Syllabus (Fourth Edition, 2023)
Topics
i. Describe and explain the oxygen cascade.
ii. Describe the movement of carbon dioxide from the cell to the atmosphere.
iii. Explain perfusion-limited and diffusion-limited transfer of gases.
iv. Define diffusing capacity and its measurement.
v. Describe the role of endogenous nitric oxide in ventilation and perfusion.
Topics not covered in previous SAQs
ii. Describe the movement of carbon dioxide from the cell to the atmosphere.
iv. Define diffusing capacity and its measurement.
v. Describe the role of endogenous nitric oxide in ventilation and perfusion.
Learning Objectives for the First Part Examination in Intensive Care Medicine
- This will ensure that trainees, tutors, and examiners can work from a common base.
- All examination questions are based around this Syllabus.
- These learning objectives are designed to outline the minimum level of understanding required for each topic.
- The accompanying texts are recommended on the basis that the material contained within them provides sufficient information for trainees to meet the learning objectives.
- Trainees are strongly encouraged to explore the existing and evolving body of knowledge of the Basic Sciences as they apply to Intensive Care Medicine by reading widely.
- For all sections of the syllabus an understanding of normal physiology and physiology at extremes of age, obesity, pregnancy (including foetal) and disease (particularly critical illness) is expected.
- Similarly, for pharmacology, trainees are expected to understand a drug’s pharmacology in these contexts.
- An understanding of potential toxicity and relevant antidotes is also expected.
Definitions
Throughout the document specific wording has been used under the required abilities to indicate the level of knowledge and understanding expected and a glossary of these terms is provided.
Definitions
| Calculate | Work out or estimate using mathematical principles. |
| Classify | Divide into categories; organise, arrange. |
| Compare and contrast | Examine similarities and differences. |
| Define | Give the precise meaning. |
| Describe | Give a detailed account of. |
| Explain | Make plain. |
| Interpret | Explain the meaning or significance. |
| Outline | Provide a summary of the important points. |
| Relate | Show a connection between. |
| Understand | Appreciate the details of; comprehend. |
SAQs
i. Describe and explain the oxygen cascade.
2015A 17
Describe the oxygen cascade in a person breathing room air at sea level.
2013A 11
Describe the oxygen cascade, from the atmosphere to the mitochondrion, in a patient breathing room air.
CICMWrecks Answer
- Fraction of O2 in atmosphere = 0.21
- Oxygen cascade:
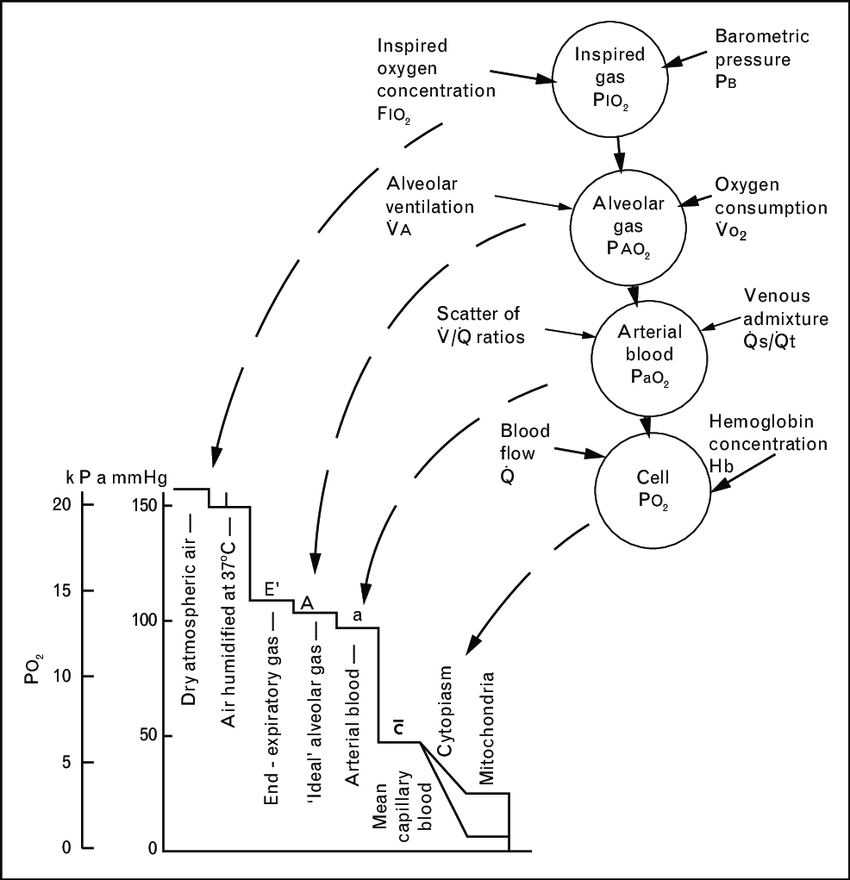
1. Oxygen in the atmosphere
- Oxygen in the atmosphere at sea-level
- Atmospheric pressure = 760mmHg
- pO2 = 760mmHg x 0.21 = 160mmHg
2. Oxygen in the bronchi
- Inspired air at sea level is humidified and saturated by H2O vapour at the isothermic saturation boundary 3cm distal to the carina
- pO2 = 0.21 (760mmHg – 47mmHg) = 150mmHg
3. Oxygen in the alveoli
- In the alveoli, inspired air is diluted with CO2 diffusing into the alveoli from the alveolar capillaries.
- pAO2 = 0.21(760mmHg – 47mmHg) – paCO2/R + f
- where, R = respiratory quotient, approx. 0.8
- f = correctional factor
- paCO2 = 40mmHg
- pAO2 = 100mmHg
- pAO2 = 0.21(760mmHg – 47mmHg) – paCO2/R + f
4. Oxygen in the arterial blood
- Oxygen diffuses from the alveoli to pulmonary capillaries (solubility coefficient 0.024) however paO2 is lower than pAO2 due to venous admixture
- Factors contributing to venous admixture
- V/Q mismatch
- Shunt
- The degree of venous admixture can be calculated by
- Oxygen in carried in blood as a predominant Hb bound portion and a minor diffused portion, governed by the oxyhaemoglobin dissociation curve
- In healthy adult, A-a gradient is no more than 15mmHg
5. Oxygen in the cytosol and mitochondria
- Oxygen diffuses from capillary blood across the plasma membrane (according to Fick’s law of diffusion) into the cell cytosol and then across the mitochondrial membranes into the mitochondria
- There is paucity of evidence to determine mitochondrial pO2 but estimated to be between 5mmHg and up to 40 mmHg in recent studies
Sakurai / Gladwin 2016
Examiner Comments
2015A 17: 63 % of candidates passed this question.
This question could be answered with a description or a diagram but required an ordered journey from the atmosphere to the mitochondria. This is commonly available in many texts and most candidates answered the question well. Most candidates said the alveolar PO2 fell solely because CO2 came out of the pulmonary capillary. Very few talked about oxygen uptake into the capillary. Another common omission was failure to state normal values for the A-a gradient.
2013A 11:
This topic is a core aspect of respiratory physiology. The vast majority of the candidates could draw the oxygen cascade, but were let down by not having sufficient breadth and/or depth of information (e.g. alveolar gas equation was either omitted, inaccurate or poorly described in relation to the oxygen cascade) to describe the physiological principals at each step of the cascade.
ii. Describe the movement of carbon dioxide from the cell to the atmosphere.
iii. Explain perfusion-limited and diffusion-limited transfer of gases.
2023B 06 – 2021A 15
Explain perfusion limited and diffusion limited transfer of gases in the alveolus.
2016B 22
Outline the physiological factors that affect the diffusion of oxygen and carbon dioxide within the lung.
CICMWrecks Answer
Fick’s law of diffusion
- Describes Diffusion through tissues
- Rate of movement of solute across semi-permiable membrane J is
where
C = concentration (or partial pressure for gasses)
A = cross-sectional area
T = thickness of the membrane or distance over which diffusion takes place.
The rate of diffusion of a gas through a tissue is:
Directly ∝:
- Surface area of the barrier
Affected by:- Parenchyma volume: Changes with Body size and in disease states
- V/Q mismatch: reduced in shunt and dead space
- Pulmonary Blood Volume: changed with vascular distension and recruitment
- Cardiac output: increased recruitment in high output states, decreased recruitment and increased V/Q mismatch in shock states
- Posture: Increased surface area while supine (compared to sitting or standing)
- Solubility of the gas
- CO2 is ~20 times as soluble as O2 in blood
- Concentration gradient (partial pressure difference)
- Rate of blood flow through lungs
- Transit time of blood across capillary (not part of Fick’s Equation) – based on HR
- alters total gas exchange across alveolus
- Can potentially change perfusion limited gas exchange to diffusion limited
- Alveolar partial pressure affected by:
- Atmospheric pressure
- Ventilation: Alveolar hypoventilation → ↑ PACO2 , ↓ PAO2
- Partial pressure in blood affected by:
- Binding of gas to protein:
- Rate of oxygenation of reduced Hb:
- Shift of oxygen dissociation curve (pH, temperature, PCO2, 2,3-DPG)
- Haematocrit
- Abnormalities of haemoglobin
- Formation of carbamino compounds
- Anaesthetic agents to plasma contents, e.g Albumin, cholesterol
- Enzymatic Action
- carbonic anhydrase (conversion of HCO3 to CO2)
- Rate of blood flow through lungs
Inversely ∝:
- Membrane thickness
- Increased thickness impedes gas exchange – Pathological states like pulmonary edema and cardiac failure
- Square root of Molecular Weight
- smaller substances diffuse more quickly
Diffusion vs. perfusion limited
Transfer of gases can be diffusion or perfusion limited dependent on the rate limiting step
Diffusion Limited
- Occurs in gases which do not reach equilibration of Pa and PA
- The rate of gas diffusion across the alveolar membrane limits its transport away from the lung
- Rate limiting step = rate of diffusion
- E.g. CO
- CO binds so avidly to Hb (250x that of O2) → virtually no CO dissolved in plasma → PaCO rises only slightly
- Even when RBC traversed entire length of pulmonary capillary, there is still substantial partial pressure difference across alveolar-capillary barrier → equilibrium of PaCO and PACO never reached
Perfusion Limited
- Characterized by complete equilibration i.e. Pa = PA
- amount of gas transferred between alveolus and capillary = dependent on amount of blood passing through the capillary
- rate limiting step = rate of blood flow
- E.g. N2O
- N2O rapidly diffuses across alveolar-capillary barrier
- Insoluble; does not bind to Hb; only carried in plasma in dissolved form
- PaN2O = PAN2O (<0.07sec); well before RBC has traversed pulmonary capillary
- ↑ diffusion rate will not ↑ blood transport away from the lungs → limiting factor = rate of blood flow / perfusion
- e.g. CO2 (ventilation limited i.e. perfusion limited in reverse)
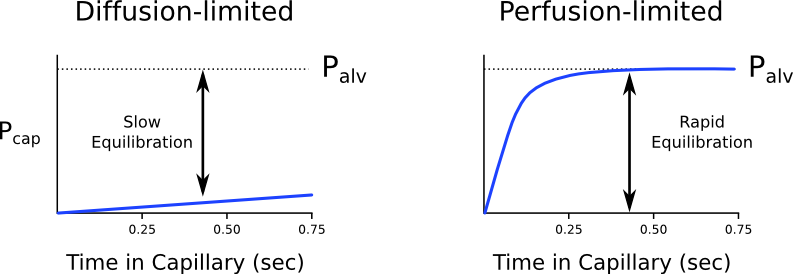
Is the transfer of O2 perfusion or diffusion limited?
- Can behave as both perfusion and diffusion limited
- O2 diffusion takes 0.25s; pulmonary capillary transit time is 0.75s
- Normal conditions
- Transfer of O2 across the alveolar capillary barrier is perfusion limited
- Equilibrium is reached between alveolar and capillary PO2 before the RBC has traversed the pulmonary capillary
- Conditions where transfer of O2 may become diffusion limited
- Disease of the alveolar capillary barrier
- Pulmonary fibrosis: thickening of alveolar-capillary barrier → ↓ rate of diffusion
- Exercise: ↑ CO → ↓ RBC transit time
- Altitude: ↓ PaO2
- Disease of the alveolar capillary barrier
Diffusion of O2 and CO2
Oxygen
- Oxygen diffusion takes ~0.25s
- Pulmonary capillary transit time is 0.75s
- Therefore, under normal conditions oxygen is a perfusion limited gas
- However, oxygen may become diffusion limited in certain circumstances:
- Alveolar-capillary barrier disease
Decreases the rate of diffusion.- Decreased surface area
- Increased thickness
- High cardiac output
Decreases pulmonary transit time. - Altitude
Decreases PAO2
- Alveolar-capillary barrier disease
Carbon Dioxide
- Carbon dioxide is ventilation limited, rather than diffusion or perfusion limited
- This is because it is:
- 20x more soluble in blood than oxygen
- Rapidly produced from bicarbonate and carbamino compounds
- Present in far greater amounts than oxygen
1.8L.kg-1 exist in the body (though 1.6L-1 of this are in bone and other relatively inaccessible compartments).
- Impairment of diffusion capacity causes type 1 respiratory failure as oxygen is affected to a much greater extent than carbon dioxide
Kerr / JC 2020
Examiner Comments
2023B 06: 48% of candidates passed this question.
This question required an explanation of the factors that influence perfusion and diffusion and a detailed description of the behaviour of specific gases including perfusion limited oxygen and carbon dioxide and diffusion limited carbon monoxide. Factors influencing perfusion include flow/cardiac output, resistance (radius and length) and viscosity whereas diffusion is influenced by the characteristics of the gas (MW and solubility), surface area of diffusing surface and the pressure/concentration gradient. Perfusion and/or diffusion limited characteristics of different gases included how quickly if at all equilibrium is reached and why this occurs with each specific gas.
2021A 15: 36% of candidates passed this question.
This question required detail on those factors affecting gas exchange at the level of the alveolus. A description of the components of the Fick equation was expected – and how this related to oxygen and carbon dioxide transfer at the alveolar capillary membrane. The rapid rate of equilibration (developed tension) was the limiting factor in of blood/alveolar exchange that rendered some gases perfusion limited (examples – N2O, O2 under usual conditions but not all) and the slower rate of others diffusion limited (examples CO and O2 under extreme conditions e.g., exercise, altitude). Estimates of time taken for each gas to equilibrate relative to the time taken for the RBC to travel across the interface was also expected for full marks. CO2 despite rapid equilibration and higher solubility was correctly described as perfusion limited (unless in disease states). Better answers described CO2 as ventilation limited. Some answers also correctly included the component of interaction with the RBC and haemoglobin. Ventilation/perfusion inequalities over the whole lung were not asked for and scored no marks.
2016B 22: 43% of candidates passed this question.
Good answers to this question were those that included a definition of diffusion; an outline of Fick’s Law of Diffusion and then a further description how each of the variables in the this Law affect the diffusion of oxygen and carbon dioxide in the lung; and an outline of the other factors that affect diffusion not covered by the above. Most candidates included Fick’s Law in their answers and at least briefly expanded on the associated variables.
Few candidates defined the process of diffusion. The other common omissions were the factors that affect diffusion that aren’t directly encompassed in Fick’s Law, such as cardiac output, capillary transit time, carbonic anhydrase (conversion of HCO3 to CO2) and combination of oxygen with haemoglobin.
iv. Define diffusing capacity and its measurement.
2012A 20
List the physiological factors affecting the diffusion of oxygen across the alveolar membrane (70% of marks).
Describe how this changes with exercise (30% of marks).
CICMWrecks Answer
- Diffusion capacity:
- “The volume of gas which will diffuse through a membrane each minute for a partial pressure difference of 1mmHg (ml/min/mmHg)”
- Normal diffusion capacity for oxygen (DLO2): 20ml/min/mmHg
- Fick equation:
- Thickness of membrane (normal: 0.3μm)
- Surface area of membrane (normal: 50-100m2)
- Age, posture, degree of inflation (1 mark for any)
- Partial pressure gradient across membrane
- Rate of blood flow through lungs
- (no points for mentioning diffusion constant of gas – question relates to only oxygen)
- Rate of oxygenation of reduced Hb
- Shift of oxygen dissociation curve (pH, temperature, PCO2, 2,3-DPG)
- Haematocrit
- Abnormalities of haemoglobin
In exercise
- DLO2 increases to 30-60ml/min/mmHg
- Increased VT and RR
- Increased alveolar ventilation → partial pressure gradient of O2 across capillary increases (significant as flow of erythrocytes through pulmonary vasculature likely to increase)
- Recruitment of dormant pulmonary capillaries (increased surface area for diffusion)
- due to: Increased lung inflation, Increased pulmonary arterial systolic pressure
- Perfusion increases from 21ml/min/mmHg up to 65ml/min/mmHg
- Better matching of ventilation-perfusion
Mooney 2016
Examiner Comments
2012A 20: 5 (50%) of candidates passed.
The first section of this question was generally well done, but few really good marks, whereas the second section was poorly understood. The diffusing capacity is defined as the volume of gas that will diffuse through the membrane each minute for a partial pressure difference of 1mmHg. Factors affecting the rate of gas diffusion through the respiratory membrane include those related to the Fick equation (e.g. thickness of the membrane, surface area of the membrane, diffusion coefficient of the gas in the substance of the membrane, partial pressure difference of the gas between the two sides of the membrane, gas’s solubility), rate of combination of oxygen with reduced haemoglobin and factors affecting surface area (e.g. lung volume, age, posture). During strenuous exercise the oxygen diffusion is increased as pulmonary blood flow is greatly increased and there is opening up of previously dormant pulmonary capillaries increasing the surface area of blood into which oxygen can diffuse. Also, alveolar ventilation increases and there is better matching of ventilation and perfusion increases from 21ml/min/mmHg up to 65ml/min/mmHg.

Recent Comments