Syllabus (Fourth Edition, 2023)
Topics
i. Describe the inspiratory and expiratory processes involving the chest wall, diaphragm, pleura, and lung parenchyma.
ii. Understand compliance (static, dynamic, and specific) and its measurement.
iii. Relate compliance to the elastic properties of the respiratory system.
iv. Describe the pressure volume relationships in the respiratory system.
v. Explain the concept of time constants.
vi. Explain the significance of the vertical gradient of pleural pressure and the effect of positioning.
vii. Describe the pressure-flow and flow-volume relationships of the lung.
viii. Describe the factors affecting airway resistance and its measurement.
ix. Explain the relationship between resistance and respiratory gas flow.
x. Describe the production, properties, and role of surfactant.
xi. Describe the work of breathing and its components.
Topics not covered in previous SAQs
iii. Relate compliance to the elastic properties of the respiratory system.
iv. Describe the pressure volume relationships in the respiratory system.
v. Explain the concept of time constants.
vi. Explain the significance of the vertical gradient of pleural pressure and the effect of positioning.
vii. Describe the pressure-flow and flow-volume relationships of the lung.
ix. Explain the relationship between resistance and respiratory gas flow.
Learning Objectives for the First Part Examination in Intensive Care Medicine
- This will ensure that trainees, tutors, and examiners can work from a common base.
- All examination questions are based around this Syllabus.
- These learning objectives are designed to outline the minimum level of understanding required for each topic.
- The accompanying texts are recommended on the basis that the material contained within them provides sufficient information for trainees to meet the learning objectives.
- Trainees are strongly encouraged to explore the existing and evolving body of knowledge of the Basic Sciences as they apply to Intensive Care Medicine by reading widely.
- For all sections of the syllabus an understanding of normal physiology and physiology at extremes of age, obesity, pregnancy (including foetal) and disease (particularly critical illness) is expected.
- Similarly, for pharmacology, trainees are expected to understand a drug’s pharmacology in these contexts.
- An understanding of potential toxicity and relevant antidotes is also expected.
Definitions
Throughout the document specific wording has been used under the required abilities to indicate the level of knowledge and understanding expected and a glossary of these terms is provided.
Definitions
| Calculate | Work out or estimate using mathematical principles. |
| Classify | Divide into categories; organise, arrange. |
| Compare and contrast | Examine similarities and differences. |
| Define | Give the precise meaning. |
| Describe | Give a detailed account of. |
| Explain | Make plain. |
| Interpret | Explain the meaning or significance. |
| Outline | Provide a summary of the important points. |
| Relate | Show a connection between. |
| Understand | Appreciate the details of; comprehend. |
SAQs
i. Describe the inspiratory and expiratory processes involving the chest wall, diaphragm, pleura, and lung parenchyma.
2010B 14
List the muscles involved in respiration and briefly describe their function.
CICMWrecks Answer
Primary groups of Muscles
| INNERVATION | FUNCTION | |
|---|---|---|
| DIAPHRAGM | ||
| Sheet of skeletal muscle Domed Inserts into lower ribs | Phrenic nerves C3, C4, C5 | Flattens on inspiration – Abdominal contents moved inferiorly → Vertical dimension of thorax increased – Ribs lift and move outwards → Circumference of thorax increased Moves up and down 1cm in tidal breathing can move 10cm in forced inspiration and expiration |
| EXTERNAL INTERCOSTAL MUSCLES | ||
| Insert into superior and inferior borders of ribs Slope inferiorly and outwardly* | Intercostal nerves Anterior rami of thoracic spinal nerves (T1 to T11) | Move the ribs superiorly and outward, increasing circumference of thorax |
| INTERNAL INTERCOSTAL MUSCLES | ||
| Insert into superior and inferior borders of ribs Slope superiorly and inwardly* | Intercostal nerves Anterior rami of thoracic spinal nerves (T1 to T11) | Move the ribs inferiorly and inward, increasing circumference of thorax Not required in quiet breathing, as expiration is passive |
*NSFW:
External Intercostal muscles: ‘hands in pockets’
Internal Intercostal muscles: ‘hands on tits’
Accessory muscles
Accesory inspiratory muscles
(not used in quiet breathing within tidal volume)
- Scalene muscles
- Elevate first two ribs
- Sternomastoids
- Raise the sternum
Accessory expiratory muscles
(not used in quiet breathing within tidal volume)
- Abdominal wall muscles
- Rectus abdominus
- Internal obliques
- External obliques
- Transversus abdominus
- Reduce abdominal cavity volume → Increase abdominal pressure → Diaphragm moves up → lungs decrease in volume
Mooney 2016
Examiner Comments
2010B 14: 5 (33%) of candidates passed this question
Most candidates correctly identified the diaphragm, intercostals, abdominals and accessory muscles as important. However, the majority of candidates omitted to mention the muscles of the larynx, pharynx and airway and thus failed to achieve a good score. Good answers included a detailed description of their function including differentiating between external and internal intercostals. Syllabus: B1b,1, 2a References: Nunn’s respiratory physiology P76 – 80 and West, Respiratory Physiology: the Essentials, pgs 93 – 95
ii. Understand compliance (static, dynamic, and specific) and its measurement.
2022A 03 Define respiratory compliance, include its components and their normal values (25% marks). Explain the factors that affect respiratory compliance (75% marks).
2019B 17 Explain respiratory compliance and outline the factors that affect it.
2017A 14 Define respiratory compliance (20% of marks). Describe the factors that affect it (80% of marks).
2014A 15 What is lung compliance and how is it measured?
2011B 07 Define lung compliance (30% marks). Describe how is it measured (70% marks).
2007B 13 Briefly describe the factors that affect lung compliance.
CICMWrecks Answer

Lung compliance
- Change in lung volume per unit change in transmural pressure
- Normal lung compliance ~200ml/cmH2O
- Static compliance (Cs)
- ” Compliance of lung measured when lung held at constant lung volume”
- no pressure componet due to resistance
- is a function of: Elastic recoil of the lung, Surface tension of alveoli
- Dynamic compliance (Cd)
- ” Compliance of lung measured during cycles of inspiration and expiration”
- includes the pressure required to generate flow by overcoming resistance forces
- is a function of: respiratory rate
- Dynamic Compliance usually < Static Compliance due to the degree of time dependence in the elastic behaviour of a particular lung
- Specific compliance
- Compliance per unit volume lung
- Used to compare different lungs
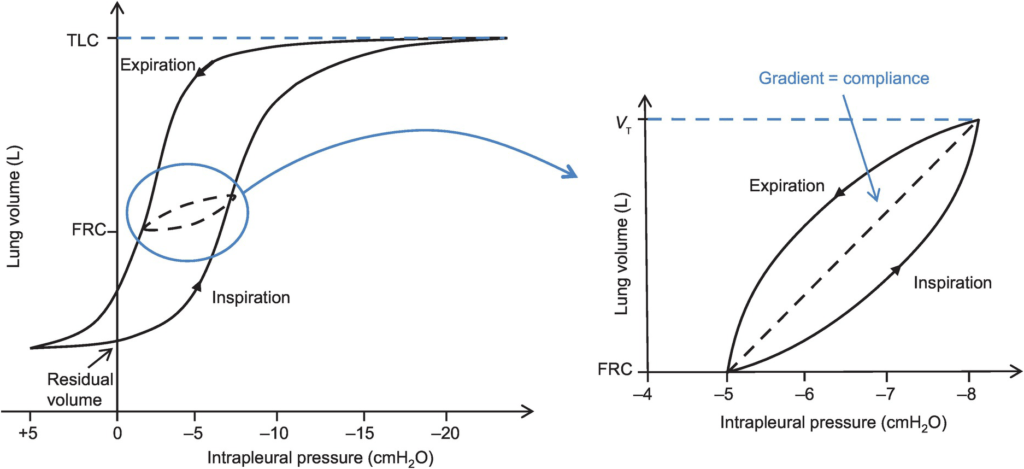
- Hysteresis
- any process where the future state of a system is dependent on its current and previous state
- Compliance of the lung is different in inspiration and expiration
- In dynamic compliance curves:
- Airways resistance is a function of flow rate. Flow rate (therefore resistance) is maximal at the beginning of inspiration and end-expiration.
- In static compliance curves:
- There is no resistive component. Hysteresis is due to viscous resistance of surfactant and the lung.
Factors Affecting Compliance
Lung Compliance
- Surfactant
- increases lung compliance
- decreases surface tension at alveolar air – water interface
- prevents small alveoli from collapsing
- accounts for most of hysteresis in intact lungs
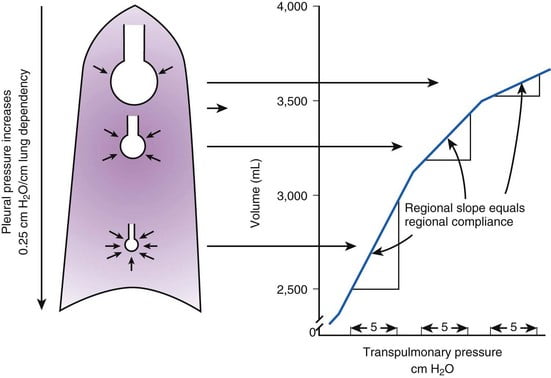
- Lung volume
- Lung Compliance decreases at higher lung volumes
- Specific compliance (Compliance/FRC) remains constant
- Elephants have greater lung compliance than mice!
- Pulmonary blood volume
- Increased PBV decreases lung compliance
- Pulmonary venous congestion from L heart failure or mitral regurgitation
decreases lung compliance
- Bronchial smooth muscle tone
- Increased bronchial smooth muscle tone decreases compliance
- Decreased dynamic lung compliance by 50% in animal models of methacoline
challenge
- Disease
- ARDS, pneumonia decreases lung compliance
- pulmonary fibrosis → Impraired elasticity → decreases lung compliance
- Asthma, Emphysema increases lung compliance
Chest Wall Compliance
- Chest wall restriction – reduced chest wall compliance
- Obesity
- Spastic paralysis of chest wall musculature
- Ossification of costal cartilages
- Kyphosis/scoliosis
- Scarring/constriction (e.g. circumferential burns)
- Position: Prone (60% reduced compliance)
- Collagen Disorders: Increased Chest Wall Compliance
Measurement of Compliance
Dynamic Compliance
- ” Compliance of lung measured during cycles of inspiration and expiration”
- Measure:
- Measure with spirometer
- Using Volume/Pressure curve during normal rhythmic breathing at points of no flow
- Equation above then gives dynamic compliance
Static Compliance
- ” Compliance of lung measured when lung held at constant lung volume”
- Volume vs Pressure loops during inspiration and expiration demonstrate Hysteresis
- Measure:
- @ no flow in or out of the lung, AND time for pressure to equlibrate across the lung (>10sec).
- Patient exhales in steps holding the volume with open glottis
- Intrapleural pressure measured as oesophageal pressure
- Measured compliance secondary to viscoelastic properties and accounts for both short and long time-constant alveoli.
Specific Compliance
- Measure of the average compliance across all lung units
- Children = Adults ~ 0.05 cmH2O-1
Gladwin / Sakurai / JC 2020
Examiner Comments
2022A 03: 27% of candidates passed this question.
This question covers a core principle of respiratory physiology and would be expected to have a high pass rate. Most candidates were able to provide a concise definition and distinguish between the different types of compliance. The imprecise use of terminology often created the impression of a lack of fundamental understanding of this key concept. Candidates are encouraged to be accurate and concise in their definitions. A lack of detail in describing the relevant components of compliance and the factors that influence it, immediately limited the capacity of some candidates to achieve an adequate score.
Most candidates provided less than half of these factors and only provided a list rather than explaining how compliance was impacted. Marks were maximised by dividing the impacts into those that altered lung compliance versus those that impacted on chest wall compliance, and the better candidates explained how and why compliance was affected. Confusion often arose from the imprecise use of arrows with the result that candidates frequently demonstrated an incorrect fact in relation to the direction of the arrow. Candidates are reminded to take care when using abbreviations or arrows to ensure they are not relying on the examiner to interpret a cause and effect relationship.
2019B 17: 51% of candidates passed this question.
Answers were generally well structured. Better answers described lung and chest wall compliance and the pressures which are used to calculate compliance. Better answers displayed an understanding of dynamic, static and specific compliance and provided a reasonably comprehensive list of the physiological factors affecting chest and lung compliance.
2017A 14: 54% of candidates passed this question.
This question was generally well answered with good structure.
2014A 15: 34% of candidates passed this question.
There was a good understanding of the definitions of compliance but many candidates failed to clearly demonstrate an understanding of the difference between static and dynamic compliance. Many candidates had little knowledge of how compliance is measured. It was expected that descriptions of methods to measure static and dynamic compliance would be provided. There were frequent errors in descriptions that were provided
2011B 07: 9 (36%) of candidates passed this question.
This is a core area of physiology that relates to everyday Intensive Care practice, thus it was expected that more than the observed number of candidates would have scored well. Candidates performed poorly purely from a lack of sufficient knowledge. Easy marks were to be gained purely by mentioning that compliance is defined by ∆V/∆P, the ∆P being the gradient from alveolar – intrapleural, normal values, static and dynamic compliance. Good answers would then include a mention of how static and dynamic compliance is measured (specifically how volume and pressures are measured.
Syllabus: B1d 2b
Recommended sources: Nunn Applied Respiratory Physiology, 6th Ed, Pgs 35-36
2007B 13: 1 candidate (14%) passed this question.
Main points/concepts expected in answer.
- Surfactant:
- increases lung compliance
- decreases surface tension at alveolar air-water-interface
- prevents small alveoli from collapsing
- accounts for most of hysteresis in intact lung
- Lung elastic recoil: lung compliance changes in disease states
- Lung volume:
- lung compliance greatest around FRC
- lung compliance reduced at low and high lung volumes
- gravitational effects on regional lung compliance
- Pulmonary blood volume: Pulmonary venous congestion reduces lung compliance
- Lung size: Specific compliance = lung compliance / FRC
- Dynamic lung compliance:
- nfluenced by airways resistance
- lung compliance measured during normal breathing
- less than static lung compliance
- frequency dependence
iii. Relate compliance to the elastic properties of the respiratory system.
iv. Describe the pressure volume relationships in the respiratory system.
v. Explain the concept of time constants.
vi. Explain the significance of the vertical gradient of pleural pressure and the effect of positioning.
2016A 03
Compare the physiology of the apex of the lung with the base of the lung in the upright position.
CICMWrecks Answer
Vertical gradient of pleural pressure and alveoli
Inspiration
- Inspiratory muscle contraction → Overcomes resistance to insp flow → negative alveolae pressure -1cm H2O → VT 500ml
- Weight of lung on alveoli and pleura above:
- causes gradient of pleural pressure: Apex (-10cmH2O) Base (-2.5cm H2O)
- Apical alveoli larger
- But compliance lesser (due to baseline distension)
- Lesser ventilation for same pressure
- Apex and base on different part of compliance curve
Expiration:
- Gradient of pleural pressure smaller
- Apex: -4cm H2O → on steeper part of compliance curve → ventilation better
- Base +3.5cm H2O →airway closure → gas trapping & shunt
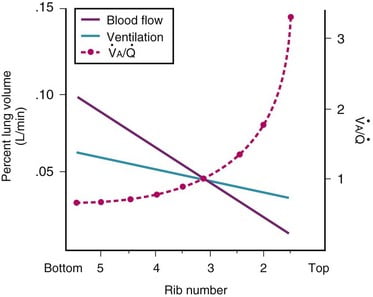
Ventilation, perfusion, V/Q matching
Vertical segments based on V and Q
- Both V and Q ↓ as you move from base to apex.
- ↓ total number of alveoli → ↓ diffusive area → ↓ V
- ↑ compression of intra-alveolar vessels → ↑ west zone 1 → ↓ Q
- V ↓’s slower than Q
| Level | V/Q | Ventilation | Perfusion | PO2 | PCO2 |
|---|---|---|---|---|---|
| Apex | ~3 High | Lower Alveoli largest (no wt of lung) | Very Low Blood hydrostatic pressure low (high gravity) | High 132 | Low 28 |
| At level of heart | ~1 | Slightly more ventilated (Optimized) | Optimized (less effect of gravity) | 108 | 39 |
| Base | ~0.67 towards mixed venous point | Well ventilated (in normal lung): small alveoli, more compliance (effect of wt of lung) | Highly perfused Maximal Hydrostatic pressure | relativly hypoxic 89 | relatively hypercapnoeic 42 |
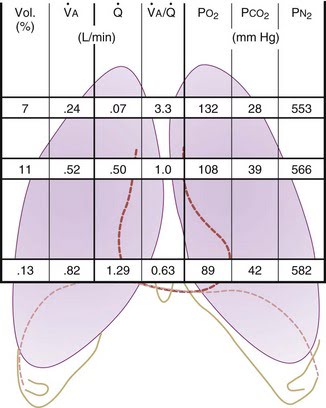
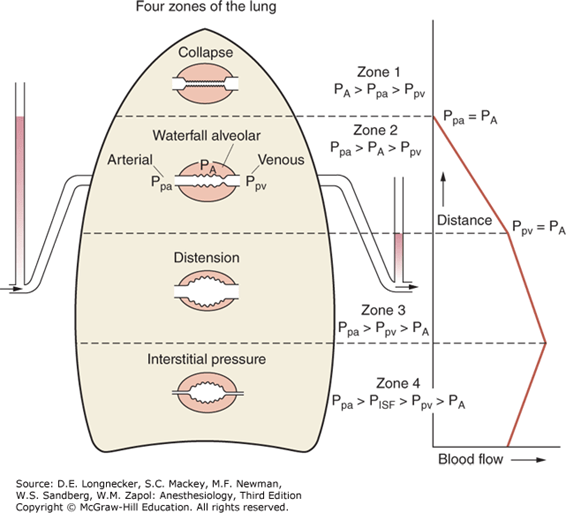
West Zones:
- Divided into zones based on relationship between Alveolar pressure (PA) Arterial pressure (Pa) Venous pressure (Pv) Interstitial pressure (Pi)
- West Zones 1,2,3: Due to changes in hydrostatic pressure when pumping to top of lung vs. bottom of lung
| West Zone | Pressure Relationships | Physiology | Location |
|---|---|---|---|
| Zone 1 | PA > Pa > Pv | No flow of blood, as arterial pressure completely opposed by alveolar pressure | not seen in normal lung |
| Zone 2 | Pa > PA > Pv | Resistance to flow is determined by alveolar pressure (Starling resistor effect) | about 3cm above the heart |
| Zone 3 | Pa > Pv > PA | Resistance to flow is determined by venous pressure Venous pooling causes increased distension of pulmonary capillaries | majority of healthy lung |
| Zone 4 | Pa > Pi > Pv > PA | Low lung volume causes narrowing of extra-alveolar vessels | Lung bases at low lung volume or in pulmonary edema |
JC 2019
Examiner Comments
2016A 03: 33% of candidates passed this question.
The majority of candidates gave extensive detail on West’s zones of the lungs and did not describe other parameters that vary from base to apex. Ventilation, resistance, compliance, alveolar and lung size all vary. Some candidates mixed up the changes at the apex versus the base.
vii. Describe the pressure-flow and flow-volume relationships of the lung.
viii. Describe the factors affecting airway resistance and its measurement.
2021B 12
Explain the physiological factors that affect airway resistance.
2016B 06 – 2009A 18
Describe the factors that affect airway resistance.
2013B 23
What factors affect airway resistance? (80% of marks)
Briefly outline how it may be measured and/or changes in flow are detected. (20% of marks)
CICMWrecks Answer
Airway Resistance
- Resistance is the impedence to flow.
- Normal Airways Resistance (AWR):
- Adult: ~2 cmH2O/L/s
- Newborn: ~20 cmH2O/L/s – declines markedly
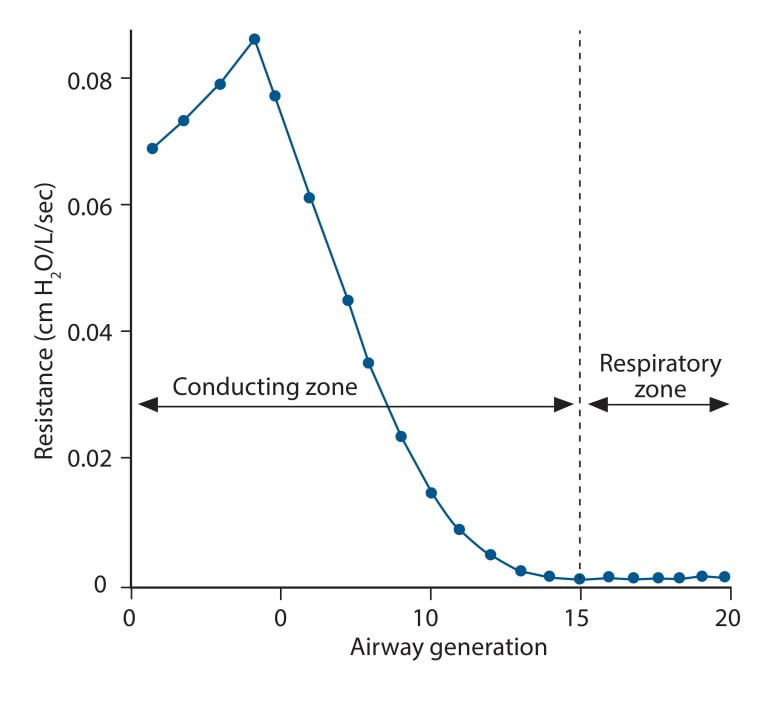
- Main Site of AWR:
- Mid-sized bronchi 7th/8th generation
- comparatively smaller cross-sectional area
- (note that in neonates, a greater proportion of Raw comes from the smaller peripheral airways)
- In the airway flow can be laminar or turbulent
- Flow depends on Depends on Reynolds number
where
Re is Reynold’s number
r is radius
ρ is density
v is velocity
η is viscosity
Laminar Flow
- Ordered flow occuring in concentric layers within a tube
- Flow in the center is fastest and flow in the most peripheral layer is the slowest
- Resistance to laminar flow obeys the Poisuille-Hagen Equation
where
R is vessel resistance
η is viscosity
L is length of vessel
r is radius of vessel
- Increases in viscosity of gas, or length of the tube increase resistance
- Increases in radius of the tube, decreases resistance by a power of 4
Turbulent Flow
- In turbulent flow, due to the disorganized flow and increased likelihood of friction
with the static airway wall, resistance is markedly increased. - Resistance to turbulent flow obeys the following equation
where
R is Resistance to flow
ρ is density
l is length of vessel
r is radius of vessel
- Increases in density of gas, or length of the tube increase resistance
- Increases in radius of the tube, decreases resistance by a power of 5
Factors affecting Airway Resistance
- Physics factors (see above):
- Location in the airway (see above): Mid-sized bronchi are the location of greatest airway resistance, resistance progressively declines with successive airway generations
- Flow:
- Laminar Flow vs turbulent flow
- Depends on Reynolds number factors
- density more important than dynamic viscosity, velocity (flow rate) as Main Site is Turbulent.
- Flow rate:
- Flow related airway collapse
- Airways beyond generation 11 have no structural rigidity
- High flows can reverse transmural pressure gradient and cause airway collapse
- Flow related airway collapse
- Newborn: ~20 cmH2O/L/s – declines markedly with age to ~2 cmH2O/L/s
- Radius changes
- Muscular control of airway diameter
- Neural:
- Parasympathetics important in bronchomotor tone → airway constriction via ACh and muscarinic receptors
- Sympathetic system virtually absent in lung
- Hormonal:
- Although no symppathetic innervation, abundance of β2 adrenoceptors → airway dilation
- Neural:
- Smooth mm tone:
- (↓r) bronchospasm, Musc antag (PSNS), LTs, PGF2-alpha
- (↑r) β2-agonists, adrenaline neb, SNS
- ↓intramural radius:
- oedema, ↑mucous, wall hypertrophy
- External compression:
- tumour, haemorrhage, PTX
- dynamic airways compression with forced expiration
- Muscular control of airway diameter
- Lung Volume
- ↑ lung vol →
- ↑ radial traction → ↓ AWR
- ↑ -ve intrapleural → ↑ patency of small airways
- ↓ lung vol → ↑ AWR
- CPAP or PEEP → ↑ FRC → reduces flow-related airway collapse at low lung volumes
- ↑ lung vol →
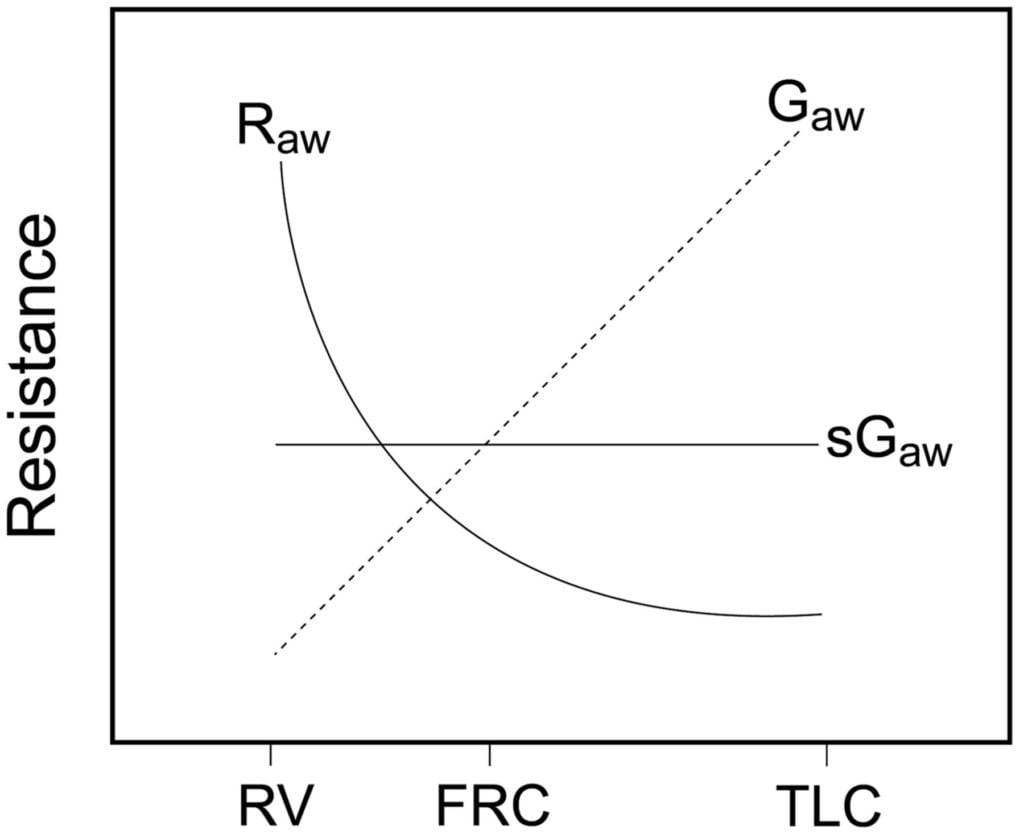
Relationship between Lung volume, Airway Resistance (R) , reciprocal of resistance (Conductance G, specific conductance sG)
Notice that only sGaw is independent of lung volume
Measurement of Airway Resistance
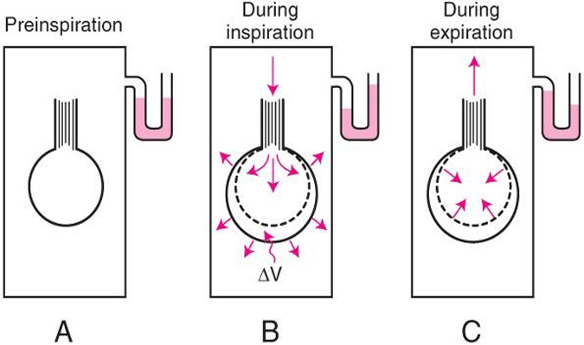
Body Plethysmography:
- Q measured with flow meter
- Lung Volume is measured with Plethysmography
- ∆P via Plethysmography and Boyle’s Law
- (A) box pressure is atmospheric
- (B) inspiration
- ∆V allows for ∆P measurement for given Q since
- PV = constant
- Then AWR can be calculated from 1
Interrupter Technique (direct from AWR eqn)
- Method
- Manometer distal to shutter
- Used to measure mouth and alveolar pressure
- Flow during inspiration or expiration in interrupted for 50–100 ms repeatedly throughout the respiratory cycle.
- Measure
- Q – flow rate (measured before interruption)
- P2 – mouth pressure (measured before interruption)
- P1 – pressure in alveoli (measured at the end of the interruption at te level of the mouth after equilibration)
- Apply Ohm’s Law (AWR equation above).
- Adequate for normal lungs not diseased.
Gladwin / Sakurai 2016
Examiner Comments
2021B 12: 31% of candidates passed this question.
It was expected candidates cover the breadth of the factors that affect airway resistance. Generally, as a concept the type of flow (laminar vs turbulent) was answered well by most candidates, however many failed to mention the other factors that affect airway resistance. Airway diameter as a primary determinant of airway resistance was commonly omitted. Better answers which covered the factors affecting airway diameter classified them broadly and included examples such as physical compression/external obstruction, broncho-motor tone and local cellular mechanisms. Some answers did not explain these factors in enough detail and often with incorrect facts.
2016B 06: 47% of candidates passed this question.
Candidates who used a structured approach of using formulae that describe resistance fluid flow scored well. Poiseuille’s law describes the determinates of resistance to laminar fluid flow and provides a useful answer structure. The most common mistakes were confusion between resistance and compliance as well as failure to describe turbulent as well as laminar flow.
2013B 23: 5 candidates passed (18.5%).
This topic required a definition and understanding of airways resistance. It was expected candidates could identify that issues around the nature of flow (turbulent vs. laminar) and airway diameter were central determinants. It was expected candidates would describe the determinants of turbulent flow.
The provision of formula and comments about Reynolds number helped demonstrate an understanding of this. Better answers discussed the transitional point in the airway and the paradox about size vs. total cross sectional area and its influence on total resistance. Several candidates confused pulmonary vascular resistance with airways resistance. Using graphs to help illustrate certain concepts would have been helpful. Measurement of resistance (indirectly via measurement of flow and pressure difference by a body plethysmography, spirometry) and detection of flow (spirometry, capnography) was in general poorly understood.
2009A 18: Pass rate: 30%
Important factors to be discussed in this answer were anatomical site, laminar versus turbulent flow, airway calibre and factors that affect it such as oedema and sympathetic tone. The effect of lung volume on airway resistance is usefully described in a diagram. The differences in infants earned extra marks
Syllabus B1d, 2h
Reference: Nunn 6th edition p39-47.
ix. Explain the relationship between resistance and respiratory gas flow.
x. Describe the production, properties, and role of surfactant.
2012B 06
Describe the structure of surfactant (25% of marks).
Explain the effects of surfactant upon surface tension and lung mechanics (75% of marks)
CICMWrecks Answer
Surfactant:
- Phospholipoprotein complex
- DPPC – 40%
- Other phospholipids – 40%
- Surfactant-associated proteins – 10%
- Lipids – small amount
- DPCC and other phospholipids have a hydrophilic head, and a hydrophobic tail
- Align themselves on the interior alveolar surface
- Intermolecular forces repel each other, reducing surface tension
In an alveolus:
- Surfactant reduces surface tension, increasing compliance
- Surface tension of surfactant changes with alveolar tension
- At lower volumes, surface tension reduced to near zero
→ Prevents collapse at low volumes - At higher volumes, surface tension rises
→ Prevents overdistension - Shows hysteresis
- At lower volumes, surface tension reduced to near zero
- Surface tension draws fluid out of peri-alveolar capillaries
- Reduced surface tension
→ reduces hydrostatic pressure in capillaries
→ prevents transudate
- Reduced surface tension
Mooney 2016
Examiner Comments
2012B 06: 8 (36.4%) of candidates passed.
The answer required a description of surfactant composition (phospholipids 85%, neutral lipids 5%, and proteins 10%). Phospholipid dipalmitoylphosphatidylcholine is the main surface active component. It was expected candidates would provide a description of the arrangement of the phospholipids with the hydrophilic head in the aqueous phase and the hydrophobic tail in the airspace of the alveolus. The effects of surfactant required an explanation of surface tension and how this affects alveoli. One good way to explain this was describing how La Place’s law would affect alveoli with, and without, surfactant. As the alveoli decrease in size, the surfactant molecules are pushed together and exert a greater surface tension lowering effect. Surfactant is also important in the lung elastic recoil and hysteresis and for alveolar stability preventing collapse and thereby improving lung compliance and decreasing work of breathing. Surfactant also helps oppose the starling forces in the lung and keep fluid from being drawn into the alveoli. Candidates often misunderstood La Place’s law and did not explain how surfactant decreases surface tension.
xi. Describe the work of breathing and its components.
2024B 01
(a) Describe the work of breathing and its components (85% of marks).
(b) Briefly outline the efficiency of the lung (15% of marks).
2021A 02
Describe the work of breathing and its components.
CICMWrecks Answer
Work of Breathing
- WOB = Energy used by the respiratory muscles during ventilation
- Work = Pressure x Volume (measured in Joules)
- represented as area on pressure-vol loop (dynamic compliance curve)
- Tidal breathing at rest: <2% BMR; O2 requirement = 3ml/min
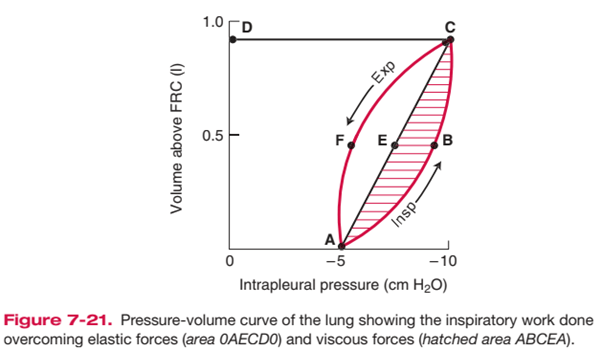
Components of Work of Breathing
WOB can be divided into:
- Inspiratory work
- Active
- Elastic + resistive work
- Expiratory work
- Usually passive (uses potential energy stored during inspiration)
- Resistive work
Inspiratory elastic work
- ~65% of total work
- work done on inspiration to overcome:
- surface tension of lung (70%)
- elastic properties of lung/ lung elastic recoil (30%)
- stored as elastic potential energy → used on expiration
Inspiratory + expiratory resistive work
- ~35% of total work; lost as heat
- energy required to overcome frictional forces: includes
- Airway resistance: between gas molecules
- depends on type of flow + airway calibre
- turbulent flow (↑RR; upper airway obstruction, ↑airway density)
→ ↑ airway resistance than laminar flow - ↓ airway calibre (radius) (e.g. bronchoconstriction, dynamic airway compression, ETT)
→ ↓ calibre → ↑ WOB
- Tissue resistance e.g. interstitial lung disease
- Airway resistance: between gas molecules
- Usually potential energy stored from insp work is sufficient to perform expiratory resistive work → expiration can become active in pathological conditions e.g. COPD, asthma
Total work and efficiency of breathing
- O2 cost of breathing:
- During a normal TV breath at rest, the total work of breathing is low – The
inspiratory muscles consumes 3 mL O2/min, which is ~1% of the body’s total
O2 consumption at rest (VO2 = 250 mL O2/min) - O2 consumption of breathing increases by up to 30% with hyperventilation (due to an increase in either minute volume or RR)
- During a normal TV breath at rest, the total work of breathing is low – The
- Total work and efficiency of breathing:
- Difficult to measure – It is calculated by measuring O2 cost of breathing, then
assuming efficiency as:
- Difficult to measure – It is calculated by measuring O2 cost of breathing, then
Normal efficiency is estimated at 5-10%
Increased WoB
- Elastic Work:
- Breathing large lung volumes: increases total work of inspiration by extending the line AEC to a higher volume above FRC, increasing area 0AECD0
- Poorly compliant lungs (e.g. restrictive disease surfactant deficiency): increases total work of inspiration by reducing slope of AEC, increasing area 0AECD0
- Resistive Work
- e.g. turbulent flow with rapid RR, lung disease associated with increased AWR
- Increases total work of inspiration by producing a larger area ABCEA (i.e. it bulges)
- This also causes AECFA to bulge out and increase area, such that when stored elastic potential is insufficient to overcome this tissue resistance force, expiration becomes an active process requiring work as expiratory muscles are recruited
Minimizing WoB
- Elastic work:
- PEEP: keep lung vol at FRC and maximise number of ventilated alveoli
- Positioning: optimise lung volume
- Surfactant: minimise surface tension
- Optimise RR: elastic WOB ↓s with ↑ RR
- Resistive work
- ↓RR: RR directly proportional to resistive work
- ↑laminar flow: more efficient than turbulent flow; can be ↑ by ↓gas density e.g. heliox
- ↑radius: ↑lung vol; bronchodilators
Kerr / Bianca
Examiner Comments
2024B 01: 29% of candidates passed this question.
This question required candidates to provide a detailed description of the work of breathing and its components. A good answer divided the components into elastic and inelastic/resistive work and provided an overview of the factors that affected each of them. This description was allocated the majority of marks. A thorough answer also discussed the role of expiration on work of breathing, whilst usually a passive process it can be active under some conditions and good answers touched upon these. The second section of the question required an overview of the fate of the energy utilised by the respiratory muscles, with a large proportion lost as heat, or through hysteresis and airway resistance.
2021A 02: 24% of candidates passed this question.
This is a core topic within respiratory physiology. There was a very low pass rate for this question. Expected components of the answer included: a definition of WOB as a product of pressure and volume or force and distance including the units of measurement; followed by a detailed explanation of the following three broad components – elastic resistance, viscous resistance and airflow resistance. Further marks were awarded to situations where the energy for expiration increases beyond stored potential energy as well as the impact of respiratory rate and tidal volume on different aspects of the WOB. For example, the changes in TV will have relatively greater impact on the elastic component, whereas RR will impact the resistance component. Additional marks were awarded for describing the efficiency of breathing. A common area where candidates missed out on marks was producing a diagram of WOB without a description; many diagrams were often incorrectly drawn or had no axes labelled. There were many incorrect definitions or respiratory equations provided without any link to the written answer. Factual inaccuracy and limited depth of knowledge were also prevalent in poorly performing answers. Marks were not awarded for a description of the control of breathing.

Recent Comments