Syllabus (Fourth Edition, 2023)
Topics
i. Describe the anatomical and physiological features of the pulmonary circulation.
ii. Understand pulmonary vascular resistance and the factors that affect this.
iii. Understand the differences between the pulmonary and systemic circulation.
Topics not covered in previous SAQs
.
Learning Objectives for the First Part Examination in Intensive Care Medicine
- This will ensure that trainees, tutors, and examiners can work from a common base.
- All examination questions are based around this Syllabus.
- These learning objectives are designed to outline the minimum level of understanding required for each topic.
- The accompanying texts are recommended on the basis that the material contained within them provides sufficient information for trainees to meet the learning objectives.
- Trainees are strongly encouraged to explore the existing and evolving body of knowledge of the Basic Sciences as they apply to Intensive Care Medicine by reading widely.
- For all sections of the syllabus an understanding of normal physiology and physiology at extremes of age, obesity, pregnancy (including foetal) and disease (particularly critical illness) is expected.
- Similarly, for pharmacology, trainees are expected to understand a drug’s pharmacology in these contexts.
- An understanding of potential toxicity and relevant antidotes is also expected.
Definitions
Throughout the document specific wording has been used under the required abilities to indicate the level of knowledge and understanding expected and a glossary of these terms is provided.
Definitions
| Calculate | Work out or estimate using mathematical principles. |
| Classify | Divide into categories; organise, arrange. |
| Compare and contrast | Examine similarities and differences. |
| Define | Give the precise meaning. |
| Describe | Give a detailed account of. |
| Explain | Make plain. |
| Interpret | Explain the meaning or significance. |
| Outline | Provide a summary of the important points. |
| Relate | Show a connection between. |
| Understand | Appreciate the details of; comprehend. |
SAQs
i. Describe the anatomical and physiological features of the pulmonary circulation.
2020B 13
Describe the anatomical (20% marks) and physiological (80% marks) features of the pulmonary circulation.
CICMWrecks Answer
Anatomy
- Thin walled arteries and veins, contains little smooth muscle → easily distorted by lung expansion
- Pulmonary arteries (deoxygenated blood) -> pulmonary capillaries (gas exchange) → pulmonary veins (oxygenated blood)
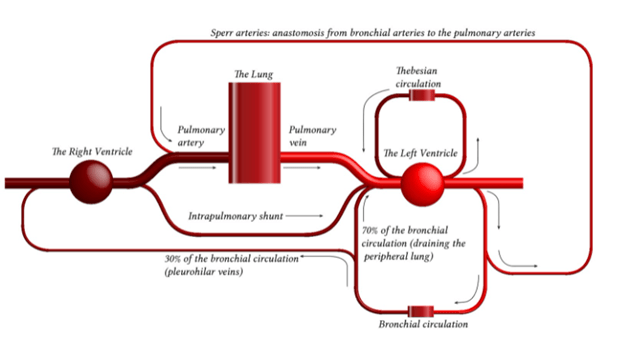
- Pulmonary capillaries are exposed to alveolar pressure and not supported by solid tissue → prone to collapse
- Contains 10% of circulating blood volume – 500mls
Physiology
- General:
- Low pressure 25/8 MPAP 15mmHg
- Low resistance 20-120 dynes.sec.cm-5
- Flow: total of cardiac output 5L/min
- Pulmonary blood volume
- ~500mls of blood – blood reservoir
- Varies over course of the respiratory and cardiac cycle and in response to gravity
- Varies in response to changes in intrathoracic pressure
- Pulmonary blood pressure
- Normal PA systolic pressure = 18-25 mmHg
- Normal PA diastolic pressure = 8-15 mmHg
- Normal mean pulmonary arterial pressure = 9-16 mmHg
- Capillary pressure is 8-10 mmHg
- Venous pressure 6-12 mmHg
- Resistance
- The resistance in the pulmonary circulation can be calculated as follows:
- PVR = 80 × (mPAP- PAOP)/CO
- The normal value for PVR is 100-200 dynes/sec/cm-5
- Approximately 1/10th of systemic circulation
- Regulation of blood flow/resistance
- West zones
- In zone 1, PA > Pa > Pv No flow of blood
- In zone 2, Pa > PA > Pv Resistance to flow is determined by alveolar pressure (Starling resistor effect)
- In zone 3, Pa > Pv > PA Resistance to flow is determined by venous pressure Venous pooling causes increased distension of pulmonary capillaries
- In zone 4 Low lung volume causes narrowing of extra-alveolar vessels
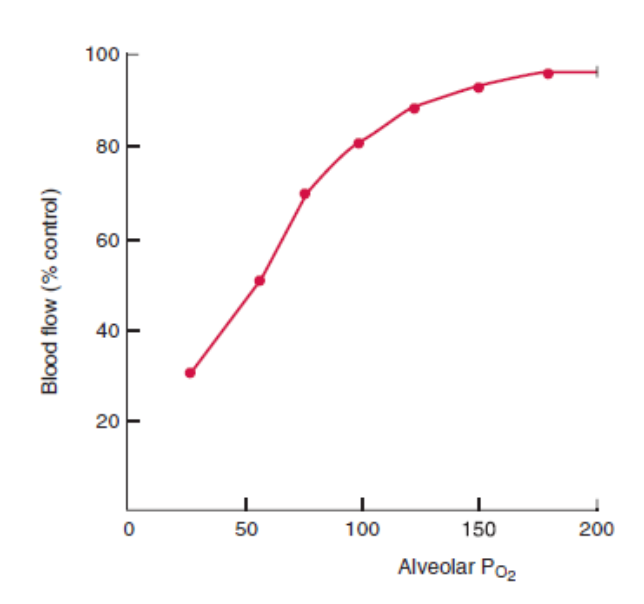
- Hypoxia – pulmonary hypoxic vasoconstriction
- Lung volumes
- West zones
- Regional distribution
- Distension of partially collapsed capillaries
- Recruitment of completely collapsed capillaries
- Local mediators: NO, prostacycline
- Function
- Gas exchange
- Filtration of clots and debris
- Immunological – pulmonary macrophages, IgA production
- Metabolic – metabolism of drugs, removal of proteases
- Endocrine – source of ACE
Guo 2021
Examiner Comments
2022B 15: 23% of candidates passed this question.
Many candidates described the anatomical pattern of right ventricle to arteries to smaller arteries to arterioles to capillaries to venules to veins to the left atrium. To obtain full credit one needed to describe relevant aspects of anatomy including main pulmonary artery ~5cm in length divides into L and R pulmonary arteries. Arteries are relatively thin walled with little smooth muscle, capillaries form an extensive sheet of blood flow over the alveolar wall, and the pulmonary circulation drains into four pulmonary veins that empty into the left atrium. A structured approach would then follow regarding physiology. There is ~500 ml of blood in the pulmonary circulation with ~10% in the capillaries and half the remainder in each of arteries and veins. The system has a high capacitance and is very distensible. The volume can halve or double to adjust for posture, respiratory effort and changes to the systemic circulation. Values for normal pulmonary artery pressure were expected and an explanation that this is just adequate to reach the apices of the lung and that if the pulmonary pressure was higher there would be a risk of compromised perfusion and flow. Comparisons with the systemic pressures or detail such as capillary values gained extra credit. For example, highlighting that regional distribution and regulation is relatively passive compared to the systemic circulation and thus gravity and posture have significant effects. Many candidates gave the units incorrectly. Of the candidates who described the West Zones, most seemed aware of the influence of alveolar pressure, but few seemed aware of the importance of low pulmonary pressure relative to the effect of gravity, such that the pulmonary arterial pressure was just adequate to reach the apex of the lung. Most candidates were aware of the important role of hypoxic pulmonary vasoconstriction to optimise VQ matching. The autonomic system has relatively little effect upon regulation especially compared to the systemic circulation. Many candidates wrote in generalities about the physiology of circulatory systems without discussing special features of the pulmonary circulation. The detail supplied was often less than the expected level.
2020B 13: 25% of candidates passed this question.
The examiners consider that an understanding of the pulmonary circulation is core area of the syllabus. In general, the anatomy section was better answered than the physiological features. As well as a description of the gross anatomy of the pulmonary circulation tracking it from the pulmonary valve to the left atrium, some mention of the microscopic anatomy was required (e.g., that the pulmonary arteries are thin walled with little smooth muscle).
For the second part of the question, a breadth of knowledge was required. Candidates were expected to address the following physiological features of the pulmonary circulation: volume, pressure, resistance, regulation and regional distribution and function. Marks were apportioned to each section, so it was important to write something on each section. Focussing on one section in detail (e.g., a very detailed description of West’s Zones) usually came at the expense of missing one or more of the other sections, most commonly the functions of the pulmonary circulation. Indeed, candidates that scored well provided information on each section and for the functions of the pulmonary circulation mentioned more than gas exchange.
2016B 19
Describe how Starling forces determine fluid flux within the pulmonary capillary bed.
CICMWrecks Answer
Introduction
- Capillaries contain semipermeable membranes to allow the movement of fluid and solutes.
- it is normally impermeable to large protein
- Plasma ultrafiltrate is filtered by bulk flow through the capillary wall by the action of opposing hydrostatic and oncotic pressures
- The key features of the pulmonary microcirculation are:
- The pulmonary capillaries (and the alveoli) have very thin walls which minimises the barrier to diffusion.
- In the alveolar walls, the capillaries form a dense network which has been considered to be almost a continuous thin film of blood. This provides a large capillary surface area.
- The pressures in the pulmonary circuit are much lower than in the systemic circulation and the pulmonary vascular resistance is very low. The pressure is just sufficient to perfuse the apical areas of the lungs in the erect healthy adult.
Starling Forces
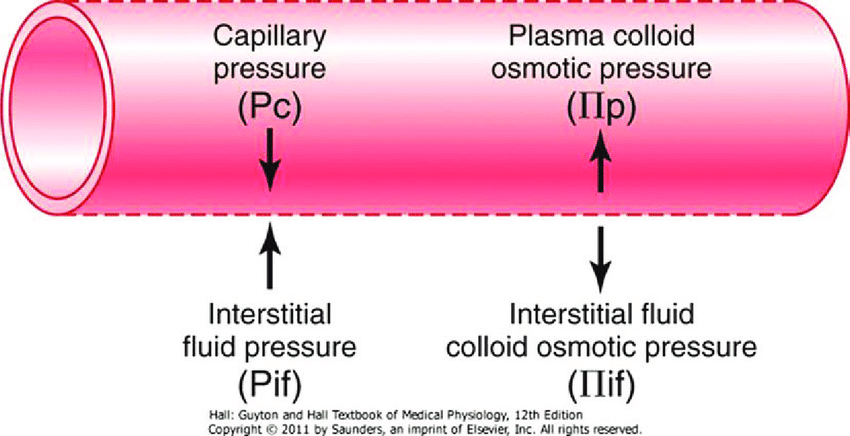
- The NET flux across the membrane is the balance of hydrostatic pressure and oncotic pressure, as defined by the Classic Starling Equation:
where
Jv is the trans endothelial solvent filtration volume per second
( [ Pc – Pi ] – σ [ πp – πi ] ) is the net driving force
P = hydrostatic pressure
π = oncotic pressure
σ = Staverman’s reflection coefficient ie. Permeability of membrane to protein (0.5 for lung)
κ = filtration constant = LpS = Hydraulic conductivity x Surface Area
| Pulmonary | Systemic | ||
|---|---|---|---|
| Pc Capillary hydrostatic pressure | Pressure moving fluid out of capillary | 13→6 mmHg Arterial → venous Variable due to hydrostatic effects of gravity in different parts of lung | ~35→15 mmHg Arterial → venous |
| Pi Interstitial hydrostatic pressure | Pressure moving fluid into capillary | Variable, but 0 to slightly negative | 5 mmHg |
| πp Plasma oncotic pressure | Pressure keeping fluid within capillary | 25 mmHg | ~20 mmHg |
| πi Interstitial fluid oncotic pressure | Pressure keeping fluid out of capillary | 17 mmHg | ~0 mmHg |
Oncotic pressure gradient
- The interstitial oncotic pressure is high indicating significant leak of protein (mostly albumin) across the thin capillary walls under normal circumstances. The reflection coefficient has been estimated at about 0.5
- Considering the typical values and allowing for the reflection coefficient, it can be estimated that the net oncotic gradient is small but favours reabsorption.
Hydrostatic pressure gradient
- The capillaries are called intra-alveolar vessels and the presssure they are exposed to is close to alveolar pressure (zero to slightly negative, due to surfactant) and become more negative closer to the hilum
- This favours flow of fluid from the alveolar intersitium into the pulmonary lymphatics.
- The capillary hydrostatic pressure is variable because of the effects of gravity.
- The pulmonary circuit has a low resistance and about half of this resistance is due to the pulmonary capillaries which have no muscle in their walls. The capillary hydrostatic pressure is quickly affected by changes in pulmonary artery pressure and left atrial pressure without much protective buffering.
Overall Effect
The balance of Starling forces in the lung is generally stated as favouring reabsorption because of the clinical fact that the lungs are generally dry and clearly need to be to facilitate gas exchange
Safety Factors Preventing Pulmonary Oedema
- Increased lymph flow
- Decrease in interstitial oncotic pressure (oncotic buffering mechanism)
- High interstitial compliance
JC 2019
Examiner Comments
2016B 19: 25% of candidates passed this question.
The equations for nett fluid flux and for nett filtration pressure were incorrect in many answers. Better answers presented the equations and discussed each of the elements as relevant to the pulmonary capillary bed, including difference from systemic capillary beds.
Mention of the role of lymphatics and of the effect of surfactant, left atrial pressure, gravity and posture gained marks, also.
2008B 24
Describe the gravity dependent processes which affect pulmonary blood flow (70% of marks).
Describe the changes that result from an acute increase in pressure in the pulmonary vessels (30%).
CICMWrecks Answer
Gravity Dependent Processes
- Low pressure circuit:
- pressure drop of ~10mmHg from RV (15mmHg) to LA (5mmHg)
- PAP is just sufficient to raise blood to top of lung
- Blood flow in upright lung varies due to gravity effect (hydrostatic Pressure)
- Lung divided into vertically into 4 zones (West Zones)
- Zone 1 not present in normal lungs
- manifests in Positive pressure ventilation, Hypovolaemia, eg. haemorrhage
- Zone 4 appears in the presence of interstitial pressures or at very low lung volumes
- Zone 1 not present in normal lungs
- Normal balance between the zones varies based on:
- changes in posture
- changes in airway pressures due to anatomical changes / disease, ventilation changes
- changes in lung volume:
- At extremes pulmonary capillaries are linearly stretched and collapse as may occur with hyperinflation.
- At very low lung volumes, extra-alveolar blood vessels become compressed and flow reduces (Zone 4).
- changes in pulmonary vascular pressures related to cardiac factors or pulmonary vascular disease
- There are alternate theories explaining the heterogeneity in pulmonary perfusion and ventilation in both health and disease, which suggest that gravity has a less important role in the variation of regional distribution
- for e.g: The underlying structure of the bronchial and pulmonary vascular anatomy with non-symmetrical branching (Structural theory)
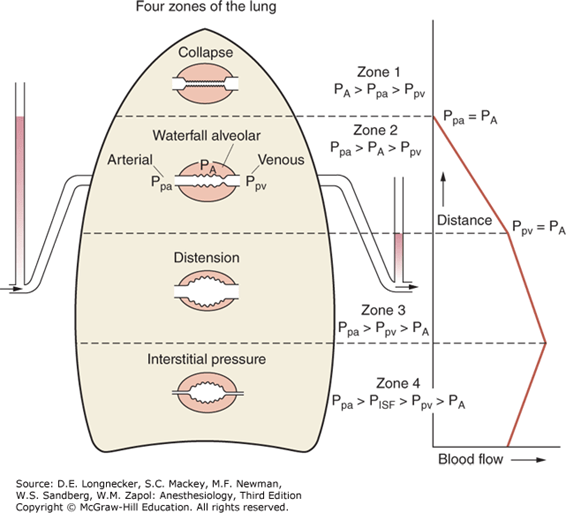
West Zone 1
- Not present in the normal lung
- Nil flow of blood to apical zones
- ↑alveolar dead space → High V/Q ratio
- Increased in:
- Hypotension, PE, Hyperinflation of lung with PPV
- Minimal change in PaO2 with increased West Zone 1 as Hb fully loaded
- Slight increase in PaCO2 as there is decreased apical perfusion, however this is compensated for by the increased RR chemoreceptor change: Minimal change in PaCO2
- Hypotension, PE, Hyperinflation of lung with PPV
West Zone 2
- Starling Resistor Mechanism
- ↑ hydrostatic P or ↓ Alveolar pressure → Pa > PA → capillary opens → flow → ↓ hydrostatic P ° to flow → Pa < PA → capillary closes
- Blood flow tends to ‘flutter’ (pulsatile flow)
- decreased in diastole, increased in systole.
- Increased in inspiration, decreased in expiration
- Present from the apex of the upright lung → 10cm above the level of the heart
West Zone 3
- Blood flow is constant due to the maintenance of arterio-venous pressure gradient
- Alveolar pressure is not a factor determining blood flow in this zone
- 10cm above the heart → bases of upright lung
- Effect of weight of lung ↓PA
- Hydrostatic pressure is maximal (~25mmHg)
- Low V/Q ratio
- Contributes to venous admixture
West Zone 4
- Interstitial pressure acts as a Starling resistor for pulmonary blood flow.
- It is seen when interstitial pressure is high (e.g due to pulmonary oedema).
- Also seen at very low lung volumes, where extra-alveolar blood vessels become compressed and flow reduces.
Effect of ↑P in pulmonary vessels
- Pulmonary circulation is low pressure circuit – ↑pressure 2° ↑PAP / PVP (LA) pressure
- Response in pulmonary vasculature is:
- Recruitment of closed capillaries
- Distension (↑caliber) of vessels
- Increased pressure delivered to the arterioles causes dilation and decreases resistance to flow, increasing flow by as much as twice what would be expected due to pressure alone
- Pulmonary arteries are approximately ½ as distensible as veins; this buffers pressure changes transmitted to the alveolar capillaries and also permits the arteries to adopt a reservoir function
- Net effect of recruitment and distension is bufering of pressure rise (↓pressure of pulmonary circulation) until these processess are exhausted or in the presence of pulmonary capillary disease
Gladwin 2016
Examiner Comments
2008B 24: 4 (80%) candidates passed this question
Most candidates quite correctly approached this from the perspective of “West’s zones of the lung. A clear description of the relationship between pulmonary arterial, venous and alveolar pressures producing the classical 3 zones was expected, along with situations which may alter the normal balance between the 3 zones, e.g. changing posture or airway pressure.
Additional points were awarded for candidates describing ‘zone 4’ or alternate theories of V/Q distribution. Whilst most candidates described recruitment and distension with respect to changing pulmonary arterial pressure, candidates were also expected to correctly state that an increase in pulmonary artery pressure is only observed when these processes are exhausted, or in the setting of pulmonary vascular disease, then describing the subsequent effects of pulmonary hypertension on the heart and circulation.
The vascular tree is distensible, that is, a change in pressure will produce a corresponding increase in dimension of the blood vessels:
Increased pressure delivered to the arterioles causes dilation and decreases resistance to flow, increasing flow by as much as twice what would be expected due to pressure alone The veins are 6 to 10 x as distensible as arteries owing to the structural differences in their respective walls. A notable exception is the pulmonary circulation where arteries are approximately ½ as distensible as veins; this buffers pressure changes transmitted to the alveolar capillaries and also permits the arteries to adopt a reservoir function. Pulmonary vascular resistance is also a function of lung volume. At extremes pulmonary capillaries are linearly stretched and collapse as may occur with hyperinflation. At very low lung volumes, extra-alveolar blood vessels become compressed and flow reduces (Zone 4). Use of appropriate graphs to illustrate some of the above points would have been desirable..
Syllabus Ref: B1i 2, B1k 2. a,c,i
Suggested Reading: Nunn’s Applied Respiratory Physiology / A B Lumb & J F Lunn – 6th ed – Chapters 7,8
ii. Understand pulmonary vascular resistance and the factors that affect this.
2009B 16
Discuss the factors affecting pulmonary vascular resistance.
CICMWrecks Answer
- Vascular resistance is the resistance to blood flow for a given pressure gradient across the vessels
- Pulmonary vasculature is a high capacitance, low pressure system
- Pulmonary artery pressures: 25/8 (MAP 15)
- Pulmonary Vascular Resistance (PVR)
- ~ 1/10th of SVR
- ~ 0.25-1.6 mmHg/L/min (or) 20-120 dynes.Sec.Cm-5
- Factors Affecting Pulmonary Vascular Resistance:
- Recruitment and Distension
- Gravity
- Autonomic Innervation
- Volume
- Hypoxia, Hypercapnoea, Acidosis
- Local Mediators
1. Recruitment and distension:
- At normal pressure and flows, most capillaries are either partially or completely collapsed
- At higher pressures, decrease in resistance due to
- Distension of partially collapsed capillaries
- Recruitment of completely collapsed capillaries
2. Gravity
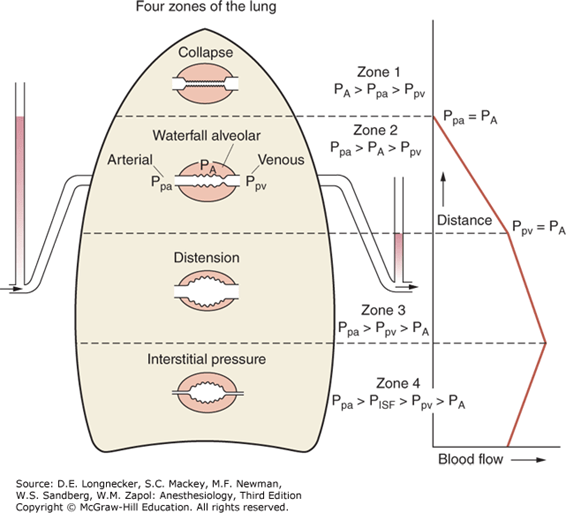
- Divided into West Zones based on relationship between Alveolar pressure (PA) Arterial pressure (Pa) Venous pressure (Pv) Interstitial pressure (Pi)
- West Zones 1,2,3: Due to changes in hydrostatic pressure when pumping to top of lung vs. bottom of lung
| West Zone | Pressure Relationships | Physiology | Location |
|---|---|---|---|
| Zone 1 | PA > Pa > Pv | No flow of blood, as arterial pressure completely opposed by alveolar pressure | not seen in normal lung |
| Zone 2 | Pa > PA > Pv | Resistance to flow is determined by alveolar pressure (Starling resistor effect) | about 3cm above the heart |
| Zone 3 | Pa > Pv > PA | Resistance to flow is determined by venous pressure Venous pooling causes increased distension of pulmonary capillaries | majority of healthy lung |
| Zone 4 | Pa > Pi > Pv > PA | Low lung volume causes narrowing of extra-alveolar vessels | Lung bases at low lung volume or in pulmonary edema |
3. Autonomic innervation:
- Sympathetic innervation from sympathetic trunk
- Noradrenaline
- α1 (vasoconstriction) and β (vasodilation) receptors
- α effects dominate (vasoconstricton)
- Parasympathetic innervation from vagus nerve
- Acetylcholine (M3 receptors)
- Cause vasodilation
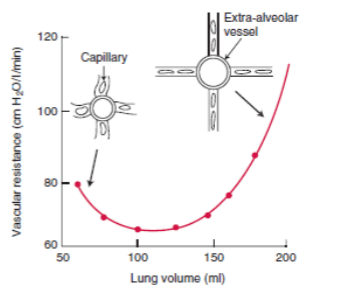
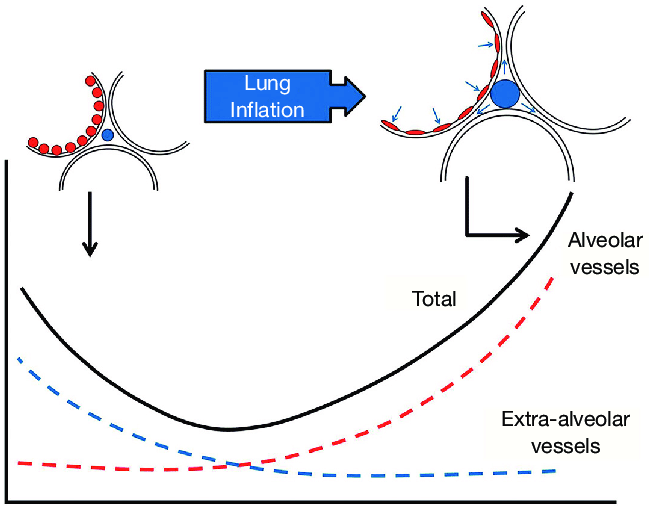
4. Volume
- Extra-alveolar vessels are stretched laterally by increased volumes
- Compressed by low volumes
- Pulmonary capillaries are stretched longitudinally by increased volumes, decreasing
radius -> more resistance - PVR is a balance of these two effects
- PVR is lowest at functional residual capacity
5. Hypoxia, Hypercapnoea, Acidosis
- Hypoxia:
- Alveolar (not arteriolar) hypoxia causes local vasoconstriction of pulmonary vessels
- This limits perfusion of underventilated lung regions, reducing shunt
- There is a similar, but less potent, effect of hypercapnoea and acidosis on vascular tone, reducing perfusion of hypoventilated regions
6. Local mediators:
- Dilators:
- Nitric oxide
- Prostacycline
- Isoprenaline
- Constrictors:
- Histamine
- Serotonin
- Endothelins
Mooney 2016
Examiner Comments
2009B 16: 3 (33%) of candidates passed this question.
A good answer to this question required a discussion that focused on the following key
points-
- Recruitment and distension of pulmonary capillaries. Helps limit pulmonary vascular resistance as pressure and flow increase.
- Lung volume. Lung inflation is thought to have a dual effect, expanding large vessels by traction while compressing smaller vessels and resistance is dependent upon lung volume, being lowest at approx FRC.
- Gravity. Perfusion is distributed down a vertical gradient in the lung, reflecting the balance between intra-alveolar pressure and the distending vascular pressure. (West’s Zones)
- Oxygen. Hypoxia causes pulmonary vasoconstriction. Diverts blood away from hypoxic regions of the lung.
- Hypercapnia and acidosis vasoconstriction
- Autonomic innervation. Alpha -adrenergic stimulation – vasoconstrictor, Beta-adrenergic stimulation – vasodilatation, Parasympathetic stimulation – Vasodilatation
- Local mediators. Vasoconstrictors (Serotonin, histamine, endothelins) and Vasodilators (NO, prostacyclin, isoprenaline)
The majority of these points could be efficiently explained through the use of graphs/figures,
all of which are commonly found in the majority of physiology books that include respiratory
physiology. Those candidates who failed to do so were also those who scored fewer points
with this question.
2016B 05
Describe the physiological factors that affect pulmonary arterial pressure (65% of marks).
Write short notes on the use of inhaled nitric oxide as a pulmonary vasodilator (35% of marks).
CICMWrecks Answer
Factors affecting Pulmonary Arterial Pressure
Pressure in a system is generated by the interaction between flow and resistance
Factors affecting Pulmonary artery pressure are: PBF x PVR
Factors affecting Pulmonary Vascular Resistance
- Recruitment and Distension
- At higher pressures, decrease in resistance due to distension of partially collapsed capillaries and recruitment of completely collapsed capillaries
- Gravity – West Zones
- Zone 1 – PA > Pa > Pv – no flow of blood
- Zone 2 – Pa > PA > Pv – Resistance determined by alveolar pressure (starling resistor effect)
- Zone 3 – Pa > Pv > PA – Resistance determined by venous pressure
- Zone 4 – Pa > Pi > Pv > PA – Low lung volumes causes narrowing of extra-alveolar pressures
- Autonomic Innervation
- Sympathetic innervation from sympathetic trunkNoradrenaline
- α1 (vasoconstriction) and β (vasodilation) receptors
- α effects dominate (vasoconstricton)
- Parasympathetic innervation from vagus nerve
- Acetylcholine (M3 receptors)
- Cause vasodilation
- Sympathetic innervation from sympathetic trunkNoradrenaline
- Volume
- Balance of extra vascular lateral stretch (↓resistance) by increasing volumes and capillary longitudinal stretch (↑ resistance)
- Hypoxia, Hypercapnoea, Acidosis
- Alveolar hypoxia causes local vasoconstriction
- Similar but less potent effect of hypercapnoea and acidosis
- Local Mediators
- Dilators: Nitric oxide, prostacycline, Isoprenaline
- Constrictors: Histamine, Serotonin, Endothelins
Factors affecting Pulmonary Blood Flow
- Venous return
- MSFP – RAP
- Resistance to venous return
- LV output, RV output
- Gravity dependant
- Recruitment and distension of vasculature
Inhaled Nitric Oxide
Click to open CICMWrecks Table: Nitric Oxide
JC 2019
Examiner Comments
2016B 05: 51% of candidates passed this question.
Pressure in a system is generated by the interaction between flow and resistance. A structured approach to defining and describing the many factors that influence fluid flow and resistance was required to score well. Poiseuille’s law describes the determinants of resistance to laminar fluid flow and provides a useful answer structure. It is also necessary to describe factors that determine flow. This includes factors that determine venous return, as well right and left heart output.
A standard structured answer to the pharmacology of nitric oxide enabled concise and high scoring answering of this question.
iii. Understand the differences between the pulmonary and systemic circulation.
2017A 07
Compare and contrast the systemic circulation with the pulmonary circulation.
CICMWrecks Answer
| Pulmonary circulation | Systemic circulation |
|---|---|
| Movement of blood from the heart to the lungs for oxygenation, then back to the heart again | Movement of blood from the heart through the body to provide oxygen and nutrients to the tissues of the body while bringing deoxygenated blood back to the heart |
| Deoxygenated blood (RA) → RV → Pulmonary Artery →→→ capillary beds → Oxygenated blood →→→ Pulmonary Veins → LA | Oxygenated blood (LA) → LV → Aorta →Major Arteries →→→ Capillaries → Gas and nutrient exchange → Deoxygenated blood →→→ Veins → Vena cavae → RA |
| Accept the entirety of cardiac output, with little capacity to regulate flow (hypoxic vasoconstriction being the exception) | Regulate flow to different organs at different times Contains resistance vessels which allow it to allocate cardiac output accordingly. |
| Low pressure – low resistance | High pressure – high resistance |
| BP – 25/8 (mean 15) mmHg | BP – 120/80 mmHg |
| Pressure differences from inlet to outlet of the pulmonary system is about (15 – 5) = 10 mmHg | Pressure differences from inlet to outlet of the systemic system is about (100 – 2) = 98 mm Hg which is ~ 10 times that in pulmonary system |
| the walls of the pulmonary artery and its branches are remarkably thin and contain relatively little smooth muscle (they are easily mistaken for veins). | the arteries generally have thick walls and the arterioles in particular have abundant smooth muscle. |
| The lung is required to accept the whole of the cardiac output at all times. It is rarely concerned with directing blood from one region to another | The systemic circulation regulates the supply of blood to various organs, including those which may be far above the level of the heart (the upstretched arm, for example). |
| At any given time, contains ~10% of the circulating blood volume, or about 500ml. | At any given time, contains ~90% of the circulating blood volume, or about 5400ml. |
| Blood Flow = Cardiac output (in the abscence of shunts / recirculation) | Blood Flow = Cardiac output (in the abscence of shunts / recirculation) |
| highly compliant – the volume of blood is able to change substantially with minimal change in pressure | Compliance varies depending on distance from heart and as per different regional circulations |
| The distribution of pressures along the pulmonary circulation is far more symmetrical. Much of the pressure drop occurs within the capillary bed itself | Most of the pressure drop is just upstream of the capillaries |
| The pulmonary capillaries are virtually surrounded by gas, and receive little support. Hence are liable to collapse or distend, depending on the pressures within them and alveolar pressure. | All capillaries are surrounded and supported by solid tissue |
| PVR ~ 1/10th of SVR ~ 0.25-1.6 mmHg/L/min 20-120 dynes.Sec.Cm-5 | SVR 9-20 mmHg/L/min 900-1200 dynes.sec.cm-5 |
| Minimal sympathetic effect (as relatively little smooth mm.) | SVR highly regulated by Autonomic tone |
| PVR decreases significantly as pulmonary artery pressure increases because of capillary recruitment (mainly) and distension | This inverse relationship not so significant |
| Both the arteries & veins increase their caliber as the lung expands by radial traction. | No such phenomenon in systemic circulation |
| Vasodilate in response to hypoxia and hypercapnoea | Vasoconstrict in response to hypoxia and hypercapnoea |
| gas exchange function: between blood to air | between blood and tissues |
| metabolic and synthetic functions: Metabolism of: 5HT, PGs ACE: convert AT I → AT II) Synthesize thromboplastin, Heparin | Delivers substance to organ systems for metabolism, synthesis, excretion Synthesizes NO Synthesizes pro- and anti- coagulants |
| role in acid base homeostasis: by CO2 exchange by buffering | by metabolism and excretion via kidneys, liver, skin, GI, etc by buffering |
| Filters large emboli | Filtration in Liver and Kidney |
| Some reservoir function in pulmonary vasculature | Large reservoir in organs (mainly Liver) and venous system |
JC 2019
Examiner Comments
2017A 07: 26% of candidates passed this question.
This question encompasses a wide area of cardiovascular physiology. As a compare and contrast question this question was well answered by candidates who used a table with relevant headings. Comprehensive answers included: anatomy, blood volume, blood flow, blood pressure, circulatory resistance, circulatory regulation, regional distribution of blood flow, response to hypoxia, gas exchange function, metabolic and synthetic functions, role in acid base homeostasis and filter and reservoir functions.
A frequent cause for missing marks was writing about each circulation separately but comparing. For example: many candidates stated ‘hypoxic pulmonary vasoconstriction’, but did not contrast this to ‘hypoxic vasodilation’ for the systemic circulation. Frequently functions of the circulations were limited to gas transport / exchange

Recent Comments