (met-Hb) because it only uses two wavelengths of light (660 nm and 940 nm).
Co-oximeter:
- A co-oximeter is a blood gas analyzer that, in addition to the status of gas tensions provided by traditional blood gas measurements, measures concentrations of oxygenated hemoglobin (oxyHb), deoxygenated hemoglobin (deoxyHb or reduced Hb), carboxyhemoglobin (COHb), and methemoglobin (MetHb) as a percentage of the total hemoglobin concentration in the blood sample
- Use of co-oximetry is indicated:
- when a history is consistent with toxin exposure
- hypoxia fails to improve with the administration of oxygen
- there is a discrepancy between the Pao2 on a blood gas determination and the oxygen saturation on pulse oximetry (Spo2)
- clinician suspects other dyshemoglobinemias such as methemoglobinemia or carboxyhemoglobinemia.
- Different haemoglobin species have different absorption spectra.
Mechanism / Measurement
- Uses Beer-Lambert law to detect different Hb species.
- “Incidence of light is inversely proportional to the path distance and concentration of light absorbing particles within the path”
- multi-wavelength spectrophotometry (measures the absorption of light passing through blood from several dozens of wavelengths)
- Complex, but straightforward internal computations
- enables the instrument to distinguish between oxy-Hb, deoxy-Hb, and carboxyhemoglobin,-COHb, methemoglobin -metHb, other hemoglobin moieties and ‘background’ light-absorbing species
- This is reported as the fractional oxyhaemoglobin content (FO2Hb), which is defined as:
- The FO2Hb measure provides a more accurate picture of the availability of oxygen to the tissues in the presence of haemoglobin variants.
- If the original blood sample contained no carboxy-Hb or met-Hb, then the values for FO2Hb and SaO2 would be identical.
Advantages:
- Accurate measure of oxygen saturation: low readings indicate true hypoxia, and high readings always represent true hypoxia
- Able to detect different Hb species, like deoxy-Hb, carboxy-Hb, met-Hb
- Not confused by ambient light, absence of pulsatile flow, tricuspid regurgitation, methylene blue dye.
Limitations of co-oximetry:
- Expensive (depending on device
- Invasive (Blood sample needed)
- Variations with different devices, especially due to Limitations on Quality control
- Possible false values with severe hypoxemia, and extremes of Hb concentrations (better with newer generation devices)
- Not available in all blood gas analyzers
- Continuous monitoring not commercially availabe yet
Limitations of pulse oximetry:
| PATIENT FACTORS | ||
| Low or High SpO2 | Low SpO2 | Normal or High SpO2 |
| Met-Hb Sulph-Hb | Poor perfusion of finger Movement artifact Venous pulsations Fingernail polish Intravenous pigmented dyes Haemoglobinopathy Anaemia with co-existing hypoxia | Carbon Monoxide poisoning |
| EQUIPMENT FACTORS | ||
| – Ambient light interference – Poorly fitting probe – Assay calibrated using healthy volunteers only down to SpO2 80%. Unknown significance if tested SpO2 less than 80% | ||
| PHYSIOLOGICAL FACTORS | ||
| – Due to O2 dissociation curve, insensitive to changes above PaO2 80mmHg – Does not measure tissue oxygenation | ||
JC 2020
Examiner Comments
2018A 08: 32% of candidates passed this question.
Most candidates confused co-oximetry with other methods of measuring oxygenation of blood. Whilst there were a number of excellent descriptions of pulse oximetry, these attracted no marks for the first two sections. Structuring the answer based on the three parts asked, would have improved answers ensuring all aspects of the question were addressed.
2023B 01
Explain why the oxygen-haemoglobin saturation value derived by a pulse oximeter (SpO2) could be different from the measured arterial value (SaO2).
CICMWrecks Answer
Methods of Measuring oxygen saturation
Co-oximetry
- Blood gas analyzers measure arterial SaO2 by co-oximetry. (gold standard of SaO2 measurement)
- measures concentrations of oxygenated hemoglobin (oxyHb), deoxygenated hemoglobin (deoxyHb or reduced Hb), carboxyhemoglobin (COHb), and methemoglobin (MetHb) as a percentage of the total hemoglobin concentration in the blood sample
- Accurate measure of oxygen saturation: low readings indicate true hypoxia, and high readings always represent true hypoxia
- Not confused by ambient light, absence of pulsatile flow, tricuspid regurgitation, methylene blue dye.
- Uses Beer-Lambert law to detect different Hb species.
- “Incidence of light is inversely proportional to the path distance and concentration of light absorbing particles within the path”
- multi-wavelength spectrophotometry (measures the absorption of light passing through blood from several dozens of wavelengths)
Pulse oximetry
- Light emitter
- Produces infra-red light at 660nm and 950nm
- Light detector
- Detects light at 660nm and 950nm
- Processor
- Calculates SpO2 using the ratio of absorbance at 660nm and 950nm
- Light detected (incidence) represents light passing through both pulsatile (arterial) blood and non-pulsatile elements (venous blood and other tissues)
- Processor differentiates light incidence during maxima and minima of pulse wave and calculates SpO2 from pulsatile blood only giving SaO2
SpO2 different from SaO2
| PATIENT FACTORS | ||
| Low or High SpO2 | Low SpO2 | Normal or High SpO2 |
| Met-Hb Sulph-Hb | Poor perfusion of finger Movement artifact Venous pulsations Fingernail polish Intravenous pigmented dyes Haemoglobinopathy Anaemia with co-existing hypoxia | Carbon Monoxide poisoning |
| EQUIPMENT FACTORS | ||
| – Ambient light interference – Poorly fitting probe – Assay calibrated using healthy volunteers only down to SpO2 80%. Unknown significance if tested SpO2 less than 80% | ||
| PHYSIOLOGICAL FACTORS | ||
| – Due to O2 dissociation curve, insensitive to changes above PaO2 80mmHg – Does not measure tissue oxygenation | ||
Examiner Comments
2023B 01: 32% of candidates passed this question.
This question required candidates to identify that the measured arterial value (SaO2) was the gold standard to which the limitations of the pulse oximeter should be compared. A detailed description of the intrinsic and extrinsic factors of potential sources of difference of the SpO2 measurement was then expected. Intrinsic factors included wavelengths used, pulse added absorbance, derivation of the SpO2 value and time delays. Extrinsic factors where largely patient and environment related including light pollution, poor peripheral perfusion for various reasons, probe location variances and probe artefact.
ii. Describe the principles of capnography, including calibration, sources of errors limitations.
2022A 19
Describe the physiological factors that affect PaCO2.
CICMWrecks Answer
PaCO2: measure of carbon dioxide within arterial or venous blood
PCO2
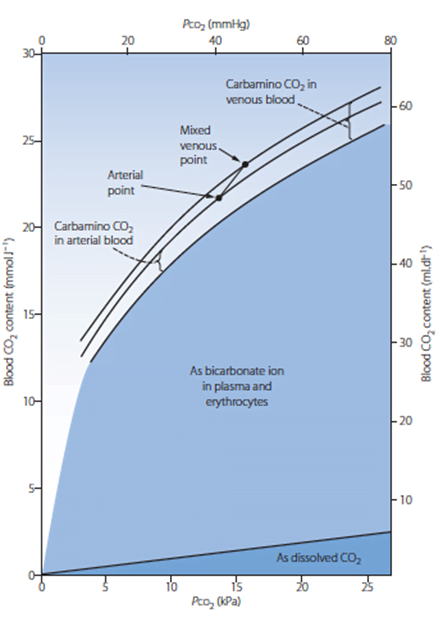
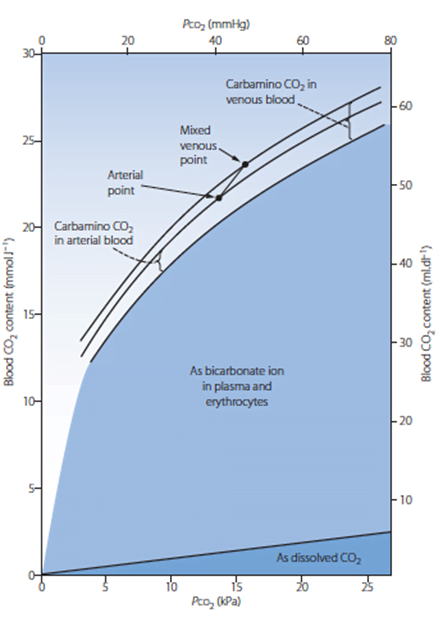
- Small portion of CO2 carriage in blood – approx. 5%
- The rest being HCO3 (approx. 90%), Carbamino compounds (approx. 5%), and carbonic acid (negligable)
- Constitutes 10% of A-V difference in CO2 carriage
- The rest being HCO3 (approx. 60%) and Carbamino compounds (approx. 30%)
- Obeys Henry’s Law
- Mass of dissolved gas is proportional to its partial pressure
- Solubility coefficient of CO2 ~0.54
- Obeys Dalton’s Law
- Sum of all partial pressures equals the environmental atmospheric pressure
Factors affecting PaCO2
- Factors affecting PaCO2
- Rate of metabolism and CO2 production
- FiCO2 (usually negligible)
- Alveolar ventilation
- Increased alveolar ventilation decreased PaCO2
- PaCO2
- In ideal system equal to PACO2 – 10% shunt only increases CO2 by 0.7mmHg
- PACO2 = (CO2 delivery to lung) / (Alveolar ventilation)
- Alveolar ventilation = (Vt – Vd) x RR
- Vt = Tidal volume – Approx. 7ml/kg
- Vd = Dead space volume
- Anatomical deadspace = first 16 divisions of airway – approx 2ml/kg
- Alveolar deadspace – Volume of non-perfused lung
- Increases with
- West zone 1
- PE
- Decreased lung perfusion
- Decreased cardiac output
- Positive pressure ventilation
- Upright posture
- Increases with
- RR – Regulated by medullary respiratory centre
- Chemoreceptor
- Peripheral
- Sensitive to decreased pO2, decreased pH, decreased blood flow and increased pCO2
- Increases respiratory rate
- Central
- Sensitive to CO2 via conversion to [H+]
- Increases respiratory rate
- Peripheral
- Baroreceptor
- Decreased stretch of aortic and carotid baroreceptors increases respiratory rate
- Pulmonary receptors
- J fibres
- Stimulation causes apnoea, bronchoconstriction, bradycardia and hypotention
- Stretch receptors
- Inflation reflex – Inhibits inspiration on lung inflation
- Deflation reflex – Inhibits expiration on lung deflation
- J fibres
- Chemoreceptor
- CO2 production and metabolism
- production occurs predominantly in mitochondria
- From metabolism of glucose
- Glucose + 6O2 → 6CO2 + 6H2O
- From
- BMR – 40kcal/hr/m2
- Increased muscle activity
- Post-prandial metabolism
- Thyroid hormones increase metabolism
- Catecholamines increase metabolism
- Disease states
- Fever
- Malignant hyperthermia
- Tourniquet
- Relative perfusion of tissues
- Blood from highly metabolic tissues contributes relatively greater amounts of CO2 per weight
- Blood from less metabolic tissues contributes relatively less CO2 per weight
- From metabolism of glucose
- production occurs predominantly in mitochondria
Sakurai 2016
Examiner Comments
2022A 19: 33% of candidates passed this question.
Candidates who scored well generally defined PaCO2 and proceeded to describe factors in terms of those related to production and elimination. Good answers described the key production factor as being rate of production through aerobic metabolism which is in turn influenced by substrate and BMR. Those who scored well described elimination as being dependent upon minute ventilation, which in turn is influenced by CO2 detection by chemoreceptors, specifically detailing the difference between peripheral and central. Many candidates detailed pathophysiological factors which unfortunately did not gain any marks.
2018B 03 – 2017A 21 – 2009A 09 – 2007B 24
Explain the causes of the differences between measured end tidal and arterial partial pressures of carbon dioxide (CO2).
CICMWrecks Answer
PaCO2
- Factors affecting PaCO2
- Rate of metabolism and CO2 production
- FiCO2 (usually negligable)
- Alveolar ventilation
- Increased alveolar ventilation decreased PaCO2
End-Tidal CO2
- CO2 contained in gas at the end of tidal expiration
- Contains:
- Alveolar CO2
- High CO2 diffusion – PACO2 = PaCO2
- Only 0.7mmHg Alveolar-arterial CO2 gradient for 10% shunt
- Alveolar Dead Space CO2
- Anatomical – conducting airways
- Physiological – West zone 1 / Apex
- Varies with posture and pathology
- Alveolar CO2
- Measured by capnometer
- In-line or side-stream
- Used IR absorbance at 4.23 μm
- Side-stream: lag in CO2 detection due to increased dead space between respiratory tract and analyzer
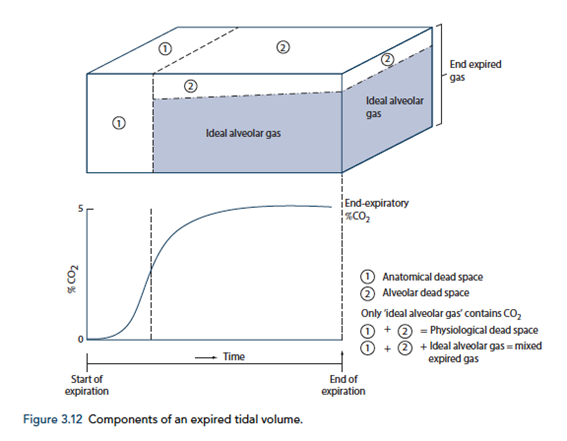
End-tidal to Arterial PaCO2 difference
- Normal ETCO2 – PaCO2 ~5mmHg
- Can be due to Artificially low ETCO2 or Artificially High PaCO2
Artificially low ETCO2
- Dead space (VD)
- Assumed PCO2 however usually low pCO2 but non 0 pCO2
- Contributes to ETCO2-PaCO2 ~5mmHg
- Pathological ↑VD
- ↑alveolar dead space (normal individuals = 0)
- Mixing of gas between perfused and non-perfused alveoli → ETCO2 < PaCO2
- Equivalent to ↑ West Zone 1
- → PE, hypotension, excess PEEP/IPPV
- COAD – poor perfusion of hyper-expanded alveoli
- ↑alveolar dead space (normal individuals = 0)
- Closing capacity (CC):
- Usually
40 CC may exceed FRC - ↑ Airways collapse/gas trapping → airways closure → ↑alveolar pCO2 within alveoli not exhaling
- Exacerbated by
- low volume ventilation close to FRC
- High FiO2 for extended periods → denitrogenation → loss of airways splinting = CC closer to FRC
- Usually
- Sampling line problems:
- Too far from trachea (ie ↑ mechanical dead space)
- Too long – unable to adequately sample as gas is trapped in line
- Air leakage/line blockage leading to measurement error with entraining of room air, loss of expired air
- Machine:
- Loss of calibration of sampling unit
- Excess H2O in water trap interfering with measurement
- Interference from other gases (N2O) artificially raises ETCO2 due to interference with IR absorber “Collision broadening”
- Incorrect timing of measurement
- Inadequate expiration time → failing to reach plateau = incomplete alveolar expiration = falsely low ETCO2
Artificially high PaCO2
- Should be measured from arterial sample
- Venous sampling will artificially ↑pCO2
- Loss of calibration of machine
Gladwin / Sakurai 2016
Examiner Comments
2018B 03: 29% of candidates passed this question.
The answer required an explanation of the causes of the difference between the PaCO2 and ETCO2. This required recognising how the end point of phase 3 of the capnograph trace corresponds with end tidal CO2. The difference is caused by the alveolar dead space. The difference is normally very small in healthy adults with the ETCO2 being lower than the PaCO2. It is increased with increasing alveolar dead space. Many incorrectly attributed anatomical dead space as a contributor to the PaCO2-ETCO2 gradient. Discussion of the various types of dead space did not score marks. Marks were awarded for the processes that cause an increased gradient e.g. low cardiac output and pulmonary embolism. Recognising physiological factors such as increasing gradient with increasing age scored marks. Marks were not awarded for descriptions on how dead space is measured.
2017A 21: 30% of candidates passed this question.
Many candidates didn’t distinguish between the different types of dead space. In general this topic was not well understood.
2009A 09: Pass rate: 40%
Good answers were in tabular format.
The antidepressant action is similar for each agent. Initial increase in 5HT and NA, followed in 2-3 weeks by a down regulation or change in efficiency of 5HT transmission. The agents produce elevated neurotransmitters via different mechanisms, either reuptake blockade or enzyme inhibition. MAOIs can be competitive or non-competitive. Mention of the different neurotransmitters affected by each agent was required.
A description of significant side effects at therapeutic doses, and in overdose was expected with explanations provided. These should have included – the anticholinergic effects and cardiotoxicity of TCAs, postural hypotension, the catecholamine, pethidine and tyramine related complications of MAOIs, and serotonin syndrome with SSRI/MAOI use and or overdose. More marks were gained for mention that side effect profiles can be beneficial e.g. analgesic properties of TCAs, sedation with TCAs/ SSRIs and energizing benefits of SSRIs/SNRIs. SSRI’s safety and efficacy have markedly reduced the use of MAOIs and to a lesser extent TCA’s..
Syllabus G2f2d
Reference: Stoelting p 398-407, Katzung p 476-487.
2007B 24: 0 candidates passed this question.
The main points for a pass were
Patient factors:
- Normal value for the difference between end tidal and arterial CO2
- Physiological factors e.g. alveolar dead space, failure to plateau of the capnograph trace
- Pathological factors e.g. cardiac arrest, air embolism, asthma
Equipment factors: Leaks, Occlusion, Samling site errors etc
A common mistake was to state that dead space caused the difference between end tidal and arterial carbon dioxide but not which type of dead space. The Bohr equation was not required.
2015B 23
Describe the factors that affect the partial pressure of CO2 in mixed venous blood.
2011A 07
Briefly describe the factors that affect the partial pressure of carbon dioxide in mixed venous blood.
CICMWrecks Answer
Mixed venous blood
- Mixture of all venous blood from all tissue capillary beds.
- Sampled from pulmonary artery
- In reality, omits venous blood from physiological shunt
PCO2
- Small portion of CO2 carriage in blood – approx. 5%
- The rest being HCO3 (approx. 90%), Carbamino compounds (approx. 5%), and carbonic acid (negligable)
- Constitutes 10% of A-V difference in CO2 carriage
- The rest being HCO3 (approx. 60%) and Carbamino compounds (approx. 30%)
- Obeys Henry’s Law
- Mass of dissolved gas is proportional to its partial pressure
- Solubility coefficient of CO2 ~0.54
- Obeys Dalton’s Law
- Sum of all partial pressures equals the environmental atmospheric pressure
PMVCO2
- Sum of PaCO2 and dissolved portion of CO2 produced
- PaCO2
- In ideal system equal to PACO2 – 10% shunt only increases CO2 by 0.7mmHg
- PACO2 = (CO2 delivery to lung)/(Alveolar ventilation)
- Alveolar ventilation = (Vt – Vd) x RR
- Vt = Tidal volume – Approx. 7ml/kg
- Vd = Dead space volume
- Anatomical deadspace = first 16 divisions of airway – approx 2ml/kg
- Alveolar deadspace – Volume of non-perfused lung
- Increases with
- West zone 1
- PE
- Decreased lung perfusion
- Decreased cardiac output
- Positive pressure ventilation
- Upright posture
- Increases with
- RR – Regulated by medullary respiratory centre
- Chemoreceptor
- Peripheral
- Sensitive to decreased pO2, decreased pH, decreased blood flow and increased pCO2
- Increases respiratory rate
- Central
- Sensitive to CO2 via conversion to [H+]
- Increases respiratory rate
- Peripheral
- Baroreceptor
- Decreased stretch of aortic and carotid baroreceptors increases respiratory rate
- Pulmonary receptors
- J fibres
- Stimulation causes apnoea, bronchoconstriction, bradycardia and hypotention
- Stretch receptors
- Inflation reflex – Inhibits inspiration on lung inflation
- Deflation reflex – Inhibits expiration on lung deflation
- J fibres
- Chemoreceptor
- CO2 production
- Occurs predominantly in mitochondria
- From metabolism of glucose
- Glucose + 6O2 → 6CO2 + 6H2O
- From
- BMR – 40kcal/hr/m2
- Increased muscle activity
- Post-prandial metabolism
- Thyroid hormones increase metabolism
- Catecholamines increase metabolism
- Disease states
- Fever
- Malignant hyperthermia
- Tourniquet
- Relative perfusion of tissues
- Blood from highly metabolic tissues contributes relatively greater amounts of CO2 per weight
- Blood from less metabolic tissues contributes relatively less CO2 per weight
- From metabolism of glucose
- Occurs predominantly in mitochondria
Sakurai 2016
Examiner Comments
2015B 23: 15 % of candidates passed this question
It was expected candidates would define key concepts, particularly ‘mixed venous’. Many candidates knew some of the elements that contributed to mixed venous PCO2 but few described all of the main factors. There was little mention of tissue capillary flow as a factor affecting mixed venous CO2
2011A 07: 1 (8%) of candidates passed this question.
Candidates were expected to provide a definition of important terms such as mixed venous. Many candidates provided much information about the partial pressure of carbon dioxide in arterial blood without discussing the factors which alter the mixed venous pressure.
Partial pressure of CO2 in mixed venous blood depends on the CO2 content of the mixed venous blood, which in turn represents a balance between CO2 production in the tissues and the CO2 content in arterial blood. Good answers demonstrated an understanding of this and provided relevant details about these aspects. The partial pressure of CO2 is related to the CO2 content by the CO2 dissociation curve, the position of which is determined by the state of oxygenation of haemoglobin, the Haldane effect. CO2 production is related to aerobic metabolism in cells and total production is defined by the metabolic rate. Examples of increased and decreased CO2 production gained additional marks. The partial pressure of CO2 in mixed venous blood is related to the partial pressure or content of CO2 in arterial blood.
This is determined mainly by alveolar ventilation under the control of chemoreceptorsand the brainstem respiratory centre.
Syllabus: B1h, 2c
Recommended sources: Applied Respiratory Physiology, Nunn 5th edition, Chp 10 pages 222 to 239
2023A 03
Outline the principles of measurement of end-tidal CO2 using infrared radiation (25% of Marks). Describe the potential sources of error when using this modality and how they may be mitigated (75% of Marks).
2019B 10
Describe the principles of capnography, including calibration, sources of error and limitations.
2015B 09
Describe the principles of measurement of end-tidal CO2, including the sources of error.
2010A 04
Describe the underlying principles involved in the measurement of end tidal CO2 (by infrared analysis), including sources of error and interference.
CICMWrecks Answer
Principles
- Beer Lambert law: At a given wavelength, the amount of infrared radiation absorbed by gas is proportional to the concentration of gas present
- CO2 is a heteronucleic molecule, and so absorbs infra-red light
- Infrared light shone across a sample of gas
- Narrow band light emitted from infrared source
- Band frequency chosen which fits the peak absorption frequency of CO2
- 4.23micrometres
- Shone across gas, and absorbed at a detector
- Detector emits signal to analyser -> screen
- CO2 reading outputted is inversely proportional to CO2 present in sample, as per Beer-Lambert Law
- Narrow band light emitted from infrared source
- Gas can be sampled at the patient within the ventilation circuit (in-line), or in a sample of gas diverted away to a separate analysing chamber (sidestream)
Sources of error and limitations
- Sampling
- Entrainment of atmospheric gas if leak in sidestream line
- Occlusion of sidestream line causes loss of gas sampling
- Water condensation absorbs IR light -> erroneously high ETCO2
- Modern capnography includes a water trap and heater (to reduce condensation)
- Calibration
- Incorrect calibration of analyser
- Interference
- Other gases (notably N2O) have a similar absorption spectrum
- Presence may falsely elevate measured ETCO2 (esp. if infrared frequency band too broad)
- Presence of other gases causes ‘collision broadening’
- Absorption spectrum of CO2 is broadened
- Pressure
- Partial pressure, rather than percentage composition, is measured
- If pressure ↓ (e.g. by suction drawing gas into sampling chamber), erroneously low measured ETCO2
- Sampling chamber
- If too large, mixing of gas between respiratory cycles -> compression of waveform and erroneously low measured ETCO2
Mooney 2016
Examiner Comments
2023A 03: 21% of candidates passed this question.
The principles of infrared (IR) measurement of expired CO2 was answered in acceptable detail by most candidates. Sources of error were rarely identified nor explained in acceptable detail. Many candidates demonstrated errors of understanding when attempting to answer this section. Important concepts not covered by numerous candidates included side-stream vs mainstream techniques; how the Beer-Lambert law is applied and how concentration is used for partial pressure; what is the role of sapphire glass and the difference between collision broadening and additional IR absorption by N2O.
2019B 10: 31% of candidates passed this question.
Answers that scored well followed the structure outlined in the question and explained the principles of each component of the question
2015B 09: 19% of candidates passed this question.
Candidates were expected to be detail the principles required to measure carbon dioxide in expired gas. This would involve some comment on ways to sample end tidal gas (in line vs side stream) and also ways to measure carbon dioxide. It was expected candidates could provide a detailed description of infrared analysis including the apparatus design and principles such as the asymmetric nature of CO2 as a polyatomic gas allowing absorption if infrared radiation with some discussion of response times and equipment design. It was expected these principles would be related to the potential errors (e.g. other gases, collision broadening)
2010A 04: 1 (10%) of candidates passed this question
Candidates were expected to at least mention and describe the following points – absorption at the infrared spectrum; Beer-Lambert Law and it’s relevance to measurement of ETCO2; sources of error (effect of other gases, atmospheric pressure), sources of interference (gas sampling methods, heating), calibration, features of the sampling chamber that may cause error (glass construction, size), sampling rates, etc.
Answers provided by candidates lacked breadth and depth, indicated that there was generally a poor understanding of this topic. The usual mistake was to discuss the clinical reasons behind the reading not reflecting the PaCO2 rather than sources of error of the end tidal CO2. Candidates should review this topic from the references from which the answer was sought and texts included as recommended reading.
Syllabus: R2d, S2g
iii. Describe the methods of measurement of oxygen and carbon dioxide tension in blood.
2022B 16 – 2014B 22
Describe how the values for PaO2, PaCO2, pH and bicarbonate are determined on a blood gas sample.
CICMWrecks Answer
Blood Gas: pO2
- Measured using Clark Electrode
- Platinum cathode
- Coated in gas permeable membrane à permeable to O2
- Membrane impermeable to other oxidizing molecules
- O2 + 4e– → 2O–
2O– + 2H2O → 4OH–
- Silver chloride anode
- 4Ag → 4Ag+ + 4e–
4Ag+ + 4Cl– → 4AgCl
- 4Ag → 4Ag+ + 4e–
- Phosphate buffer with KCl
- Platinum cathode
- Cathode voltage potential to -0.65v
- In absence of O2 current = 0v
- In presence of O2, O2 diffuses through gas-permeable membrane and is reduced, absorbing 4e–
- Micro-ampmeter measures movement of electrones between anode and cathode
- The current produced is proportional to the pO2 of the test solution
- Sensitivity – related to thickness of membrane and size of cathode area
Blood Gas: pCO2
- Measured using Stowe-Severinghaus Electrode
- Modified pH electrode with outer semi-permeable membrane (Teflon or Silicon Elastic)
- CO2 diffuses into electrolyte layer
- CO2 + H2O → H2CO3 → H+ + HCO3+
- H+ diffuses across glass electrode and alter pH
- Change in pH measured
- Henderson-Hasselbach Equation used to determine pCO2
Blood Gas: pH
- Measured using Sanz Electrode
- 2 half-cells connected by KCl bridge
- Measurement half-cell contain glass membrane with layers of hydrated and non-hydrated glass, permeable or sensitive to H+
- Measurement electrode consists of Silver-Silver chloride bathed in phosphate buffer at known pH 6.84
- Reference half cell contains mercury-mercury chloride in KCl saturated solution
- Measuring electrode responds to the H+ in the sample and the difference between reference and measurement cells measured by a voltmeter or pH meter
- At 37 degrees – change in one pH unit alters voltage by 61.5mV
Blood Gas: Bicarbonate
- Calculated from pH and CO2 using Henderson-Hasselbach Equation
- Actual bicarbonate
- Aerobically drawn arterial sample
- Standard bicarbonate
- Bicarbonate level in an oxygenated plasma specimen at 37 degrees and a pCO2 of 40mmHg
Sakurai 2016
Examiner Comments
2022B 16: 36% of candidates passed this question.
This question about how PaO2, PaCO2, pH, and HCO3 are obtained was not well answered by most candidates. Arterial blood gasses are routinely performed in most ICU on a daily basis. This question relates to a Level 1 (L1) topic in the CICM First Part Syllabus. Most answers simply lacked enough information. Details of how the Clark, Severinghaus, and Sanz electrode’s function was expected. Many candidates confused the pH and PaCO2 electrodes and confused the Clark (Polarographic) electrode with a Fuel Cell. Some knowledge about the types of electrodes and chemical reactions (e.g. reduction of O2 at the Platinum cathode in the Clark electrode) occurring in these devices was expected.
2014B 22: 23 % of candidates passed this question
A correct description of the Clarke electrode, Severinghaus and the pH electrode was expected to attain a pass. Candidates who used correct depictions of these electrodes with annotated description attracted higher marks. Most candidates didn’t comment on the temperature correction and standardization to 37 degrees. There was partial understanding on the calculation of HCO3 by most candidates. In general the question was poorly answered considering the wide spread use of blood gas analysis.

Recent Comments