Syllabus (Fourth Edition, 2023)
Topics
i. Describe the anatomy relevant to central venous access (including femoral, internal jugular, external jugular, subclavian and peripheral veins).
ii. Describe the anatomy relevant to the insertion of an arterial line into a radial or femoral artery.
iii. Describe the anatomy relevant to the insertion of an intercostal catheter.
iv. Describe the anatomy relevant to the performance of endotracheal intubation, a cricothyroidotomy and a tracheostomy.
v. Describe the anatomy of the bronchial tree relevant to bronchoscopy.
vi. Describe the anatomy relevant to the performance of a lumbar puncture.
Topics not covered in previous SAQs
i. Describe the anatomy relevant to central venous access (including femoral, internal jugular, external jugular, subclavian and peripheral veins).
ii. Describe the anatomy relevant to the insertion of an arterial line into a radial or femoral artery.
iv. Describe the anatomy relevant to the performance of endotracheal intubation, a cricothyroidotomy and a tracheostomy.
v. Describe the anatomy of the bronchial tree relevant to bronchoscopy.
Learning Objectives for the First Part Examination in Intensive Care Medicine
- This will ensure that trainees, tutors, and examiners can work from a common base.
- All examination questions are based around this Syllabus.
- These learning objectives are designed to outline the minimum level of understanding required for each topic.
- The accompanying texts are recommended on the basis that the material contained within them provides sufficient information for trainees to meet the learning objectives.
- Trainees are strongly encouraged to explore the existing and evolving body of knowledge of the Basic Sciences as they apply to Intensive Care Medicine by reading widely.
- For all sections of the syllabus an understanding of normal physiology and physiology at extremes of age, obesity, pregnancy (including foetal) and disease (particularly critical illness) is expected.
- Similarly, for pharmacology, trainees are expected to understand a drug’s pharmacology in these contexts.
- An understanding of potential toxicity and relevant antidotes is also expected.
Definitions
Throughout the document specific wording has been used under the required abilities to indicate the level of knowledge and understanding expected and a glossary of these terms is provided.
Definitions
| Calculate | Work out or estimate using mathematical principles. |
| Classify | Divide into categories; organise, arrange. |
| Compare and contrast | Examine similarities and differences. |
| Define | Give the precise meaning. |
| Describe | Give a detailed account of. |
| Explain | Make plain. |
| Interpret | Explain the meaning or significance. |
| Outline | Provide a summary of the important points. |
| Relate | Show a connection between. |
| Understand | Appreciate the details of; comprehend. |
SAQs
i. Describe the anatomy relevant to central venous access (including femoral, internal jugular, external jugular, subclavian and peripheral veins).
2021B 08
Describe the anatomy of the internal jugular vein including surface anatomy landmarks relevant to central venous line insertion.
2017B 23
Outline the anatomy of the internal jugular vein relevant to central venous line cannulation (80% of marks).
Include important anatomical variations (20% of marks).
2014A 18
Outline the anatomy of the internal jugular vein. (80% of marks)
Describe the Doppler Effect. (20% of marks)
CICMWrecks Answer: IJV (Internal Jugular Vein) Anatomy
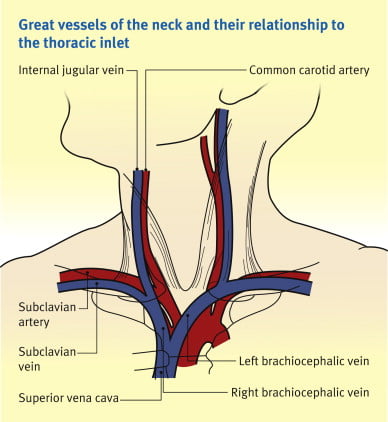
Origin / Course / Termination
- Originates at the jugular foramen where it continues the sigmoid sinus
- Exits the foramen accompanies by the glossopharyngeal (IX), vagus (X) and accessory (XI) nerves
- runs caudally down the neck – The vein lies most superficially in the upper part of the neck
- The vein lies lateral, first, to the internal carotid artery, separated by the hypoglossal (XII) nerve, and then to the common carotid artery, with the vagus nerve between and posterior to the artery and vein.
- These three structures lie in a common fascial compartment (the carotid sheath) with the cervical sympathetic chain lying posterior to the sheath.
- These four structures, two vessels and two nerves, form a quartet throughout the neck.
- The deep cervical chain of lymph nodes lies close against the carotid sheath
- The vein is initially posterior to, then lateral and then anterolateral to the carotid artery during its descent in the neck
- Terminates behind the sternoclavicular joint, where it joins the subclavian vein to form the brachiocephalic vein
Relations of the IJV
- Anterior –
- Internal carotid artery and vagus nerve
- Superficially, the internal jugular vein is overlapped above and then lower down covered by the sternocleidomastoid muscle and is crossed above by the posterior belly of the digastric and lower down by the inferior belly of the omohyoid
- Posterior –
- C1, sympathetic chain, dome of the pleura. On the left side, the IJV lies anterior to the thoracic duct
- Posteriorly, the vein rests on (from above downwards) the rectus capitis lateralis, the transverse process of the atlas, the scalenus medius, and the scalenus anterior, with the phrenic nerve crossing it; and all are covered by the precervical fascia
- Medial – Carotid arteries, cranial nerves IX-XII
Anaesthesia & Intensive Care Medicine,
https://doi.org/10.1016/j.mpaic.2009.10.005.
Surface Anatomy for Venepuncture
- Lies lateral to the carotid artery within triangle formed by: Two heads of Sternocleidomastoid muscle and clavicle
- On Ultrasound: Non-pulsatile, thin walled, compressible vessel lateral to the carotid artery
Anatomical Variations
- The right IJV (80.5%) was more often larger than the left IJV.
- With reference to the CCA, 85.2% of the IJV were found in the lateral position, 12.5% anteriorly, 1.1% medially and 1.1% posteriorly.
- IJV were sometimes found to be hypoplastic, and in rare cases this was seen bilaterally in both the right and left IJV.
- 5.5% have an IJV that does not correspond to the site predicted by external markings
- Other variations:
- IJV bifurcation
- IJV duplication
- IJV fenestration
- IJV trifurcation
- Posterior tributary
Sources:
Ellis H. The clinical anatomy of the great veins of the neck. Br J Hosp Med (Lond). 2010 Feb;71(2):M20-1. doi: 10.12968/hmed.2010.71.Sup2.46501. PMID: 20220708.
Asari AIA, Barros RAV, Borges MAP. Anatomic variant of the internal jugular vein and its importance in vascular access for hemodialysis. J Vasc Bras. 2019 Oct 23;18:e20190014. doi: 10.1590/1677-5449.190014. PMID: 31692937; PMCID: PMC6822959.
Gladwin / JC 2020
CICMWrecks Answer: Doppler Effect
Doppler effect
- Change in apparent frequency of sound for an observer moving relative to its source
- Use in ultrasound
- Sound waves reflected off objects moving toward or away from transducer
(usually blood)- If object moving toward transducer, frequency appears increased – displayed as red (however this is not standardized across machines)
- If object moving away from transducer, frequency appears decreased –
displayed as blue
- Can be used to measure velocity of flow, as well as direction
- Sound waves reflected off objects moving toward or away from transducer
Sakurai 2016
Examiner Comments
2021B 08: 38% of candidates passed this question.
The overall pass rate for this question was poor considering how relevant this area of anatomy is in our daily practice. Better scoring answers used a template including a general description, origin, course and relations, tributaries and as requested in this question, the surface anatomy. Many answers that scored poorly only provided the briefest detail, were vague in their descriptions and incorrect with respect to the facts presented or imprecise with respect to the terminology used.
2017B 23: 14% of candidates passed this question.
Good answers were structured including origin, termination, tributaries, relationships, surface anatomy and common variations.
Factual inaccuracies were common and there was confusion about the relations of the internal jugular vein. Many candidates did not mention the changing relationship between the internal jugular and the carotid artery as they travel through the neck or the changes that result from repositioning for insertion. Many candidates also forgot to mention surface anatomy and a number talked about ultrasound and views used for insertion of central lines. Common omissions included the origin, tributaries, relationship with the correct cranial nerves and the fact that it is usually larger on the right. Almost nobody mentioned the relationship to the pleura
2014A 18: 40% of candidates passed this question.
An overview of the Internal Jugular vein stating where it is formed and terminates would be a good start. The important surface anatomy of the vein (left and right) followed by mention of the important anatomical relationships was then required. Few candidates mentioned anatomical variations.
Many answers had no identifiable structure and went back and forth around the topic as information came to mind. A number of answers contained very rough diagrams that did not contain mark worthy information but took time to draw.
The second part of the question was generally well answered by those attempting it. Many candidates ignored or forgot about this part of the question. Some candidates wrote 2 or more pages of significant detail in stark contrast to what they had written for the first part of the question. The percentage of marks allocated is a good guide as to the level of detail required in the answer.
2022A 18
Describe the anatomy of the left subclavian vein.
2016A 16
Outline the anatomy of the subclavian vein relevant to central venous line insertion.
2013B 18
Describe the anatomy relevant to the cannulation of the left subclavian vein.
2009B 11
Describe and / or illustrate the anatomy relevant for the insertion of a central line into the left subclavian vein using any of the available techniques.
CICMWrecks Answer:
Origin
- Continuation of axillary vein
- Lateral border of 1st rib
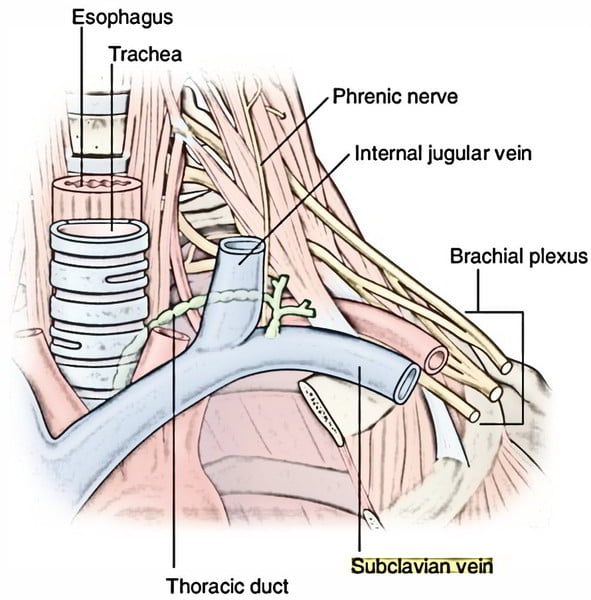
Course
- Follows subclavian artery
- Deep to clavicle
- Superior to 1st rib
Termination
- Deep to sternoclavicular joint at medial border of scalenus anterior
- Joints internal jugular vein to form bilateral brachiocephalic veins vein on left
Relations
- Anterior
- Clavicle, subclavius
- Posterior
- Subclavian artery runs deep/posterior (separated by scalenus anterior)
- Internal mammary artery is posterior medially
- Phrenic nerve is posterior
- Superior
- Skin, superficial aponeurosis
- Inferior
- Apex of lung and 1st rib
- Medial
- Brachiocephalic trunk, thoracic duct and trachea and vagal trunks
- Lateral
- Inferior trunk of brachial plexus
Surface Anatomy
- Clavicle
- Deltopectoral groove
- 2 heads of sternocleidomastoid
- Suprasternal notch
Sakurai 2016
Examiner Comments
2022A 18: 14% of candidates passed this question.
An ideal answer includes origin of subclavian vein, its tributaries, course in relation to mediastinal structures and surface anatomy for central line insertion. Vague comments like: “it follows the subclavian artery”, or “it passes between 1st rib and clavicle”, attract minimal marks. Similarly, no marks were awarded for describing technique of central line insertion and complications of procedure. Answers scored poorly due to a combination of the following, a lack of depth to their answers or inaccurate facts and limited structure/approach to an anatomical SAQ. Good answers described the course of the subclavian vein from its origin at the lateral border of the first rib, along the subclavian groove on the upper surface of the first rib, medially to its termination posterior to the sternoclavicular joint at the medial border of the scalenus anterior, where it joined the IJV to form the bracheoceaphalic vein. In addition, high scoring candidates described tributaries (e.g., the thoracic duct, external jugular) where they joined and went on to describe relations in reasonable detail, specifying whether patient is supine or erect.
2016A 16: 38% of candidates passed this question.
Answers to anatomy questions can be generally structured by considered the origin and ending of the structure, the surface landmarks and the relations (medial / lateral / anterior / posterior) and this would have worked well in this question. It was expected candidates could detail course (from origin to end) and relations of subclavian vein. This could then be used to highlight how these features may be relevant to central venous line insertion (proximity of subclavian artery or pleura creating the possibility of inadverant arterial puncture or pneumothorax. Many candidates failed to mention drainage of external jugular vein and thoracic duct and right lymphatic ducts into the subclavian veins. Candidates should ensure diagrams are accurate and well labelled and they use appropriate anatomical terminology rather than vague terms such as “in front”. Care should be taken ensuring accuracy (e.g. some mentioned dome of diaphragm instead of pleura or IVC instead of SVC)
2013B 18: 9 candidates passed (33.3%).
Understanding the anatomy of the subclavian is essential knowledge in intensive care practice. It was expected that candidates mention where it starts, where it ends, relationship to surrounding structures (in all directions, i.e. medial, lateral, anterior, posterior, etc.) and surface anatomy. In general, relationships and/or surface anatomy was either poorly understood or not mentioned.
2009B 11: 0 (0%) of candidates passed this question.
There are a few areas of anatomy that are essential for Intensivist to have a high level of knowledge of. The subclavian vein is one of them. Unfortunately the extent of knowledge displayed by the candidates was very shallow. A good answer required as a minimum, a clear description of the course of the vein. This included the following facts – it is a continuation of the axillary vein, it’s relationship to the first rib, to the medial border of the scalenus anterior, the fact that it arches up, medial, then down and that it joins the internal jugular vein (behind the subclavian joint, anatomical relationships (eg Anterior – clavicle, subclavius muscle, Posterior – first rib, apex lung superiorly, first intercostal space inferiorly, Superior – subclavian artery, thoracic duct medially, phrenic nerve, lower trunk brachial plexus laterally and Medial – brachiocephalic artery, trachea, vagal trunk, thoracic duct and oesophagus posteriorly) and surface anatomy (related to the various available techniques (eg the infraclavicular and supraclavicular approach)
Syllabus – C1d, 2g
Reference: Anatomy for Anaesthetists, Ellis and Feldman
2024A 08
Describe the anatomy of the femoral vein as it relates to central venous cannulation.
CICMWrecks Answer
Femoral triangle (aka Scarpa’s triangle)
- The major boundaries can be recalled with the mnemonic SAIL:
- lateral border: medial border of sartorius
- medial border: medial border of adductor longus
- superior border: inguinal ligament
- floor: iliopsoas (laterally) and pectineus (medially)
- roof: skin, subcutaneous tissue, a continuation of Scarpa’s fascia, great saphenous vein (joins the femoral vein), superficial lymph nodes, fascia lata
- Contents (From lateral to medial):
- femoral nerve
- femoral sheath (thickening of the deep fascia of the thigh) which has three compartments (from lateral to medial):
- femoral artery and its branches (within the lateral compartment of the femoral sheath) and the femoral branch of the genitofemoral nerve
- femoral vein (within the intermediate compartment of the femoral sheath) and deep lymph nodes
- femoral canal (the medial compartment of the femoral sheath) which contains fat and lymph nodes (of Cloquet)
Femoral sheath
- Situated within the triangle.
- Formed from the fusion and invagination of the psoas and transversalis fascia.
- Contains femoral artery, vein and tributaries, and femoral canal
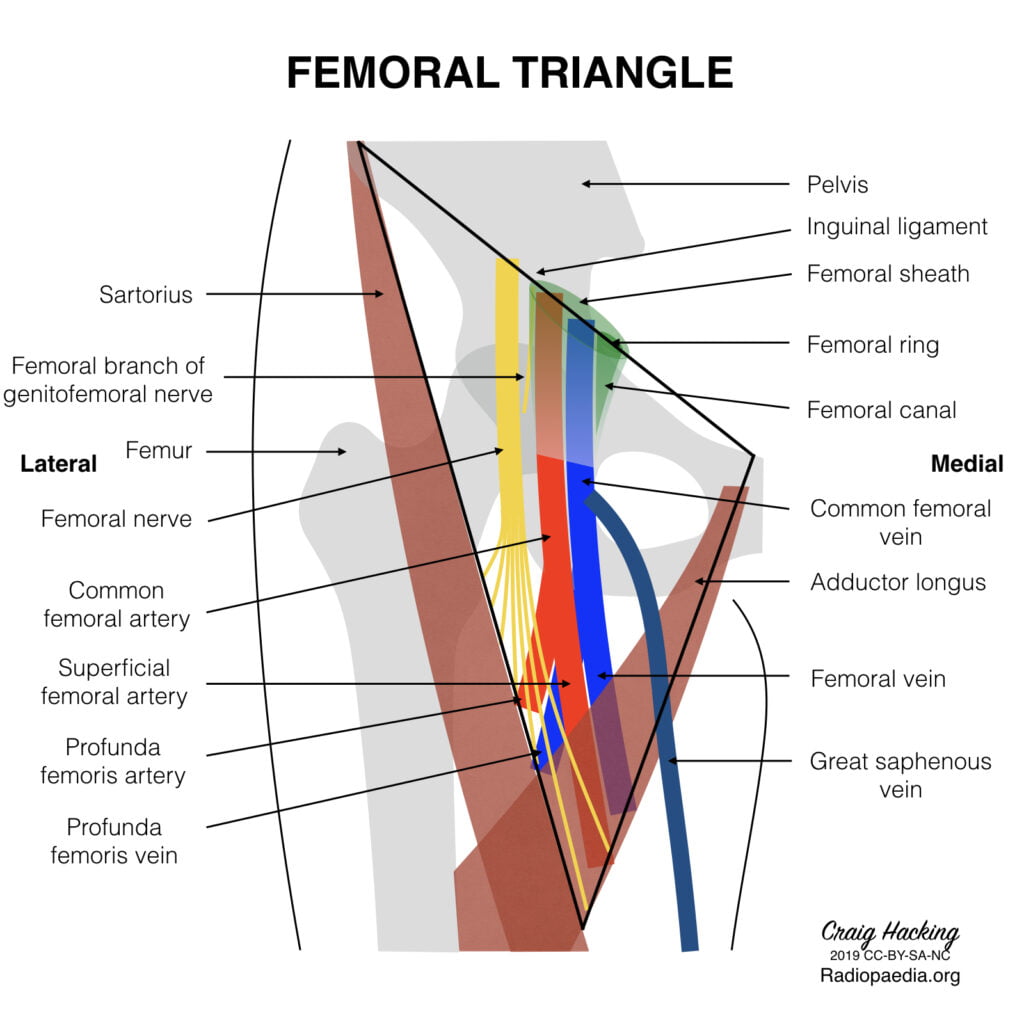
Femoral Vein
Main deep vein of the thigh and accompanies the superficial femoral artery and common femoral artery.
Course:
- Forms as the continuation of the popliteal vein at the adductor opening.
- Proximal to the confluence with the deep femoral vein, the femoral vein is commonly known as the common femoral vein. It becomes the external iliac vein as it ascends posterior to the inguinal ligament.
- In the distal adductor canal, the vein is posterolateral to the superficial femoral artery. Proximally in the canal, the vein lies posterior to the artery in the distal femoral triangle and medial to the artery at the base of the triangle.
- In the upper thigh, the vein is between the common femoral artery and femoral canal and therefore occupies the intermediate/middle compartment of the femoral sheath.
- Tributaries
- numerous muscular tributaries
- profunda femoris vein joins the femoral vein posteriorly 4-12 cm distal to the inguinal ligament
- the great saphenous vein enters anteriorly or anteromedially
- lateral and medial circumflex femoral veins are usually tributaries of the femoral vein
- Surface Anatomy:
- Palpate for the femoral pulse about 1 cm to 2 cm inferior to the inguinal ligament.
- The femoral artery is located at the midpoint between the anterior superior iliac spine and the pubic symphysis.
- With the femoral pulse identified, the femoral vein is about 0.5 cm to 1 cm medial to the pulsation.
Sources: Gray’s Anatomy, Radiopedia
JC 2019
Examiner Comments
2024A 08: 22% of candidates passed this question.
Anatomical questions are best answered with a standard structure that details the location; the boundaries (anterior/posterior, superior/inferior, medial/lateral); a description of the contents of that area and layers; and the relevant surface anatomy. For this question a description of the femoral triangle and boundaries, the origin and termination of femoral vein along with its tributaries, the relationship of the femoral vein to different structures in the triangle and information about femoral sheath and its contents was expected. Marks were also awarded for detailing the surface anatomy of femoral vein relevant to cannulation.
This was an anatomy question as such details of femoral vein cannulation technique, complications and the risks associated with femoral venous access was not required.
2012B 07
Describe the anatomy of the antecubital fossa and peripheral veins of the upper arm relevant to a peripherally inserted central venous catheter (PICC).
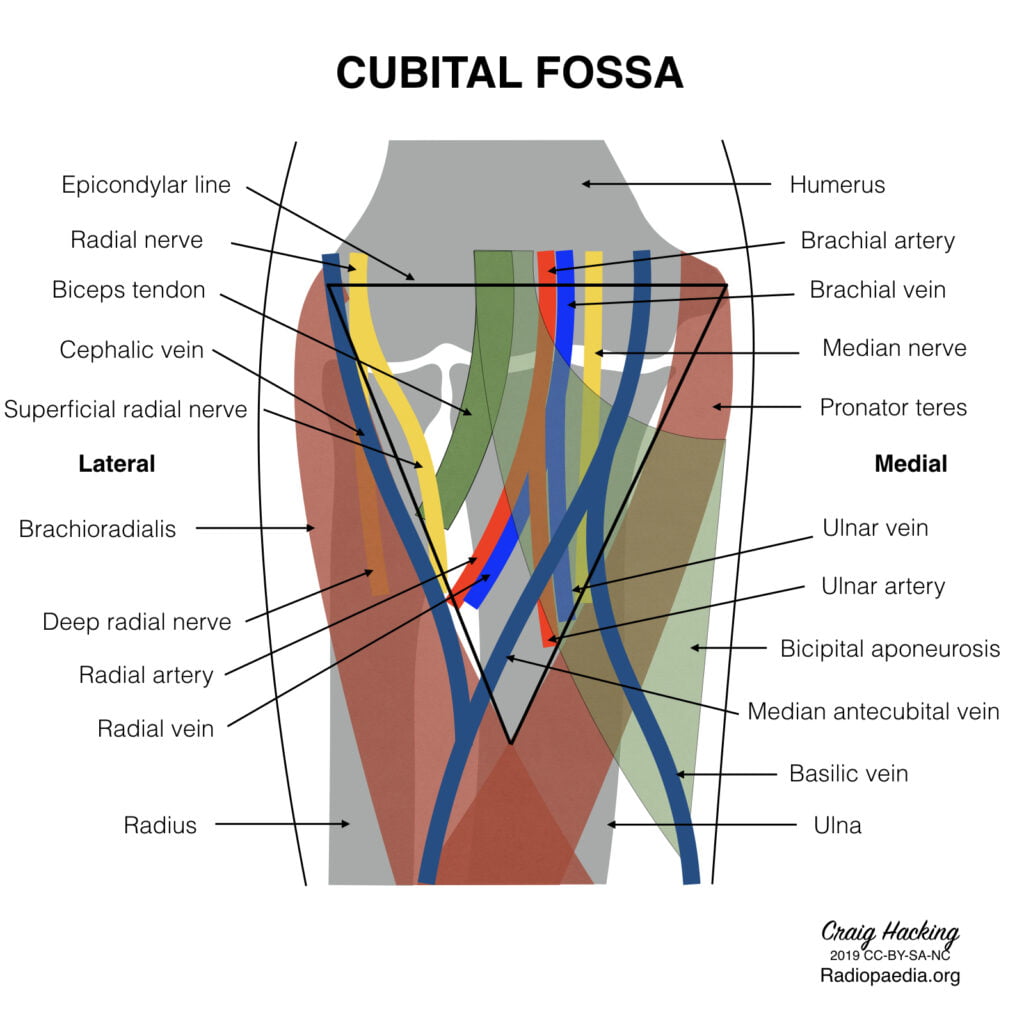
CICMWrecks Answer
Antecubital fossa – a triangular view on the anterior aspect of the elbow
Boundaries
- Medial – lateral border of pronator teres from the medial epicondyle
- Lateral – medial border of brachioradialis from the lateral supraepicondylar ridge of the humerus
- Superior – an imaginary horizontal line connecting the medial and lateral humeral epicondyles
- Inferior – the apex is directed inferiorly and is formed by the meeting point of the medial and lateral boundaries
- Deep (floor) – brachialis (proximal) and supinator (distal) muscles
- Superficial (roof) – skin, superficial fascia (containing the medial cubital vein, lateral and medial cutaneous nerves of
- the forearm, deep fascia (reinforced by the bicipital aponeurosis)
Contents (from medial to lateral)
- Median nerve – leaves the fossa between the two heads of pronator teres
- Brachial artery – bifurcates into the radial and ulnar arteries at the apex of the fossa
- Biceps tendon
- Radial nerve – not strictly in the fossa but is in the vicinity, passing underneath brachioradialis
Venous anatomy in the superficial fascia of the fossa
(from medial to lateral)
- Basilic vein
- commences in the medial forearm, joined by the medial cubital vein at the level of the ACF and then perforates the brachial fascia above the medial epicondyle, joining the brachial veins to form the axillary vein.
- Favoured for PICC cannulation because it is usually of substantial size, with predictable anatomy and is easily viewed with USS.
- Medial cubital vein (variable anatomy)
- Cephalic vein
- commences in the lateral forearm and continues up the lateral aspect of the arm before it enters the deltopectoral groove and empties into the axillary vein.
- Less used for PICC insertion because the presence of the claviopectoral fascia superiorly causes it to enter the axillary vein at an acute angle, which is often difficult for the catheter to negotiate.
Gladwin 2016
Examiner Comments
2012B 07: 5 (22.7%) of candidates passed
Knowledge of anatomy of the areas of the body where common procedures are performed in the intensive care unit is essential. Defining the question by giving the boundaries and contents of the antecubital fossa along with a diagram illustrating the arrangement of the veins would have constituted a pass. The course of the basilic vein and an explanation of why it is favoured over the cephalic vein (presence of the clavipectoral fascia which provides an acute angle for the catheter to negotiate along with a valve frequently located at the junction) was important applied anatomy relevant to PICC line insertion. Transposition of medial and lateral structures was a common error in answers to this question.
ii. Describe the anatomy relevant to the insertion of an arterial line into a radial or femoral artery.
2010A 23
Describe and or illustrate the anatomy relevant to the insertion of an arterial line into the femoral artery
CICMWrecks Answer
Femoral triangle (aka Scarpa’s triangle)
- The major boundaries can be recalled with the mnemonic SAIL:
- lateral border: medial border of sartorius
- medial border: medial border of adductor longus
- superior border: inguinal ligament
- floor: iliopsoas (laterally) and pectineus (medially)
- roof: skin, subcutaneous tissue, a continuation of Scarpa’s fascia, great saphenous vein (joins the femoral vein), superficial lymph nodes, fascia lata
- Contents (From lateral to medial):
- femoral nerve
- femoral sheath (thickening of the deep fascia of the thigh) which has three compartments (from lateral to medial):
- femoral artery and its branches (within the lateral compartment of the femoral sheath) and the femoral branch of the genitofemoral nerve
- femoral vein (within the intermediate compartment of the femoral sheath) and deep lymph nodes
- femoral canal (the medial compartment of the femoral sheath) which contains fat and lymph nodes (of Cloquet)
Femoral sheath
- Situated within the triangle.
- Formed from the fusion and invagination of the psoas and transversalis fascia.
- Contains femoral artery, vein and tributaries, and femoral canal
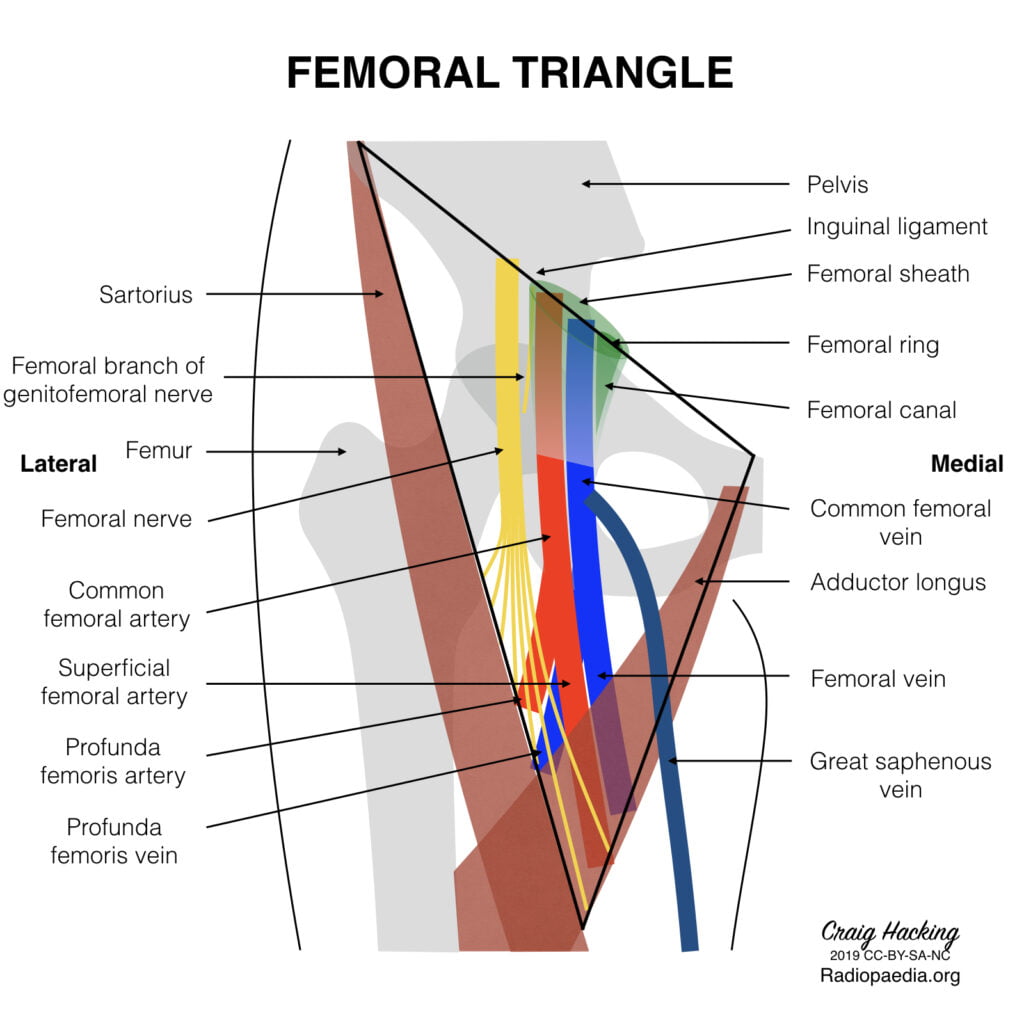
Femoral artery
Main artery of the lower limb, originates as a continuation of the external iliac artery at the level of the inguinal ligament.
Course:
- Enters the femoral triangle deep to the midpoint of the inguinal ligament (clinically the femoral pulse is usually found midway between the ASIS and pubic tubercle), lateral to the femoral vein
- Passes through the triangle and exits at its apex, entering the adductor canal (Hunter’s canal)
- Exits the adductor canal by passing through the adductor hiatus in adductor magnus (at the level of the junction between the middle and lower third of the thigh) to become the popliteal artery.
- Several branches – largest is profunda femoris, the chief artery to the thigh, which arises from the lateral aspect of femoral artery, 2-5cm below the inguinal ligament. Other branches include the superficial epigastric, superficial iliac circumflex and superficial and deep external pudendal arteries.
Relationships:
- Medial – femoral vein (upper part of the triangle)
- Lateral – femoral nerve, lumboinguinal nerve
- Superior – inguinal ligament
- Posterior – posterior part of femoral sheath, pectineal fascia, psoas major tendon, pectineus and adductor longus
- Anterior – skin, superficial fascia lata, lymph nodes, anterior part of femoral sheath
Sources: Gray’s Anatomy, Radiopedia
JC 2019
Examiner Comments
2010A 23: 3 (30%) of candidates passed this question
The femoral artery lies in the femoral triangle. Candidates were expected to describe the content of the triangle. The upper medial and lateral borders of the triangle, the anterior and the posterior relationships of the femoral artery should also be described. The femoral artery is an extension of the external iliac artery and has an important branch, the profunda femoris artery which comes off on the lateral side.
Diagrams gained marks as did mention of common anatomical landmarks to locate the artery. Candidates who failed did not have enough knowledge. Description of how to place an arterial line gained no marks.
Syllabus: C1d2g
References: Grays Anatomy pages 379,526-27,587,497
2017A 13
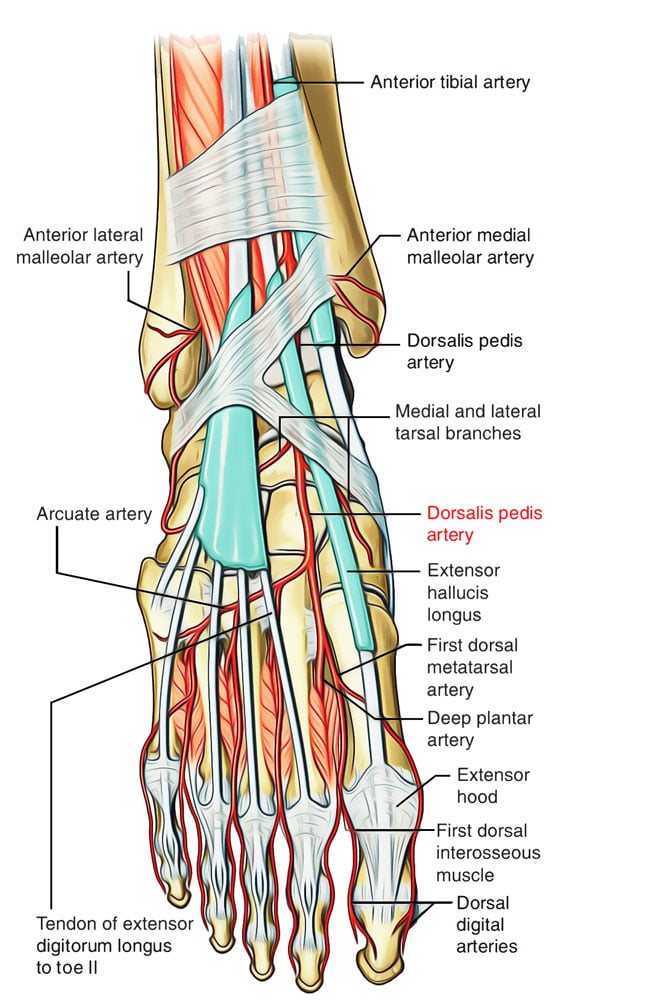
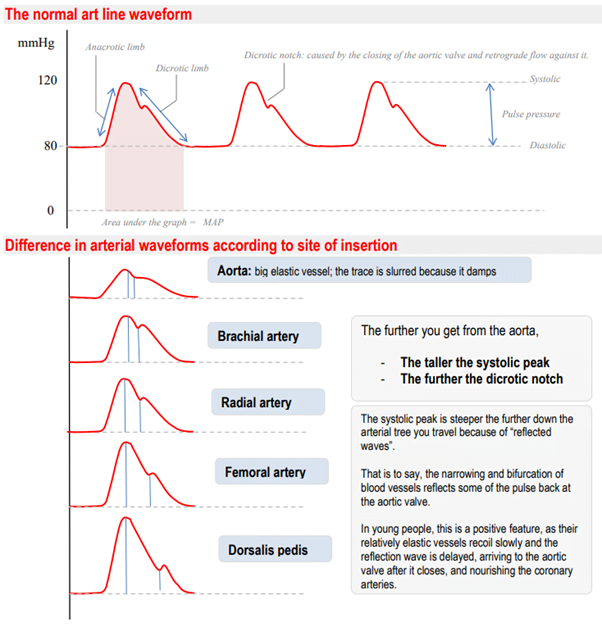
Outline the anatomy relevant to the insertion of a Dorsalis Pedis arterial cannula (50% of marks).
Explain the differences between blood pressure measurement at this site compared to measurement at the aortic arch (50% of marks).
CICMWrecks Answer: Dorsalis Pedis Artery
Dorsalis Pedis Artery
- Origin: Continuation of anterior tibial artery at anterior aspect of ankle joint
- Course: Malleoli, over lower end of tibia à Lateral to extensor hallucis longus
- Base of 1st intermetatarsal space
- Termination: Divides into
- First dorsal Metatarsal artery: terminal branch
- Deep Plantar Artery: communicates with plantar blood supply
- Palpation of the dorsalis pedis artery pulse: On dorsal surface of foot
- lateral to extensor hallucis longus tendon (or medially to extensor digitorum longus tendon)
- distal to the dorsal most prominence of the navicular bone which serves as a reliable landmark for palpation
- Acceptable choice for cannulation under most circumstances
- Although it is absent in up to one eighth of the population
- Loop collateral circulation with branches of Posterior tibial artery
- The posterior tibial artery is a similarly useful vessel for arterial pressure monitoring. Catheters placed in this artery are less susceptible to kinking on dorsiflexion of the foot than in the dorsalis pedis artery, and they may be particularly valuable in neonates and infants
Arterial Line Trace according to site of insertion (Deranged Physiology)
Source: Deranged Physiology – Click to Open
Examiner Comments
2017A 13: 30% of candidates passed this question.
The anatomy component of answers frequently lacked required detail. Many candidates listed the observed differences in the waveforms however an explanation for these differences was required.
iii. Describe the anatomy relevant to the insertion of an intercostal catheter.
2024B 18 – 2018B 11
Describe the anatomy relevant to the insertion of an intercostal catheter.
2013A 14
Describe the relevant anatomy for insertion of an intercostal catheter. (60% of marks)
How does breathing 100% oxygen help in the resolution of a pneumothorax? (40% of marks)
2010B 06
Outline the physiological consequences of a tension pneumothorax. (60% of marks)
Describe the anatomy relevant to the insertion of an intercostal catheter. (40% of marks)
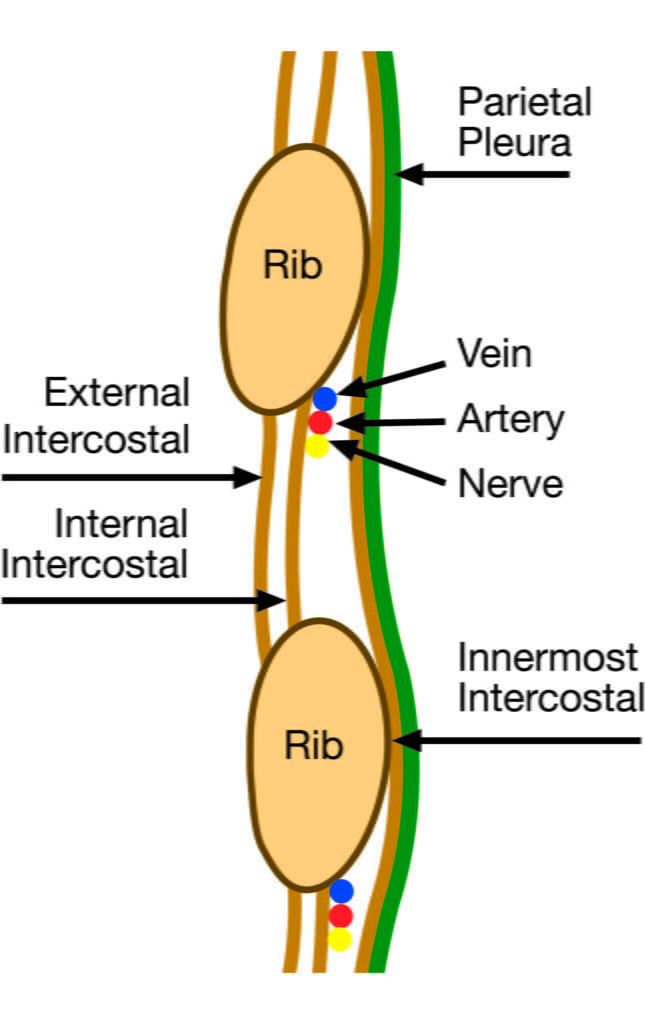
CICMWrecks Answer: Anatomy relevant to ICC Insertion
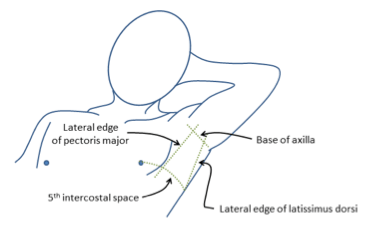
- Triangle of safety
- Lateral border of pectoralis major
- Anterior border of latissimus dorsi
- Superior to the 5th intercostal space – be aware the diaphragm (and liver/spleen) may be unexpectedly superior
- Layers (Superficial → Deep)
- Skin
- Subcutaneous connective tissue
- Fat
- Ribs and intercostal muscles
- Neurovascular bundle (intercostal artery, vein and nerves) lie in intercostal groove on infero-interior surface of the ribs
- External intercostal muscle
- Internal intercostal muscle
- Innermost intercostal muscle
- Parietal pleura
- Potential pleural space (pneumothorax)
- Visceral pleura
- Lung
Sakurai / Mooney 2016
CICMWrecks Answer: Tension Pneumothorax
- Pleura are separated by a thin layer of pleural fluid
- Surface tension keeps membranes apposed
- Balance between elastic recoil of lung tissue (natural tendency of lung to collapse) and elastic recoil of chest wall (natural tendency for chest to expand)
- Normal intrapleural pressure 2.5-6cmH2O
- When air is introduced to pleural space
- Lung not expanded by chest wall → collapse
Tension pneumothorax
- Air enters pleural space via a one-way valve in the lung
- Intrapleural pressure rises dramatically, overcoming closing capacity of one or both lungs, and may exceed right atrial pressure or even aortic pressure
Respiratory:
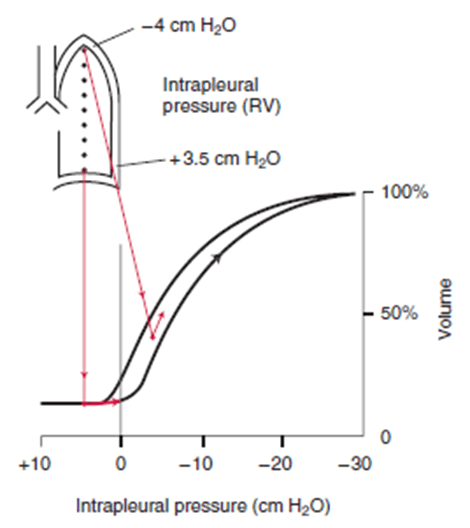
- At low and subatmospheric intrapleural pressures, lung compliance is poor → decreased ventilation → impaired gas exchange → rise in PcCO2, fall in PcO2
- If intrapleural pressure > atmospheric pressure, may exceed compressive resistance of alveoli present at low volumes
- Air moves out of lung → lung collapse
- Falling PO2 and rising PCO2 → stimulation of central and peripheral chemoreceptors → increased work of breathing (tachypnoea without much increase in TV)
V/Q
- Perfusion of lung (dependent on alveolar pressure and lung volume via effect of capillary recruitment and distension on pulmonary vascular resistance) will be maintained up until a point
- In the presence of hypoventilation → V/Q mismatch → fall in PaO2
- Lung perfusion will stop when alveolar pressure rises and lung volume drops
- However, hypoxia will still occur as a tension pneumothorax will cause V/Q mismatch in opposite lung, and may blunt cardiovascular compensation due to impaired cardiac output
Cardiovascular:
- Compression of vena cava and right atrium → decreased preload → decreased stroke volume
- Compression of aorta → increased afterload → decreased stroke volume
- The two above effects, plus hypoxia, may trigger a cardiac arrest
- Compression of ventricles → increased transmural pressure gradient → increased contractility
Mooney 2016
CICMWrecks Answer: 100% O2 in management of Pneumothorax
- Relative composition of gas in pneumothorax = atmospheric gas.
- 21% O2
- 78% N2
- 1% Ar
- Partial pressures depend on pressure within pneumothorax
- Composition of alveolar gas
| Air | 100% O2 | |
|---|---|---|
| PAO2 | = 0.21(760-47) – 40/0.8 = 0.21(713) – 50 = 150 – 50 Approx. 100mmHg | = 1(760-47) – 40/0.8 = 713 – 50 Approx. 660mmHg |
| PACO2 | 40mmHg | 40mmHg |
| PAN2 | 570mmHg | 0mmHg |
- Composition of arterial gas
| Air | 100% O2 | |
|---|---|---|
| PaO2 | Approx. 100mmHg | Approx. 600mmHg |
| PaCO2 | 40mmHg | 40mmHg |
| PaN2 | 570mmHg | 0mmHg |
- Therefore, when breathing 100% O2
- Gradient for N2 reabsorption increases by approx 570mmHg
- Diffusion is proportional to partial pressure difference (Ficks Law) therefore increased reabsorption of N2
- Solubility coefficients = [Dissolved gas] / PP(Gas)
- CO2 – 0.57
- O2 – 0.024
- N2 – 0.012
- N2 requires 2x the partial pressure gradient of O2 to achieve the same amount dissolved in water
Sakurai 2016
Examiner Comments
2024B 18: 36% of candidates passed this question.
This anatomy question reflects the knowledge base of a common ICU procedure. Good answers included insertion sites (lateral and anterior approaches) with the rationale and the relevant surface anatomy including the anatomical boundaries and neighbouring structures (pleural space, heart, liver and spleen) in relation to ICC insertion. A description of the layers of tissues traversed during ICC insertion including mention of the skin, subcutaneous tissues, superficial fascia, external – internal – innermost intercostal muscles, endothoracic fascia and parietal pleura was also required. Specific details describing the importance of the neurovascular bundle including its contents, the origin, trajectory and termination is important as this educates procedural considerations examined in other parts of the curriculum.
2018B 11: 56% of candidates passed this question.
An anatomy question expects the use of anatomical nomenclature to describe relationships.
Good answers defined the “safe triangle” for the lateral approach, soft-tissue layers passed through from skin to pleura and relationship of the neurovascular bundle to the ribs and intercostal muscles. Additional marks were gained for describing the anterior approach and related structures. Common omissions included description of deeper structures (relations) including intrathoracic and intra-abdominal organs and level of the diaphragm with regard to rib space.
No marks were awarded for a description of intercostal catheter insertion
2013A 14:
Many candidates described the technique for insertion of an intercostal catheter which was not requested. Few identified the nerve supply to the area. Most identified the “safe” triangle but failed to correctly identify its borders or draw a diagram to show anatomic landmarks. Describing the anatomy from skin to lungs, including the neurovascular bundle, was needed to pass this part of the question.
Although most knew that 100% oxygen reduce the nitrogen content in a pneumothorax and this accelerates its adsorption, but did not go on to provide any quantification of partial pressure changes in blood and in the pneumothorax bubble.
2010B 06: 9 (60%) of candidates passed this question.
The physiological consequences of tension pneumothorax were in general poorly described. Purely mentioning clinical features (eg distended neck veins) without an associated physiological explanation was not sufficient. Good answers described why tension pneumothorax causes hypoxaemia and hypotension. The cardiovascular mechanism for hypotension and the effect on pulmonary compliance, pulmonary vascular resistance, lung volumes, work of breathing, shunt fraction and carbon dioxide elimination should all have been described.
Many candidates used valuable time making comments about tension pneumothorax being a medical emergency requiring prompt assessment and treatment. These comments attracted no marks, as they were not sought in the question asked. Often the clinical need for insertion of a needle/cannula for decompression was mentioned, but again this attracted no marks.
Description of the anatomy relevant to the insertion of an intercostal catheter was very variable. Most candidates were able to detail the anatomical layers that the catheter had to traverse in order to gain access to the pleural space, and most explained why the catheter should enter the pleural space just above the rib. However, few accurately described where access to the pleural space should be sought and even fewer could explain why. The British Thoracic Society’s ‘safe triangle’ in the axilla and the anatomical boundaries of this were correctly described by very few candidates.
No candidate described an anterior approach through the mid clavicular line, although anatomical details of this approach would have been acceptable.
Syllabus: B1c 1 & B1b 2d
References: Nunn’s respiratory physiology 4th Ed P423, Ganong Review of Medical Physiology 22nd Ed P688
iv. Describe the anatomy relevant to the performance of endotracheal intubation, a cricothyroidotomy and a tracheostomy.
2023B 16 – 2020B 14 – 2015A 24
Outline the anatomy of the larynx.
CICMWrecks Answer
Cartilages
- Unpaired
- Thyroid cartilage – Level of C4~5
- Cricoid cartilage
- Epiglottis
- Paired
- Arytenoid
- Cuneiform
- Corniculate
Muscles
- Intrinsic
- Cricothyroid
- Originates in cricoid cartilage and inserts into thyroid
- Tenses vocal cords and elevates voice
- Thyroarytenoid
- Originates in thyroid cartilage and inserts into arytenoid cartilage
- Relaxes vocal cords and depresses voice
- Posterior cricoarytenoid
- Abducts the vocal cords
- Lateral cricoarytenoid
- Adducts the vocal cords
- Oblique and transverse arytenoids
- Adducts the vocal cords
- Cricothyroid
- Extrinsic
- Strap muscles
Innervation
Sensory
- Internal branch of superior laryngeal nerve
Motor
- Cricothyroid – External branch of the superior laryngeal nerve
- All other intrinsic muscles – Recurrent laryngeal nerve
Blood supply
- Superior laryngean artery (branch of external carotid)
- Inferior laryngeal artery (branch of thyrocervical trunk from subclavian artery)
Associations
- The thyroid glands lie inferolateral to the larynx (lateral to the cricoid, the isthmus is inferior to the cricoid)
- The oesophagus, anterior longitudinal ligament, cervical vertebrae lies posterior to the larynx
- The brachiocephalic trunk may arch superiorly close to the cricothyroid membrane in an anatomical variant
Sakurai 2016
Examiner Comments
2023B 16: 44% of candidates passed this question.
This question required candidates to address the following relevant to the anatomy of the larynx – it’s location and extent; relations; structure (paired and unpaired cartilages; major ligaments; intrinsic and extrinsic muscles); nerve supply (sensory and motor); and blood supply (and venous darinage). There were some marks allocated for other correct information relevant to the anatomy of the larynx (e.g. epithelium; differences in age; lymphatic drainage). This was a purely anatomy question so functions of the larynx was not required.
2020B 14: 40% of candidates passed this question.
For this question, candidates were expected to address the location of the larynx, its relations, the cartilages (single and paired), ligaments, muscles (intrinsic and extrinsic), innervation (sensory and muscular) and blood supply (including venous drainage). Marks were apportioned to each section, so whilst some detail was required, breadth of knowledge was also important. Most candidates had a grasp of the gross anatomy, the main relations and at least the innervation provided by the recurrent laryngeal nerve. However, an understanding of the functional anatomy of the cartilages was not always apparent. It should be noted that not every single muscle needed to be named (especially for the extrinsic muscles), but an understanding of the major muscle groups should have been included.
2015A 24: 13 % of candidates passed this question.
It was expected that an answer would include the names of the three single and three paired laryngeal cartilages, intrinsic and extrinsic muscles (names were not required), nerve supply (motor and sensory) and blood supply. Many candidates had good illustrations though a drawing was not essential.
The majority of candidates failed to name the laryngeal cartilages. There was much confusion about whether certain structures were bones or cartilage or even muscle. The relation of the larynx to the thyroid gland was frequently misunderstood.
Many answers focussed on the relations of the larynx but omitted basic information about the larynx itself. No marks were awarded for the contents of the carotid sheath or the course of the recurrent laryngeal nerve both of which were frequently included in answers.
2018B 01
Describe the surface anatomy of the anterior neck (30% of marks)
and the underlying structures relevant to performing a tracheostomy (70% of marks).
2017A 11
Outline the anatomical relations of the trachea relevant to performing a percutaneous tracheostomy.
2012A 10
Describe the anatomy of the neck and trachea relevant to the insertion of a tracheostomy
2009A 08
Outline the anatomy relevant to performing a percutaneous tracheostomy.
CICMWrecks Answer
Tracheostomy – insertion of a tube through the anterior portion of the neck into the trachea to facilitate ventilation
Trachea Course:
- Larynx connects to the superior part of the trachea at C6 into the thorax and terminates at the level of the sternal angle, where it divides into the right and left mainstem bronchi.
- Initially anterior, then moves posteriorly as it descends to move behind the sternal notch
Tracheal Structure:
- A fibrocartilaginous tube 10cm long, approx 5cm in neck
- Supported by incomplete cartilaginous tracheal rings, which keep the trachea patent.
- The tracheal rings are joined by fibroelastic tissue.
- They are deficient posteriorly where the trachea lies anterior to the oesophagus; the posterior gap is spanned by the involuntary smooth trachealis muscle
Relationships:
- Lateral – carotid sheaths (common carotid arteries, vagus and internal jugular veins), thyroid lobes, inferior thyroid arteries, recurrent laryngeal nerves
- Inferior to the isthmus of the thyroid gland are the inferior thyroid veins
- Posterior – oesophagus, vertebral column
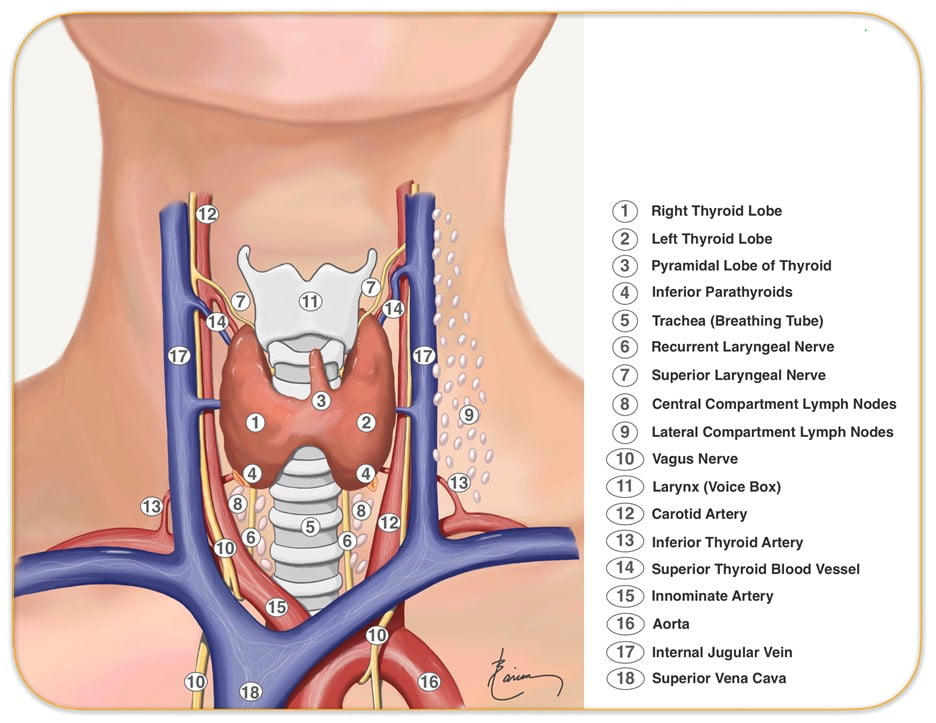
Relevant surface anatomy (in midline of neck):
- Hyoid bone (at level of C3)
- Thyroid cartilage
- Cricothyroid membrane
- Cricoid cartilage (at level of C6)
- Thyroid gland
- Sternohyoid muscle just lateral to midline structures, overlies sternothyroid and thyrohyoid muscles
Layers of dissection in tracheostomy:
- Skin
- Subcutaneous tissue
- Fat
- Pretracheal fascia (superficial and deep)
- Passage through the fibroelastic tissue in between the 1st and 2nd rings (common in perc trache) or 2nd /3rd or 3rd/4th (surgical trache)
- Trachea
Gladwin 2016
Examiner Comments
2018B 01: 79% of candidates passed this question.
Answers required a description of the surface anatomy outlining the midline structures including the hyoid bone and cartilages. The tissue layers should have been mentioned as should the relevant tracheal anatomy. The anterior, posterior and lateral relations of the trachea should also have been included along with the relevant nerves and blood vessels. Diagrams were not essential but could have been included.
Candidates should note that marks were not awarded for a description of how to perform a tracheostomy.
2017A 11: 44% of candidates passed this question.
Many candidates described how to perform a tracheostomy or the structure of the trachea rather than the relevant anatomical relations. It was expected that answers include anterior, posterior and lateral relations at the correct tracheal level including relevant vascular structures.
2012A 10: 4 (40%) of candidates passed.
For a good answer candidates were expected to mention surface anatomy of the anterior of the neck from the superior to inferior aspects (e.g. hyoid bone, thyroid cartilage,
cricothyroid ligament, cricoid cartilage and thyroid gland with sternohyoid muscle just lateral to the midline structures, the pathway of the trachea from anterior at level of larynx to more posterior as it enters the chest behind the sternal notch, nature of the tracheal rings (C shaped cartilages (first cartilage is bigger than the others in the cervical trachea) joined vertically by fibro-elastic tissue and connected posteriorly by the trachealis muscle, layers of dissection for tracheostomy (e.g. skin, subcutaneous tissue, fat, pre-tracheal fascia (superficial and deep), trachea and the relationship of thyroid to the trachea and surrounding vessels. There were some good answers amongst the successful candidates, whereas those who failed to pass this question did so because of a lack of detailed knowledge and relational anatomy. Candidates were not asked, and thus did not receive marks for, describing how to perform a tracheostomy.
2009A 08: Pass rate: 20%
Surface landmarks, anatomy of the trachea and its important relationships with the thyroid, carotid sheath and oesophagus were required to pass this question. Several candidates described the procedure of percutaneous tracheostomy in great detail. Descriptions of the procedure gained no marks.
Syllabus B1b2g
Reference: Anatomy for the Anaesthetist, Ellis and Feldman.
v. Describe the anatomy of the bronchial tree relevant to bronchoscopy.
2019B 05
Describe the anatomical course and relations of the trachea and bronchial tree (to the level of the segmental bronchi).
2016B 24
Outline the tracheal (60% of marks) and left and right main bronchial anatomy (40% of marks) in an adult.
CICMWrecks Answer
Tracheobronchial Tree
Trachea →
Primary main bronchi →
Lobar bronchi →
segmental bronchi (each supplies one bronchopulmonary segment) →
divide dichotomously→→→→
terminal bronchioles →
respiratory bronchioles →
2-11 alveolar ducts →
alveoli
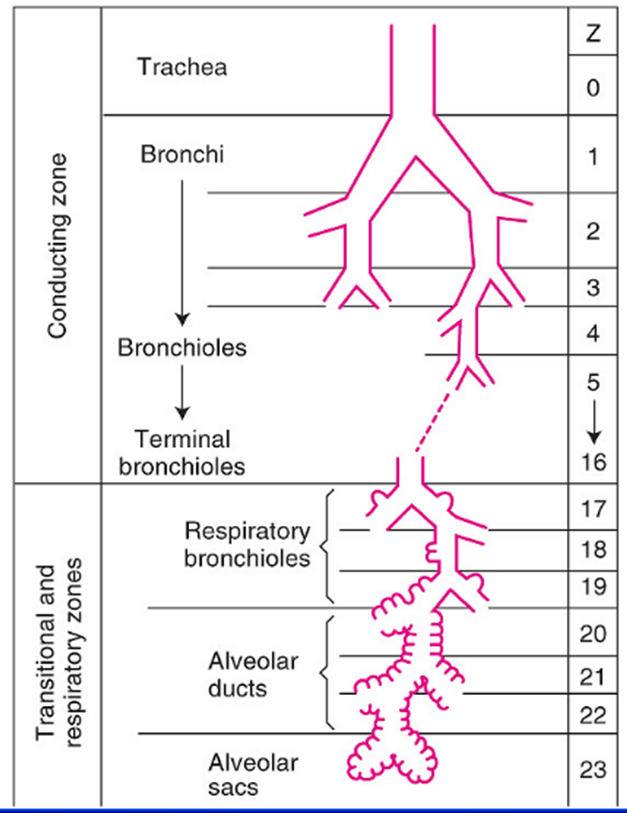
Trachea
- Midline. 10-12 cm long 15-20mm diameter.
- From Cricoid (C6 level) to bifurcation (T4-T6 level)
- 16-20 C-shaped cartilage rings
- Vertical fibroelastic tissue, and posterior trachealis muscle
- Arterial supply: Upper 2/3 – Inferior thyroid artery, Lower 1/3 Bronchial artery
- Venous drainage: Inferior thyroid vein
- Lymphatics: Drain into deep cervical, pre-tracheal, paratracheal lymph nodes
- Nerve supply: Recurrent laryngeal nerve, Sympathetic fibres from middle cervical ganglion
Bronchi
- Supplied by bronchial arteries which run along the bronchi (with vessels from pulmonary circulation)
- Drains into bronchial veins
- Similar innervation as trachea
- A bronchopulmonary segment is a portion of lung supplied by a specific segmental bronchus and arteries.
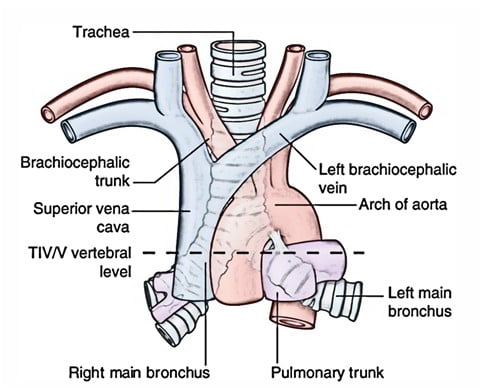
Right main bronchus
2cm long, I.D. 10-16mm
Shorter, wider, more nearly vertical than left
Branches:
- Right upper lobe
- Apical
- Anterior
- Posterior
- Bronchus intermedius
- Middle lobe
- Medial
- Lateral
- Lower lobe
- Superior
- Medial basal
- Anterior basal
- Lateral basal
- Posterior basal
- Middle lobe
Left main bronchus
4-5cm long, I.D. 8-14mm
Crosses anterior to the esophagus, which it indents.
Branches:
- Left upper lobe
- Apicoposterior
- Anterior
- Lingular
- Superior
- Inferior
- Left lower lobe
- Superior
- Anterior basal
- Lateral basal
- Posterior basal
Lining Epithelium
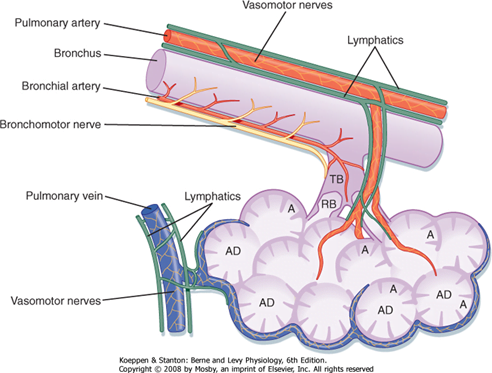
Trachea → Terminal bronchioles: ciliated pseudostratified columnar epithelium
Respiratory bronchioles → alveolar ducts → alveoli: Non ciliated cuboidal epithelium
Sources: Nunn’s Applied Respiratory Physiology, West’s Respiratory Physiology, Berne and Levy Physiology
JC 2019
Examiner Comments
2019B 05: 14 % of candidates passed this question.
To pass this question, the following were required for each section (trachea and main bronchi): landmarks; basic structural anatomy; and important relations (major vessels; major nerves; major structures). Marks were also allocated for innervation, and blood supply and venous drainage of the
trachea. Most unsuccessful answers did not address a number of these areas. Overall, the answers were better for tracheal anatomy compared to bronchial anatomy. A structured approach to anatomy questions works well and this was again the case (i.e. relations / blood supply / etc.
2016B 24: 24% of candidates passed this question.
Better answers included details of the significant structures related to the cervical and mediastinal trachea and bronchi. The lobar branches and bronchopulmonary segments requiring naming to attract full marks. Many answers lacked sufficient detail or contained inaccuracies regarding vertebral levels and key structural relations. Some candidates discussed the general anatomy of the airway, including the larynx, structure of the airways, blood supply and innervation. This did not attract marks.
vi. Describe the anatomy relevant to the performance of a lumbar puncture.
2019A 11
Describe the physiology of cerebrospinal fluid (CSF) (60% of marks).
Describe the anatomy relevant to performing a lumbar puncture (40% of marks).
2013A 02
Describe the physiology of cerebrospinal fluid (CSF). (70% of marks)
Describe the anatomy relevant to the performance of a lumbar puncture. (30% of marks)
CICMWrecks Answer: Physiology of CSF
Formation / Production of CSF
- 60-70% of the CSF is formed by the choroid plexuses
- 30-40% by the cerebral vessels lining the ventricular walls
- Normal rate is 20mL/hour
- Formation independent of ventricular pressure
- Mechanism
- From Coroid Plexus by net transport of Na+, K+, Cl-, HCO3- and water, from plasma to ventricles
- Na down Conc grad
- Others down electro chem grads
Distribution / Circulation of CSF
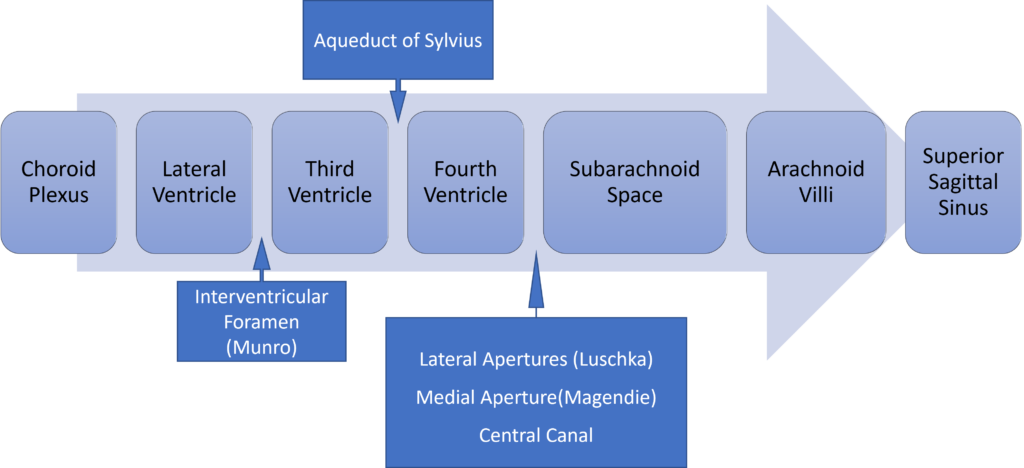
Absorption of CSF
- Absorbed through the arachnoid villi into the cerebral venous sinuses
- Absorption by bulk flow, is proportional to ventricular pressure
- If pressure < 7 cmH2O, CSF absorption ceases
- Above 7cmCSF absorption is linear
- At approximately 11 cmH2O, CSF Absorption = Formation

Composition of CSF
IDENTICAL to brain ECF, but differs in several manners from plasma
Compared with plasma:
- ↑ pCO2 (50 mmHg)
- ↓ pH (7.33)
- ↓ protein content
- 0.5% of plasma; 20 mg/dL
- poor acid-base buffering capacity
- ↓ content of glucose (by 60%) and cholesterol
- ↑ [Cl-] (by 7-14%) and ↑ [Mg2+] (by 40%)
- ↓ [K+] (by 40%), ↓ [Ca2+] (by 50%) and ↓ [Pi] (by 20-30%)
- ↑ creatinine (by 25%) but ↓ urea
- IDENTICAL osmolality (295), [Na+] (145), and [HCO3] (25)
Role / Functions of CSF
- Protective role (main function)
- Water bath effect
- Attributed to the low specific gravity of CSF (1.007)
- Causes brain to be buoyant
- ↓ its effective net weight from 1400 g to 50 g
- Mechanical cushion against acceleration/deceleration forces
- Buffer ↑ ICP by CSF translocation to extracranial subarachnoid space
- Abrupt ↑ ICP buffered by translocation of CSF within the vault to extracranial compartments
- Water bath effect
- Maintains constant ionic environment conducive to neuronal electrical activity CSF
- Supply role of nutrients (Eg simple sugars, amino acids) and O2 to brain
- Excretion of toxic substances, metabolic by-products, and CO2 from brain
- “Lymph-type” function → interstitial proteins in brain ECF return to circulation by
- CSF absorption across arachnoid villi
- Acid-base regulation → due to content, CSF allows for tight respiratory control
- Endocrine transport function → transports hormones to other brain regions
Gladwin / JC 2020
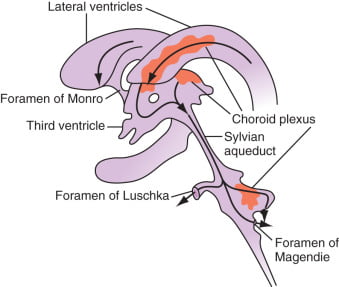
CICMWrecks Answer: Anatomy of LP
Anatomy:
- Position in sitting or lateral decubitus position
- Level:
- Any of the interspaces between between L2-L5
- L4/5 interspace: Tuffier’s Line: line between iliac crests
- (or) L3/4 interspace: Line joining PSISs (Posterior superior iliac spines)
- Discrepancy between identified and actual intervertebral space in 50% of cases
- Conus medullaris ends at L1 in about 94% of patients
Tissues and target for LP:
- In the subarachnoid space between the arachnoid mater and the pia mater.
- The tissues pierced are (in order):
- skin
- subcutaneous tissue
- supraspinal ligament,
- interspinal ligament,
- ligamentum flavum,
- dura mater,
- the arachnoid mater into the subarachnoid space.
- Lateral/paraspinal approach: Skin – subcutaneous tissue – erector spinae muscles – ligamentum flavum – dura – arachnoid – subarachnoid space
Epidural Space
- Posterolateral Epidural Space
- Posterolateral epidural space extends vertically down the spinal canal and contains arteries, venous plexus, and fat
- Posterolateral epidural space is larger than the anterior epidural space
- Posterolateral epidural space is larger in the sacral region than it is in the cervical region
- Anterior Epidural Space
- Anterior epidural space is a virtual space under normal circumstances (due to adherence of dura to bone of vertebral bodies from the foramen magnum down to L1)
Gladwin / JC 2020
Examiner Comments
2019A 11: 86% of candidates passed this question.
Better answers had a structure with headings such as function, formation, circulation, absorption and composition with dot point facts under each heading. The second part of the question lent itself to a diagram with labelling which scored well. Precise surface anatomy and mentioning all layers from the skin to the sub-arachnoid space scored well.
2013A 02:
Most candidates performed well in this question. The physiology of cerebrospinal fluid (CSF) required candidates to write about CSF formation, circulation and absorption, compare the composition of CSF to plasma and describe normal volumes and pressures. The functions of CSF also need to be listed. Some candidates described the displacement of CSF when intracranial pressure rises as a function of CSF. No marks were given for this.
The best approach to the anatomy of a lumbar puncture was to describe the lumbar intervertebral space at which the lumbar puncture is done and then describe the anatomical structures that the needle would traverse from the skin to the subarachnoid space. Mentioning the indications for a lumbar puncture was not required.
2015B 07
Draw and label a cross section of the lumbar epidural space (50% of marks).
Describe the pharmacology of bupivacaine (50% of marks).
CICMWrecks Answer: Anatomy of LP
Anatomy:
- Position in sitting or lateral decubitus position
- Level:
- Any of the interspaces between between L2-L5
- L4/5 interspace: Tuffier’s Line: line between iliac crests
- (or) L3/4 interspace: Line joining PSISs (Posterior superior iliac spines)
- Discrepancy between identified and actual intervertebral space in 50% of cases
- Conus medullaris ends at L1 in about 94% of patients
Tissues and target for LP:
- In the subarachnoid space between the arachnoid mater and the pia mater.
- The tissues pierced are (in order):
- skin
- subcutaneous tissue
- supraspinal ligament,
- interspinal ligament,
- ligamentum flavum,
- dura mater,
- the arachnoid mater into the subarachnoid space.
- Lateral/paraspinal approach: Skin – subcutaneous tissue – erector spinae muscles – ligamentum flavum – dura – arachnoid – subarachnoid space
Epidural Space
- Posterolateral Epidural Space
- Posterolateral epidural space extends vertically down the spinal canal and contains arteries, venous plexus, and fat
- Posterolateral epidural space is larger than the anterior epidural space
- Posterolateral epidural space is larger in the sacral region than it is in the cervical region
- Anterior Epidural Space
- Anterior epidural space is a virtual space under normal circumstances (due to adherence of dura to bone of vertebral bodies from the foramen magnum down to L1)
Gladwin / JC 2020
CICMWrecks Answer: Pharmacology of Bupivacaine
Examiner Comments
2015B 07: 35% of candidates passed this question.
It was expected answers would include a diagram of a cross section and label the lumbar epidural space and the key landmarks namely dura, subarachnoid space, epidural space. Most candidates were able to give a schematic representation even if not being able to draw. Some candidates confused the subdural space with the epidural space. Pharmacology of bupivacaine needed to cover both pharmacokinetics and pharmacodynamics. Several candidates addressed only one of these components and so missed the opportunity to score marks.



Recent Comments