Syllabus (Fourth Edition, 2023)
Topics
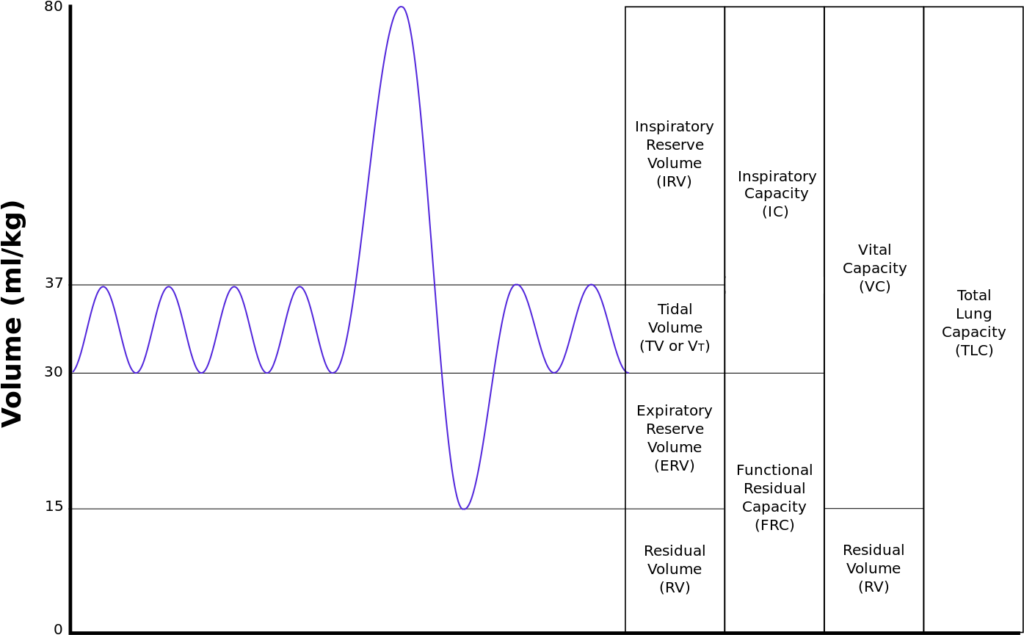
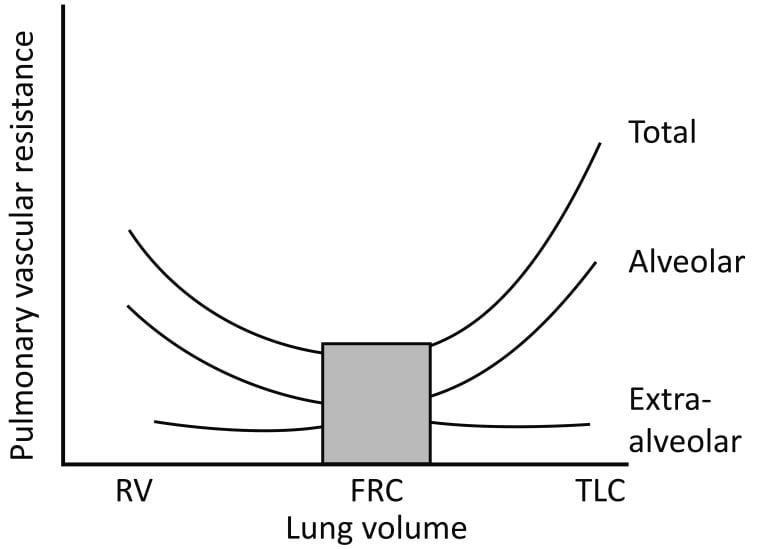
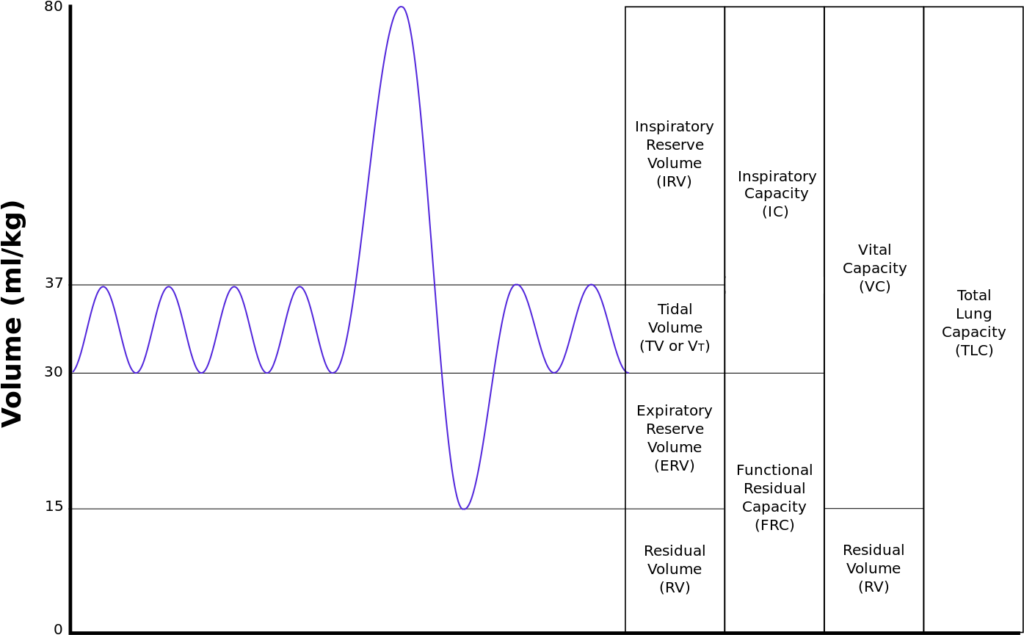
i. State the normal values of lung volumes and capacities.
ii. Explain the factors that influence lung volumes and capacities.
iii. Explain the measurement of lung volumes and capacities.
iv. Define closing capacity, describe the factors that alter closing capacity, its clinical significance and measurement.
Topics not covered in previous SAQs
iii. Explain the measurement of lung volumes and capacities.
Learning Objectives for the First Part Examination in Intensive Care Medicine
- This will ensure that trainees, tutors, and examiners can work from a common base.
- All examination questions are based around this Syllabus.
- These learning objectives are designed to outline the minimum level of understanding required for each topic.
- The accompanying texts are recommended on the basis that the material contained within them provides sufficient information for trainees to meet the learning objectives.
- Trainees are strongly encouraged to explore the existing and evolving body of knowledge of the Basic Sciences as they apply to Intensive Care Medicine by reading widely.
- For all sections of the syllabus an understanding of normal physiology and physiology at extremes of age, obesity, pregnancy (including foetal) and disease (particularly critical illness) is expected.
- Similarly, for pharmacology, trainees are expected to understand a drug’s pharmacology in these contexts.
- An understanding of potential toxicity and relevant antidotes is also expected.
Definitions
Throughout the document specific wording has been used under the required abilities to indicate the level of knowledge and understanding expected and a glossary of these terms is provided.
Definitions
| Calculate | Work out or estimate using mathematical principles. |
| Classify | Divide into categories; organise, arrange. |
| Compare and contrast | Examine similarities and differences. |
| Define | Give the precise meaning. |
| Describe | Give a detailed account of. |
| Explain | Make plain. |
| Interpret | Explain the meaning or significance. |
| Outline | Provide a summary of the important points. |
| Relate | Show a connection between. |
| Understand | Appreciate the details of; comprehend. |
SAQs
i. State the normal values of lung volumes and capacities.
ii. Explain the factors that influence lung volumes and capacities.
2020B 02
Define functional residual capacity (10% marks). Outline the functions (70% marks) of
the functional residual capacity and the factors affecting it (20% marks).
CICMWrecks Answer
Functional residual capacity
- Volume of air in lungs at the end of normal tidal expiration
- Occurs at equilibrium point between the recoil of chest/diaphragm and lungs to collapse inwards
- Sum of residual volume and expiratory reserve volume
- Normal FRC 30ml/kg (approx 2.2l in 70kg male)
Function of FRC
- Oxygen reservoir
- Normally 270mls O2 → can be expanded to 1.8l if breathing FiO2 100%
- PaO2 buffer
- Ensures no fluctuation in PaO2 between inspiration and expiration
- Prevents atelectasis
- Normally FRC above closing capacity
- Decreases V/Q mismatch
- Minimizes work of breathing
- Minimizes airway collapse → resistance decreased
- Minimizes alveolar atelectasis → decreased work required to re-inflate alveoli
- Lung kept at most compliant segment of compliance curve
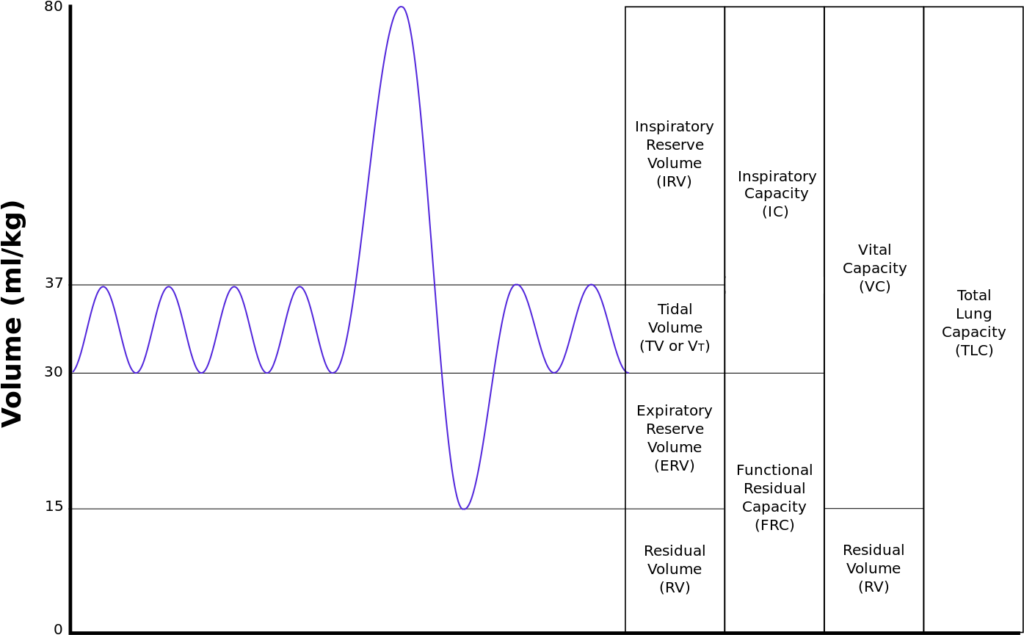
- Decreases pulmonary vascular resistance
- Extra-alveolar and alveolar capillaries kept open
- Minimizes hypoxic vasoconstriction
Factors Affecting FRC
| Factors which increase FRC | Factors which reduce FRC |
|---|---|
| Age | Impaired Lung and chest wall compliance |
| Acute asthma | Increased Intra-abdominal pressure |
| Emphysema | Supine position (by 20%) |
| PEEP Extrinsic Intrinsic (gas trapping) | Anaesthesia (by 20) |
| Upright and Prone position | Obesity |
Sakurai / Gladwin / JC 2020
Examiner Comments
2020B 02: 79% of candidates passed this question.
This question was in two parts with the percentage of marks allocated an indication of the relevant time or detail expected per part. The second part of the question also contained two distinct headings which should have been used in the answer. As an outline question, dot points with a brief explanation of each point were expected. Most candidates drew diagrams, few of which added value. For a diagram to add value it should be accurate, have labelled axes, a scale with numerical values and units. As a general rule, diagrams should also be explained and help to illustrate or relate to a written point.
For factors affecting FRC, to score full marks, it should be clearly stated if the factor causes an increase or decrease in FRC. This topic is well covered in the recommended respiratory texts.
2017A 08 – 2010B 15
Describe the physiological consequences of decreasing Functional Residual Capacity (FRC) by one litre in an adult.
CICMWrecks Answer
Functional residual capacity
- Volume of air in lungs at the end of normal tidal expiration
- Occurs at equilibrium point between the recoil of chest/diaphragm and lungs to collapse inwards
- Sum of residual volume and expiratory reserve volume
- Normal FRC 30ml/kg (approx 2.2l in 70kg male)
- Functions:
- Oxygen reservoir
- PaO2 buffer
- Prevents atelectasis
- Minimizes work of breathing
- Lung kept at most compliant segment of compliance curve
- Decreases pulmonary vascular resistance
Consequence of 1L loss of FRC
- ↑Work of breathing
- FRC is the volume at the minimum work at rest
- Compliance curve shifted to a flatter portion (greater change in pressure required for change in volume)
- FRC < closing capacity → ↑dynamic air closures/↑air trapping → ↑WOB
- ↑atelectasis (↑with supine position) → ↓ lung compliance → ↑WOB
- ↑airways resistance 2° ↓caliber of airway → ↑WOB
- ↑V/Q mismatch
- 2° to dynamic airways closure, gas trapping, atelectasis
- ↑shunt
- ↓PaO2 due to inability of zone 1 to compensate for the larger zone 3
- ↑Pulmonary Vascular Resistance (PVR)
- PVR minimal at FRC
- ↓FRC → ↓radial traction on extraalveolar vessels → ↓radius of vessels → ↑PVR
- ↑PVR → ↑ RV Afterload
- ↓FRC → ↑West Zone 4 → ↑pressure on extraalveolar vessels by poorly inflated lung → ↓radius → ↓flow
- ↓O Store and Buffer capacity
- Greater variability in saturations thoughout the respiratory cycle
- More rapid desaturation with hypoxia
Sakurai / Gladwin / JC 2020
Examiner Comments
2017A 08: 70% of candidates passed this question.
High scoring answers began with a definition and normal values, followed by a detailed list of the consequences of decreasing the FRC.
Some candidates included descriptions of the normal function of FRC, conditions that decrease FRC and ways of improving reduced FRC. These were not required and did not attract marks. Diagrams require correctly labelled axes, values & units.
2010B 15: 5 (33%) of candidates passed this question.
This is core knowledge and it was expected candidates would describe physiological consequences accurately. Good answers included a definition of FRC and correct value. A number of candidates omitted this. It was also expected that candidates mention that as FRC falls, alveolar closure occurs, lung compliance decreases and airway resistance increases work of breathing increases, pulmonary vascular resistance, and thus right ventricular afterload increases. Many candidates described alveolar closure as causing increased dead space ventilation rather than altered V/Q.
Syllabus: B1e References: Nunn’s respiratory physiology, pages 51-56
iii. Explain the measurement of lung volumes and capacities.
2017B 24
What is functional residual capacity (30% of marks)?
Describe two methods of measuring functional residual capacity (70% of marks)
2015B 04
What is functional residual capacity and describe how it is measured.
CICMWrecks Answer
Functional residual capacity
- Volume of air in lungs at the end of normal tidal expiration
- Occurs at equilibrium point between the recoil of chest/diaphragm and lungs to collapse inwards
- Sum of residual volume and expiratory reserve volume
- Normal FRC 30ml/kg (approx 2.2l in 70kg male)
- Functions:
- Oxygen reservoir
- PaO2 buffer
- Prevents atelectasis
- Minimizes work of breathing
- Lung kept at most compliant segment of compliance curve
- Decreases pulmonary vascular resistance
Measurement of FRC
- Cannot be directly measured by spirometry
- Body plethysmography
- Subject contained within glass tight box
- Breath against occluded airway
- Changes in alveolar pressure measured at mouth
- Boyle’s law used to calculate FRC
- Nitrogen wash-out technique
C1V1=C2V2- Initial alveolar concentration of nitrogen = 79% (if breathing room air)
- Subject breathes 100% O2
- Volume of total nitrogen exhaled measured (e.g 4L)
- FRC = 4L/79% = approx 5L
- Helium wash-in technique
C1V1=C2V2- Known volume and concentration of helium inhaled and allowed to
equlibrate but not diffuse into blood - Concentration and volume of exhaled helium measured and used to
calculate FRC, where
- Known volume and concentration of helium inhaled and allowed to
Sakurai / Gladwin / JC 2020
Examiner Comments
2017B 24: 59% of candidates passed this question.
Most candidates could state 2 methods of measuring FRC. Some candidates (especially for nitrogen wash out) failed to provide enough information e.g. statements such as “if the amount of nitrogen is measured then FRC can be derived” were insufficient to score many marks.
2015B 04: 25% of candidates passed this question.
This question requested a definition AND a description of measurement (one method if correctly discussed could and did generate a pass mark) although additional marks were awarded if multiple measurement methods were mentioned or described. Detailed descriptions of the factors effecting FRC and its functions were NOT requested and scored no marks. “Fowlers method” uses 100% oxygen and nitrogen analysis to calculate anatomical dead space – NOT FRC – so scored no marks. Both Helium dilution and nitrogen washout (with 100%oxygen) enable calculation of FRC using C1V1=C2V2 where V2 = V1+FRC. Body plethysmography requires more complex calculations of P1V1= P2V2 (Boyles Law) applied twice = for the box and then the lung. Few candidates had a clear understanding of this method. Most answers did not demonstrate the depth of understanding of the measurement techniques that was required to score highly
iv. Define closing capacity, describe the factors that alter closing capacity, its clinical significance and measurement.
2019B 07
Define closing capacity (10% of marks). Describe the factors that alter it (30% of marks),
its clinical significance (30% of marks) and one method of measuring it (30% of marks).
CICMWrecks Answer
Closing Capacity
- “Lung volume at which small airways and alveoli in the dependent parts of the lung first begin to close”
- Closing capacity = Closing volume + Residual volume
Pathophysiology and clinical significance of closing capacity
- Airways and alveoli in the dependent parts of the lung are much smaller (cf. nondependent regions), thus with expiration to low lung volumes below FRC these dependent airways and alveoli begin to collapse at “closing capacity” and trap gas distally, thereby causing “atelectasis”
- During atelectasis, a shunt forms (V/Q = 0) as the alveoli affected are not ventilated but remain perfused. This leads to impaired gas exchange that results in arterial hypoxaemia
Factors increasing closing capacity
- Age:
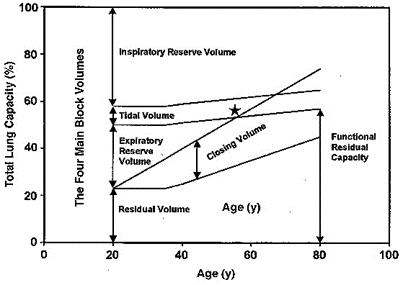
- CC=FRC at 44yrs in supine position, CC=FRC at 66yrs in upright position
- FRC depends on position, CC is independent
- Increasing abdominal pressure
- Decreased pulmonary blood flow
- Pulmonary parenchymal diseases which decrease compliance
- Obstructive airway diseases
- LV failure
- Surgery
Zaugg M, Lucchinetti E. Respiratory function in the elderly. Anesthesiol Clin North America 2000; 18: 47–58
Measuring closing capacity
Closing volume is determined using the “Single breath N2 test” (similar to Fowler’s method):
- Following a VC breath of 100% O2, the patient slowly exhales and a expired [N2] is measured with a rapid N2 analyser
- A plot of [N2] vs volume of gas expired is made:
- Phase 1: N2 in anatomical dead space
- Phase 2: N2 from anatomical dead space and alveolar gas
- Phase 3: Alveolar plateau is formed by N2 in pure alveolar gas
- Phase 4: Late in expiration when AW closure starts of occur, expired [N2] begins to rise above the alveolar plateau. The volume expired from the start of this to the end of maximal expiration is the “Closing volume”
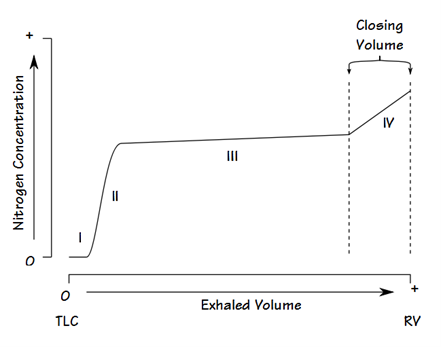
- Basis for phase 4:
- Basal AW closure is indicated by a rise of [N2] from N2-rich apical alveolar gases. Apical alveolar are rich in N2 because:
- During initial inspiration from RV, the first part of inspired gas (which is the anatomical dead space gas rich in N2) goes mainly into the apical alveoli
- Apical alveoli are larger and more poorly ventilated (cf. basal alveoli). Thus, the [N2] of apical alveolar gases are less diluted when breathing in 100% O2
- Basal AW closure is indicated by a rise of [N2] from N2-rich apical alveolar gases. Apical alveolar are rich in N2 because:
Residual volume (RV) cannot be measured directly but is calculated as follows: the FRC is measured using one of three methods: helium dilution, nitrogen washout or body plethysmography. The expiratory reserve volume (ERV) may be measured using standard spirometry. Using the measured FRC and ERV we may calculate RV from the equation: RV = FRC – ERV. Then CC = RV + CV.
Closing capacity is determined by summating “closing volume” and “residual volume”
Source: Bianca’s notes, anaeskey.com
JC 2019
Examiner Comments
2019B 07: 49% of candidates passed this question.
Many candidates confused the factors that affect closing capacity (CC) with factors which affect functional residual capacity (FRC). Some candidates confused airway closure with expiratory flow limitation secondary to dynamic airway compression. A good answer would have included the following: Small airway closure occurs because the elastic recoil of the lung overcomes the negative intrapleural pressure keeping the airway open. Thus, airway closure is more likely to occur in dependant parts of the lung where airways are smaller.
Normally closing capacity is less than FRC in young adults but increases with age. Closing capacity becomes equal to FRC at age 44 in the supine position and equal to FRC at age 66 in the erect position. Closing capacity is increased in neonates because of their highly compliant chest wall and reduced ability to maintain negative intrathoracic pressures. In addition, neonates have lower lung compliance which favours alveolar closure.
Closing capacity is also increased in subjects with peripheral airways disease due to the loss of radial traction keeping small airways open. The consequences of airway closure during tidal breathing include shunt and hypoxaemia, gas trapping and reduced lung compliance. In addition, cyclic closure and opening of peripheral airways may result in injury to both alveoli and bronchioles.
Closing volume (CV) may be measured by the single breath nitrogen washout test or by analysis of a tracer gas such as xenon during a slow exhaled vital capacity breath to residual volume. Residual volume (RV) cannot be measured directly but is calculated as follows: the FRC is measured using one of three methods: helium dilution, nitrogen washout or body plethysmography. The expiratory reserve volume (ERV) may be measured using standard spirometry. Using the measured FRC and ERV we may calculate RV from the equation: RV = FRC – ERV. Then CC = RV + CV.

Recent Comments