Syllabus (Fourth Edition, 2023)
Topics
V1: Obstetric Physiology
i. Explain the physiological changes during pregnancy and parturition.
ii. Outline the functions of the placenta and the determinants of placental blood flow.
iii. Describe the transfer of nutrients, drugs and gases between mother and foetus including the double Bohr and Haldane effects.
iv. Describe the transition from foetal to neonatal circulation and the establishment of ventilation.
v. Describe the physiological consequences of changes in posture during pregnancy including the consequences of aorto-caval compression.
V2: Obstetric Pharmacology
i. Describe the pharmacology of oxytocic drugs.
ii. Describe the pharmacology of tocolytic drugs.
Topics not covered in previous SAQs
V1: Obstetric Physiology
iii. Describe the transfer of nutrients, drugs and gases between mother and foetus including the double Bohr and Haldane effects.
v. Describe the physiological consequences of changes in posture during pregnancy including the consequences of aorto-caval compression.
V2: Obstetric Pharmacology
i. Describe the pharmacology of oxytocic drugs.
ii. Describe the pharmacology of tocolytic drugs.
Learning Objectives for the First Part Examination in Intensive Care Medicine
- This will ensure that trainees, tutors, and examiners can work from a common base.
- All examination questions are based around this Syllabus.
- These learning objectives are designed to outline the minimum level of understanding required for each topic.
- The accompanying texts are recommended on the basis that the material contained within them provides sufficient information for trainees to meet the learning objectives.
- Trainees are strongly encouraged to explore the existing and evolving body of knowledge of the Basic Sciences as they apply to Intensive Care Medicine by reading widely.
- For all sections of the syllabus an understanding of normal physiology and physiology at extremes of age, obesity, pregnancy (including foetal) and disease (particularly critical illness) is expected.
- Similarly, for pharmacology, trainees are expected to understand a drug’s pharmacology in these contexts.
- An understanding of potential toxicity and relevant antidotes is also expected.
Definitions
Throughout the document specific wording has been used under the required abilities to indicate the level of knowledge and understanding expected and a glossary of these terms is provided.
Definitions
| Calculate | Work out or estimate using mathematical principles. |
| Classify | Divide into categories; organise, arrange. |
| Compare and contrast | Examine similarities and differences. |
| Define | Give the precise meaning. |
| Describe | Give a detailed account of. |
| Explain | Make plain. |
| Interpret | Explain the meaning or significance. |
| Outline | Provide a summary of the important points. |
| Relate | Show a connection between. |
| Understand | Appreciate the details of; comprehend. |
SAQs
V1. Obstetric Physiology
i. Explain the physiological changes during pregnancy and parturition.
2023A 18
Explain the respiratory changes that occur at term in pregnancy.
2020A 18
Describe the respiratory changes that occur throughout pregnancy
2014A 04
Describe the respiratory changes during pregnancy.
CICMWrecks Answer
Respiratory Changes In Pregnancy
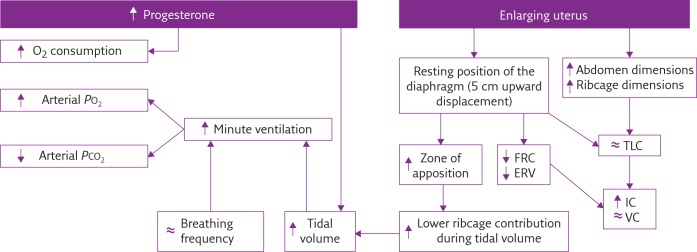
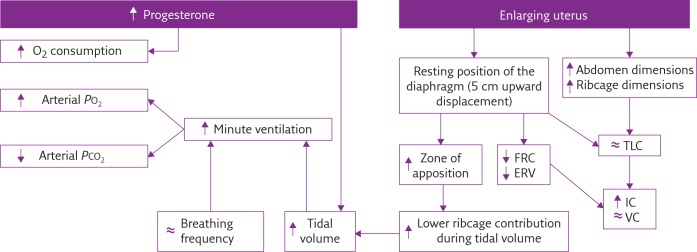
Anatomical
- Diaphragm ascends ~4cm due to foetus
- AP and lateral diameters of thorax increase 2~3cm due to relaxin effect on chest
wall - Thoracic circumference increases 5~7cm (AP and lateral diameters increased 2~3cm)
- Airway dilatation → decreased resistance (35%) and increased deadspace (45%)
- Increased cardiac output, intravascular volume, and decreased oncotic pressure
- Increased plasma volume → increased pulmonary blood volume → decreased compliance
- Venous engorgement → Upper airway oedema
Mechanical
- Lung volume changes occur from 20 weeks
- TLV decreases 5% from baseline
- FRC decreased 20% due to both ERV and RV
- Significant postural change in FRC of 70%
- Progesterone → increased sensitivity to CO2 → Minute ventilation increases 50%
- TV increases (25%)
- RR increases
- Results in hypocarbia and compensated respiratory alkalosis
- pCO2 ~ 26-32mmHg
- HCO3 ~ 18-20mmol/l
- Further increase in MV during contractions
- Inspiratory capacity increased by 10%
- Closing capacity unchanged
- Increased O2 consumption during labour (60%)
After birth
- FRC and RV return to normal within 48 hours
- TV returns to normal within 5 days
Sakurai 2016
Examiner Comments
2023A 18: 43% of candidates passed this question.
Good answers addressed the following in an ordered way: anatomic changes (including to airway, thoracic dimensions, dead space, airways resistance); what changes there are to respiratory volumes, capacities, and compliance; what happens to oxygen consumption and oxygen tension; and the acid-base changes that occur. Good answers didn’t just list these changes, but also provided an explanation for them. Few candidates mentioned the changes in oxygen tension and oxygen consumption, and why these occurred.
2020A 18: 31% of candidates passed this question.
The question asked for a description of the respiratory changes throughout pregnancy, which includes labour. Simple lists of changes did not score highly. A straightforward structure including; first, second and third trimester delineation would have elevated many answers from below par to a pass. Many good answers gave succinct detail on both mechanical respiratory changes and the hormonal mechanisms behind them. Higher scoring answers also described the overall effect of individual changes to spirometry, geometry or respiratory control.
2014A 04: 26% of candidates passed this question.
This question was variably answered, with a wide range of marks. Candidates often mentioned central regulation, anatomy, respiratory mechanics, static lung volumes or gas transfer, but did not provide comprehensive cover of all areas. Very few clearly described the extent of any change (either as a percentage or actual amount relative to the non-pregnant state). A number of candidates presented information well in diagrammatic form (e.g. static lung volumes) however then repeated this same information in text, which was unnecessary.
2012A 13
Draw (include labels and normal values) a normal spirometry trace in a young adult (20% of marks).
Describe the changes seen in the spirometry, and the respiratory system overall, in pregnancy at term (80% of marks).
CICMWrecks Answer
Normal Spirometry trace
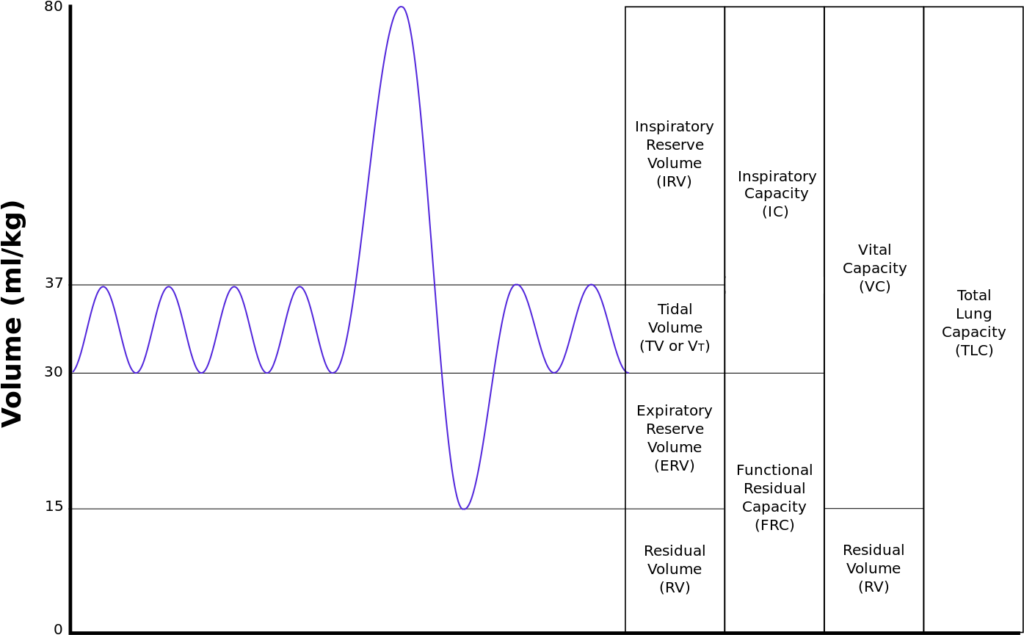
| Inspiratory reserve volume | 45ml/kg | 3 L |
| Tidal volume | 7ml/kg | 500 ml |
| Expiratory reserve volume | 15ml/kg | 1.1 L |
| Residual volume | 15ml/kg | 1.1 L |
| Total Lung Capacity | 82ml/kg | 5.7 L |
| Vital Capacity | 67ml/kg | 4.6 L |
| Functional Residual Capacity | 30ml/kg | 2.2 L |
In Pregnancy
Anatomical
- Diaphragm ascends ~4cm due to foetus
- AP and lateral diameters of thorax increase 2~3cm due to relaxin effect on chest
wall - Thoracic circumference increases 5~7cm (AP and lateral diameters increased 2~3cm)
- Airway dilatation → decreased resistance (35%) and increased deadspace (45%)
- Increased cardiac output, intravascular volume, and decreased oncotic pressure
- Increased plasma volume → increased pulmonary blood volume → decreased compliance
- Venous engorgement → Upper airway oedema
Mechanical
- Lung volume changes occur from 20 weeks
- TLV decreases 5% from baseline
- FRC decreased 20% due to both ERV and RV
- Significant postural change in FRC of 70%
- Progesterone → increased sensitivity to CO2 → Minute ventilation increases 50%
- TV increases (25%)
- RR increases
- Results in hypocarbia and compensated respiratory alkalosis
- pCO2 ~ 26-32mmHg
- HCO3 ~ 18-20mmol/l
- Further increase in MV during contractions
- Inspiratory capacity increased by 10%
- Closing capacity unchanged
- Increased O2 consumption during labour (60%)
After birth
- FRC and RV return to normal within 48 hours
- TV returns to normal within 5 days
Sakurai 2016
Examiner Comments
2012A 13: 5 (50%) of candidates passed.
This question was generally handled well. Significant variation exists in normal values between textbooks, and examiners took account of this variation. Some candidates failed to provide any normal values or gave values not in accord with the traces they provided. Some candidates confused spirometry (volume/time) with flow volume loops or even a forced expiratory volume trace. These scored no marks. The second part was not well answered by some candidates with failure to describe changes – or even contradicting correctly graphed changes (for example the reduction in residual volume with pregnancy described as increased). Memorising curves needs to be accompanied by understanding. No marks were awarded for detailed discussion of the Haldane effect, as this was not asked. Candidates are reminded to read and answer the question.
2010A 11
Describe a set of arterial blood gases in a pregnant woman at term and the reasons for these values.
CICMWrecks Answer
| pH | 7.41 |
| PaO2 | 102 mmHg |
| PaCO2 | 30 mmHg |
| HCO3– | 18 mmol/L |
| BE | -2~3 |
pH
- Respiratory Alkalosis → pH increases
- Complete renal compensation → pH normalizes
PO2
- Alveolar PO2 increases according to alveolar gas equation
- As PaCO2 decreases from 40 → 30mmHg
- PAO2 = 150 – 37 = 113mmHg
- However there is increased O2 consumption (15~30% above normal) in the hypermetabolic state → PaO2 ~ 102mmHg
pCO2
- Progesterone in pregnancy causes increased chemoreceptor sensitivity to CO2
- Minute ventilation increases 50%
- 25% increase in tidal volume
- 25% increase in respiratory rate
- Dead-space increases 45%
- However Vd/Vt unchanged
- CO2 production increases due to hypermetabolic state and foetal metabolism, however this is compensated by chemoreceptor sensitization
- therefore PACO2 decreases
- PACO2 approximates PaCO2 = approx 30mmHg → respiratory alkalosis
HCO3–
- Full metabolic compensation for chronic respiratory alkalosis occurs after 3 days according to the formula.
- This is due to decreased HCO3– reabsorption in the renal tubules
- In alkalosis, inhibition of renal secretion of hydrogen ions and ammonium
- glomerular bicarbonate filtration exceeds tubular acid secretion
- Excess bicarbonate is not converted to CO2 and H2O and reabsorbed → eliminated → Loss of base from system
Base Deficit
- reflects the renal loss of HCO3–
Sakurai 2016
Examiner Comments
2010A 11: 2 (20%) of candidates passed this question
For a good answer candidates were expected to describe the respiratory alkalosis and metabolic compensation associated with pregnancy. Candidates were expected to write a set of arterial blood gases showing a compensated respiratory alkalosis with a normal to slightly high P02. Values within +/- 5% of those expected, and found, in listed references would have scored candidates marks.
Candidates were then expected to mention that the PaO2 is high despite a 20% increase in oxygen consumption (relate that to increase in alveolar ventilation, decrease in PaCO2, and alveolar gas equation; PaCO2 is low due to tidal volume increase by 35%, Although anatomical dead space increases VD/VT in unchanged, despite CO2 production increased by increased basal metabolic rate; HCO3 decreases because of increased renal excretion of HCO3 due to inhibition of renal secretion of hydrogen ions and ammonium; base deficit reflects the renal loss of HCO3.
Some candidates described a low maternal P02, none commented on how the maternal P02 and PC02 enhance gas exchange to the foetus. While electrolyte values are often measured on arterial blood gas analysis they do not form part of an arterial blood gas and so comments on electrolytes gained no marks. The double Bohr and double Haldane effects were not required to answer this question. Once again, this question highlighted the importance of a structured approach to the answer, thus enhancing a candidates opportunity to cover all key areas and put their knowledge across.
Syllabus: O1, 2a References: Nunn’s Applied Respiratory Physiology, Lumb, 6th edition, Chp 14
2022A 06
Describe the cardiovascular changes seen throughout pregnancy.
2016A 07
Describe the cardiovascular changes of pregnancy including parturition.
2013B 19
Describe the cardiovascular changes during pregnancy.
2010B 04
Describe the cardiovascular changes that occur in pregnancy
CICMWrecks Answer
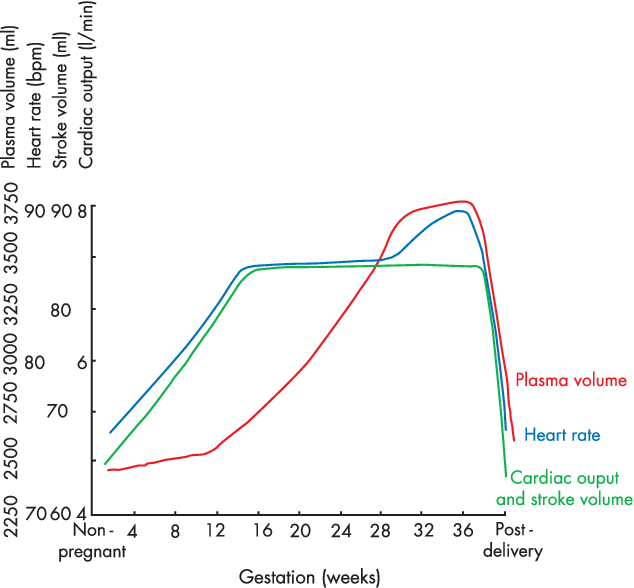
- Pregnancy is a time of increased metabolic demand, which cardiovascular changes reflect.
- Changes begin from week 8 and ↑ to plateau at 32 weeks → return to normal 2-8 weeks post delivery
- Changes depend on stage of pregnancy
- Hormonal changes: ↑ circulating concentrations of oestrogen, progesterone, hCG
- ↑ metabolic demand esp. during labour: ~↑60% O2 consumption/ CO2 production during labour
- Mechanical effects from gravid uterus
Characteristics
- Mechanical Effects:
- Thoracic changes:
- Anatomical compression of chest
- Diaphragm pushed upwards by 4cm
- ↑ AP + transverse diameter of chest wall (2-3cm)
- placental circulation: ↓pressure, ↓resistance AV shunt
- Aortocaval compression
- Collateral blood flow via collateral paravertebral epidural veins
- Thoracic changes:
- Hormonal Changes:
- ↑ circulating concentrations of oestrogen, progesterone, hCG
- Oestrogen stimulation of RAAS
- Increased plasma volume (40% or 1~1.5L positive)
- Erythropoietin secretion
- Increased erythropoiesis and red blood cell volume (20%)
Changes in CVS
- Anaemia of pregnancy
- Disproportionate plasma volume expansion relative to erythropoiesis
- Increased cardiac output (40%)
- Increased uterine blood flow (750ml/min)
- Increased renal blood flow
- Increased HR (25% by second trimester)
- Increased SV (25% in first trimester)
- Decreased peripheral vascular resistance (30%)
- Progesterone
- Prostaglandins
- Down-regulation of α receptors
- Decreased plasma oncotic pressure (15%) → peripheral oedema
During labour
- Contraction → 300ml return to central maternal circulation
- CO increases 15%, 30% and 45% in latent, active and expulsive phases of labour respectively
- Immediately after labour CO 80% pre-labour levels due to autotransfusion due to uterine involution
- Return to non-pregnant levels 2 weeks after delivery
Sakurai / Kerr / JC 2020
Examiner Comments
2022A 06: 51% of candidates passed this question.
It was expected that candidates would give a detailed description of the changes that occur throughout pregnancy, labour and post-delivery (a timeline). This should include but not be limited to, cardiac output, total peripheral resistance, blood flow distribution, uterine blood flow and blood volume changes. Better answers were able to relate these changes to the underlying mechanisms (such as progesterone induced vasodilatation etc). A detailed description of aortocaval compression and its importance was also required. Vague and imprecise statements attracted fewer marks (for example simply stating that heart rate increases without discussing the magnitude, time course and influences). This topic is well covered in some of the recommend texts.
2016A 07: 62% of candidates passed this question.
Significant CVS changes can occur by eight weeks and then progressively over the term of the pregnancy. Structured answers helped candidates avoid missing important areas of the answer. It was expected candidates could detail the major changes such as a 40 – 50% increase in blood volume, a 30 – 50% increase in cardiac output, a slight decrease in blood pressure, the heart size and position changes, the impact of aortocaval compression and alterations in colloid osmotic pressure. Some mention of the changes during labour and delivery was expected noting uterine contraction squeezes blood to maternal circulation (auto transfusion), cardiac output increases (immediately after delivery up by about 60 – 80%) and blood pressure increases (both systolic and diastolic) during labour.
Hormones, particularly the effects of foetoplacental production or transformation of hormones, and their cardiovascular effects, especially on total body composition / filling pressures were under explained. The cardiovascular changes at parturition were not well explained.
2013B 19: 4 candidates passed (14.8%).
Many candidates’ answers included respiratory and other systems (e.g. endocrine) when only cardiovascular changes were asked for. Candidates are reminded to read the questions carefully. Poor candidates lacked detail of the progressive changes through the trimesters. Changes during (and immediately post) labour and delivery were often overlooked. This is listed as a core topic within the syllabus, that is readily covered by most physiology texts and candidates are expected to have a very sound knowledge of it.
2010B 04: 4 (27%) of candidates passed this question.
A structured approach to answering this question was important. The principal topics to discuss included the increased cardiac output, increased blood volume, changes in red blood cell mass and protein concentrations, decrease in blood pressure and gravitational effects of the gravid uterus on major blood vessels. Answers benefited by specific details of percentage change and reference to timing of occurrence.
Syllabus: O1,2a
References: Hemmings Foundation of Anaesthesia: Basic and Clinical Science Pg 823 – 825, Miller Anaesthesia pgs2308-2309
2015B 08
Compare and contrast the physiological changes in the cardiovascular system in pregnancy at term and morbid obesity (BMI > 30).
CICMWrecks Answer
Pregnancy at Term
Morbid Obesity
- Pregnancy is a time of increased metabolic demand, which cardiovascular changes reflect.
- Changes begin from week 8 and ↑ to plateau at 32 weeks → return to normal 2-8 weeks post delivery
- excessive fat accumulation in adipose tissue
- WHO/NIH classification based on BMI:
- Overweight: BMI 25 – 30
- Obesity: BMI ≥ 30
- Obesity Class 1: 30 to 34.9 kg/m2
- Obesity Class 2: 35 to 39.9 kg/m2
- Obesity Class 3: BMI ≥40 kg/m2
- Alternate classifications:
- Severe Obesity: ≥ 35 or 40 kg/m2
- Morbidly Obese: BMI ≥ 40 (or) Obesity related disease and a BMI ≥ 35
- Super Obesity: ≥ 45 or 50 kg/m2
- Changes depend on stage of pregnancy
- Hormonal changes: ↑ circulating concentrations of oestrogen, progesterone, hCG
- ↑ metabolic demand esp. during labour: ~↑60% O2 consumption/ CO2 production during labour
- Mechanical effects from gravid uterus
- Changes depend on extent + duration of obesity
- Complex genetic and environmental causes
- Increased caloric intake
- Increased metabolic rate (normal for BSA)
- associated with HTN, HF, IHD, cardiomyopathy, sudden cardiac death, arrhythmias, PVD, DVT, CVD
- Thoracic changes:
- Anatomical compression of chest
- Diaphragm pushed upwards by 4cm
- ↑ AP + transverse diameter of chest wall (2-3cm)
- placental circulation: ↓pressure, ↓resistance AV shunt
- Aortocaval compression
- Collateral blood flow via collateral paravertebral epidural veins
- Compression of abdominal + leg vessels
- ↓ VR → supine hypotension + ↑ risk DVTs
- ↑ circulating concentrations of oestrogen, progesterone, hCG
- Oestrogen stimulation of RAAS
- Increased plasma volume (40% or 1~1.5L positive)
- Erythropoietin secretion
- Increased erythropoiesis and red blood cell volume (20%)
- ↑ SNS
- ↑ HR + ↑ SV
- ↑ RAAS → Na+ retention → ↑ blood vol → ↑ MAP (Systemic HTN)
- ↑ MAP → LVH → LV dilation → LV failure
- LV diastolic failure + ↑ PVR → RV hypertrophy
- ↑ Leptin → Cardiac remodelling + LVH
- Plasminogen Activator Inhibitor-1 → ↓ fibrinolysis → predisposes to VTE
- Inflammatory Adipokines → Impairs endothelial function → ↑ SVR
- insulin resistance + hyperlipidaemia → inflammatory mediator upregulation → disrupt endothelial function → IHD + cerebrovascular disease + PVD
- Anaemia of pregnancy
- Disproportionate plasma volume expansion relative to erythropoiesis
- Increased cardiac output (40%)
- Increased uterine blood flow (750ml/min)
- Increased renal blood flow
- Increased HR (25% by second trimester)
- Increased SV (25% in first trimester)
- Increased VO2 : Due to increased LBM and fat mass.
- Increased Cardiac Output: To maintain DO2.Initially with preserved ejection fraction
- Increased Stroke Volume: Due to:
- Increased preload (major factor)
- Increased contractility (minor factor) due to increased circulating adrenal hormones.
- Decreased peripheral vascular resistance (30%)
- Progesterone
- Prostaglandins
- Down-regulation of α receptors
- Decreased plasma oncotic pressure (15%) → peripheral oedema
- ↑ Peripheral vascular resistance
- Inflammatory Adipokines → Impairs endothelial function
- ↑ SNS
- Diastolic dysfunction: Due to myocardial fibrosis impairing relaxation.
- direct deposition of fat in myocardium → conduction disease (& predisposition to arrhythmias) + cardiomyopathy
- OSA
- Pulmonary HTN → cor pulmonale
- Polycythaemia → ↑ viscosity
Sakurai / Kerr / JC 2020
Examiner Comments
2015B 08: 2% of candidates passed this question.
The question was very specific for the cardiovascular system and therefore answers that
described respiratory changes and airway modulation failed to score marks. This answer leant
itself to a tabular format. Candidates are reminded to ensure they document the facts in the
correct column i.e. obesity facts in the obesity column. The cardiovascular changes associated
with term pregnancy are well described in various texts. Those associated with morbid obesity
required some integration from various sources and would include a structured series of
comments such as heart rate (unchanged), blood pressure (tendency for hypertension), stoke
volume (increased), cardiac output (increased), blood volume (increased – although perhaps
decreased on a ml/kg basis), systolic function (preserved or increased), LV wall thickness
increased. The pathological changes seen with the diseases associated with obesity are difficult
to tease out and better answers identified this. Morbid obesity has a specific definition and
stating this aided focus of the answers.
2020A 09
Outline the changes to drug pharmacokinetics and pharmacodynamics that occur at term in pregnancy.
2016B 16 – 2011A 11
Outline the influence of pregnancy upon drug pharmacokinetics
CICMWrecks Answer
Pharmacokinetics:
Absorption:
- ↓ Oral absorption
- ↑ N/V
- ↓ gastric emptying during labour
- ↓ gastric motility 2° to intestinal compression
- ↑ gastric absorption
- ↓intestinal absorption due to ↓ intestinal blood flow
- ↑ IM/SC/transdermal absorption
- ↑ skin blood flow
- ↑ C.O. (by 30-40%)
- ↓ SVR
- ↑ skin blood flow
- IV (↑ onset)
- Neuraxial
- ↓ epidural space 2° to EDVs
- ↓ spinal and epidural doses
- Inhalational
- Progesterone-mediated ↑ MV (by 50-70%)
- ↑ FA/FI ratio (= uptake
Distribution:
- ↑ VD (↑ TBW/ECF and fat)
- ↑ TBW/ECF (by 50%) (important for polar/ionized drugs)
- ↑ body fat % (important for lipid soluble drugs)
- ↓ plasma protein 2° to dilutional effect
- ↓ albumin →
- ↑ free % of acidic drugs (Eg. STP, propofol)
- ↓ dose required
- ↑ transplacental transfer of drug.
- ↓ A1AGP (by 30%) →
- ↑ free % of basic drugs (Eg. LA, β blockers)
- ↓ dose required
- ↑ transplacental transfer of drug
- ↓ albumin →
- Ionisation (mild ↑pH alters ionisation based on pKa)
- ↑ MV = mild respiratory alkalosis
- ↑ transplacental transfer of basic drugs as they will have ↑ % in unionized form
- (Base in base is less ionised)
- ↑ transplacental transfer of basic drugs as they will have ↑ % in unionized form
- ↑ ion trapping in more acidotic foetal circulation
- ↑ MV = mild respiratory alkalosis
Metabolism:
- Progesterone:oestrogen ratio
- Progesterone → induces hepatic enzymes
- Oestrogen → inhibits hepatic enzymes
- ↓ plasma cholinesterase (30%)
- Placenta metabolises some drugs
- Foetal liver has functioning CYP450
- Can metabolise drugs
- But requires transfer back to maternal circ for conjugation
Excretion:
- ↑ RBF/GFR (50%)
- ↑ clearance/↓ elimination t1⁄2 of water-soluble drugs
- ↑ MV/↓FRC
- ↑ washout of volatile agents
Pharmacodynamics:
- Decreased MAC – Increased sensitivity to volatile anaesthetics
- Increased LA sensitivity due to decreased α1-glycoprotein
- Increased sensitivity to IV anaesthetics
Gladwin / JC 2019
Examiner Comments
2020A 09: 7% of candidates passed this question.
Answers framed around absorption, distribution, metabolism and excretion performed better. Some brief comments on physiology are required as the basis for pharmacokinetic change, but discussion of physiology that was not then specifically related to pharmacology did not score marks. Specific ‘real life’ examples necessitating change in practice or prescribing were well regarded e.g. reduction in spinal/epidural local anaesthetic dosing. Vague statements about possible or theoretical changes were less well regarded.
2016B 16: 84% of candidates passed this question.
The best answers used tables and key pharmacological headings for comparisons, and avoided long sentences/ paragraphs.
An answer that correctly considered the following sections would be awarded a very good pass: Presentation, pharmacodynamics, mechanism of action, organ effects, side effects and pharmacokinetics.
Many candidates failed to identify agents as natural / synthetic catecholamines.
Few answers correctly mentioned the available preparations of these drugs or considered the structure activity relationships. Only 3 candidates commented that dobutamine is a racemic mixture.
Intracellular second messenger pathways were often incorrectly recounted or not mentioned at all. Pharmacodynamic effects on all organ systems, and all CVS parameters (HR, inotropy, PVR, SVR, SBP/DBP/MAP, regional circulations) should be considered. Metabolic fate and clinical dosage ranges were frequently incorrectly quoted.
2011A 11: 4 (33%) of candidates passed this question.
Answers framed around the structure of absorption, distribution, metabolism and excretion performed better. An approach based on the physiologic changes of pregnancy performed less well because important areas of pharmacokinetics were omitted. The effects of pregnancy on oral absorption should have included a discussion of gastrointestinal motility, nausea and vomiting and gut blood flow. Absorption from sites other than the gastrointestinal tract, such as skin, lung and the epidural space and the effect of pregnancy on these should have been mentioned. Many answers were vague on the effects of increases in total body water and plasma volume and cardiac output and changes in plasma protein binding on the distribution of drugs. Most answers did not provide enough specific examples. The effect of pregnancy hormones on liver enzyme activity were mentioned by few.
Syllabus: Generic Pharmacology III 2d
Recommended sources: Foundations of Anaesthesia: Basic clinical Science.
Hemmings and Hopkins, and Anaesthesia, Miller.
2024B 17
Describe the physiological changes that occur in the pregnant person during parturition (labour). (Changes that occur within the foetus are not required).
CICMWrecks Answer
First Stage of Labour
Onset of Regular Uterine Contractions to Full Cervical Dilation (10 cm)
Endocrine and Uterine Changes
- ↑ Oxytocin (posterior pituitary):
- Stimulates uterine contractions via calcium-mediated pathways
- Enhanced by Ferguson reflex (positive feedback from cervical stretch)
- ↑ Prostaglandins (PGE2, PGF2α):
- Promote cervical ripening by enzymatic degradation of collagen and increased water content
- Enhance myometrial contractility
- ↑ Estrogen:Progesterone ratio:
- Increases oxytocin receptor expression in myometrium
- Reduces uterine quiescence
- Relaxin softens the cervix and pelvic connective tissues
Uterine and Cervical Physiology
- Myometrial contractions begin in the fundus and progress caudally
- Frequency: ~2–3 per 10 min early, increasing to 4–5 per 10 min by late first stage
- Duration increases from 30–60 to 60–90 seconds
- Cervical effacement and dilation proceed:
- Effacement: cervix thins from ~3 cm to a thin membrane
- Dilation: progresses from 0 to 10 cm
Cardiovascular Changes
- Cardiac output increases by ~30–50% above baseline
- Stroke volume ↑ due to enhanced venous return between contractions
- HR increases by 15–20 bpm
- Autotransfusion: ~300–500 mL of blood is displaced from uterus into systemic circulation during each contraction
- Systolic BP may rise transiently during contractions
Respiratory Changes
- Oxygen consumption increases by ~40–60%
- Minute ventilation increases by ~50%, driven primarily by increased tidal volume
- Resultant respiratory alkalosis: PaCO₂ decreases to 28–32 mmHg, with a slight ↑ in pH (up to 7.48)
Metabolic Changes
- ↑ Glucose demand for uterine muscle contractions
- Beginning of lactate accumulation due to intermittent anaerobic metabolism during strong contractions
- Mild ↑ in catecholamines and cortisol stimulate gluconeogenesis and energy mobilisation
Gastrointestinal and Neurological
- ↓ Gastric motility and LOS tone → increased risk of nausea/vomiting
- Pain mediated via visceral afferents (T10–L1) from uterine and cervical stretch
- ↑ Endorphins modulate pain and provide some stress-buffering effects
Second Stage of Labour
Full Cervical Dilation to Delivery of the Neonate
Endocrine and Uterine Muscular Changes
- Stronger, more coordinated fundal-dominant uterine contractions
- Frequency: ~5 contractions per 10 minutes
- Peak intrauterine pressure: 100–120 mmHg
- Maternal voluntary effort via abdominal muscle contraction and Valsalva manoeuvre aids fetal descent
Neurohormonal and Pain Modulation
- Somatic pain (S2–S4) due to distension of lower birth canal, perineum, and pelvic floor
- Further ↑ in β-endorphins from hypothalamus and pituitary provide endogenous analgesia
- Sympathetic activation → ↑ catecholamines (adrenaline, noradrenaline)
- Excessive stress can inhibit contractions and uteroplacental blood flow
Cardiovascular Changes
- Cardiac output peaks at 80–100% above pre-labour baseline
- Increased systemic blood pressure and heart rate during maternal pushing
- Risk of aortocaval compression in supine position → reduced venous return and hypotension; left lateral positioning recommended
Respiratory Changes
- ↑ Oxygen consumption approximates levels seen in moderate-to-heavy exercise
- Reaches 2.0–2.5 mL/kg/min
- Hyperventilation continues; persistent hypocapnia may lead to lightheadedness, tingling
Metabolic and GI Changes
- High lactate production in uterine muscle → risk of maternal acidosis in prolonged labour
- Glucose depletion in long second stages contributes to maternal fatigue
- Vomiting more likely due to raised intra-abdominal pressure and gastric stasis
Third Stage of Labour
Delivery of the Placenta
Endocrine and Uterine Haemostasis
- Oxytocin surges post-delivery:
- Promotes strong myometrial contraction
- Facilitates placental separation
- Prostaglandins also contribute to sustained myometrial tone
- Contraction of spiral arteries and “physiological ligature effect” from muscle fibres reduces haemorrhage
- Active management (e.g. oxytocin IM) used prophylactically to prevent postpartum haemorrhage
Cardiovascular Adjustments
- Blood loss ~300–500 mL in vaginal delivery
- May exceed 500 mL in postpartum haemorrhage
- Cardiovascular system compensates via vasoconstriction, ↑ HR, and continued autotransfusion from contracting uterus
Respiratory and Metabolic
- Respiratory demand begins to decline as physical effort ceases
- Continued elevation in metabolic rate for tissue repair and recovery
- Restoration of acid–base balance after lactate clearance
Neurological and GI
- Emotional relief and oxytocin release facilitate bonding and lactation initiation
- Endorphin levels remain elevated immediately postpartum
- Risk of vomiting persists due to residual gastric stasis and ongoing hormonal effects
Examiner Comments
2024B 17: 39% of candidates passed this question.
This question required consideration of the alterations of the uterus, and the hormonal changes during labour, as well as discussion of the effects of this on the other body systems. Cardiovascular and respiratory changes held most of the mark weighting however gastrointestinal, metabolic and neuronal changes were also required.
A good answer was structured using the 3 stages of labour to explain the hormonal changes that initiate and maintain labour (oxytocin and positive feedback the primary but not the only factor described), changes to the cervix, uterine muscle and active muscular effort, delivery of neonate and placenta and uterine mechanisms to limit blood loss. Using this structure a description of cardiovascular and respiratory changes should follow with some detail about pain/endorphins, abdominal pressure/LOS sphincter and metabolic changes (lactate/glucose utilisation) also expected. The question was specific to parturition. Physiological changes throughout pregnancy were not required.
2024A 10
(a) Explain the excitation contraction mechanism as it relates to the smooth muscle of the myometrium including a gravid uterus (50% of marks).
(b) For each tocolytic agent: salbutamol, nifedipine, magnesium sulphate, provide the following information:
(i) List the class (10% of marks)
(ii) Provide a dose (10% of marks)
(iii) Describe the mechanism of action (20% of marks)
(iv) Outline the adverse effects (10% of marks)
CICMWrecks Answer: Smooth Muscle in Uterus
Excitation Contraction Coupling in SM
- Motor neuron depolarisation
- ACh vesicular release
- Multiple MEPs → End plate potential
- Muscle AP propagates via T-tubles
- Opens L-type Ca channels
- Influx of EC Ca → ↑ IC [Ca]
- Variable amount of Sarcoplamic reticula in SM
- Can have some ↑ IC [Ca] via Ca induced Ca release.
- Ca binds Calmodulin → Ca-Calmodulin complex
- Ca-Calmod → ↑ MLCK activity
- → Phosphorylation of Myosin Light Chain (MLC)
- → Activation of Myosin ATPase
- Cross-bridge cycling.
Cross Bridge Cycling
- “Flexed” Myosin without ATP binds to Actin.
- Binding of ATP to Myosin causes release of Actin/Myosin complex and extension of the head
- In the presence of Ca-Calmod complex
- Actin binding sites are open and binding of myosin/Actin/ATP complex is formed
- Hydrolysis of ATP to ADP + P in myosin head by Myosin ATPase
- → conformational change “initial flexing” the myosin head and releasing phosphate
- Release of ADP further flexes Myosin head
- In presence of Ca return to step 2.
Relaxation
- Ca removed from cell
- Ca ATPase
- Ca2+/Na+ antiport
- Myosin Light Chain Phosphatase
- dephosphorylates MLC → inhibition of myosin ATPase
Differences in Gravid Uterus
These physiological adaptations in the gravid uterus maintain quiescence throughout most of pregnancy, ensuring fetal development, while preparing it to transition into a highly excitable and contractile state essential for effective labor.
| Feature | Gravid Uterus | Other Smooth Muscle |
|---|---|---|
| Resting Membrane Potential | Less negative near term, increasing excitability | Stable, less variation in response to hormones |
| Hormonal Regulation | Progesterone dominance (quiescence early), estrogen dominance (contractility late) | Task-specific, less pronounced |
| Gap Junctions | Increased (connexin-43) near term for synchronized contractions | Sparse, localized contraction |
| Calcium Handling | Increased L-type calcium channel activity and intracellular calcium recruitment near term | Stable calcium influx and release mechanisms |
| Oxytocin Sensitivity | High near term, upregulated oxytocin receptor density | Minimal, plays minor or no role |
| Relaxation Mechanisms | Progesterone/NO-mediated quiescence during pregnancy, reduced near term | Nitric oxide, prostaglandins, or sympathetic input |
| Action Potentials | Long, frequent, propagating bursts near term | Short, localized |
| Structural Adaptations | Hypertrophy and hyperplasia of myocytes | Minimal structural changes |
| Functional Synchrony | Whole-organ synchronization with gap junctions, pacemaker cells, and oxytocin | Localized function, no whole-organ synchronization |
Gladwin / JC 2024
CICMWrecks Answer: Tocolytic Agents (Limited)
Examiner Comments
2024A 10: 42% of candidates passed this question.
(a) This question required an explanation of the process of contraction in smooth muscle, as well as specific information pertaining to the smooth muscle of the uterus. Specific information included: stimuli for contraction (i.e., hormones such as oxytocin, oestrogen, and prostaglandins and stretch); possessing an unstable membrane potential which plays a greater role than nervous input; as well as the uterus smooth muscle functioning as a syncytia and having baseline tone.
The key steps of contraction (influx of calcium, formation of calcium-calmodulin formation, activation of MLCK, creation of myosin-actin cross bridges with utilisation of ATP) are those generic to any smooth muscle and marks were awarded accordingly. Descriptions of striated muscle did not attract marks. A description or explanation was required rather than a list of steps (e.g., the sources of calcium rather than a simple statement of calcium influx occurring).
(b) Use of these drugs as tocolytics is acknowledged as a less common reason for their utilisation – the fractionation of this question was to breakdown into more achievable parcels of information. This allowed candidates to score more marks for relating the mechanism of action specifically to the uterus. Higher marks in this section were awarded for specific unwanted effects relevant to use as a tocolytic e.g., foetal tachycardia for salbutamol as result of crossing the placenta. Marks were awarded to doses for these drugs when used as a tocolytic, as opposed to for other indications (i.e., salbutamol infusion rather than nebulised).
ii. Outline the functions of the placenta and the determinants of placental blood flow.
2021B 06 – 2018A 09
Describe the functions of the placenta (80% of marks).
Outline the determinants of placental blood flow (20% of marks).
CICMWrecks Answer
Functions of the Placenta
- Organ of foetal + maternal origin; supports developing foetus
- Low pressure, low resistance AV shunt that provides metabolic nutrients necessary for growing foetus
- Functions
- Transfer: gas exchange; nutrient + waste exchange; drugs; heat
- Immunological barrier
- Metabolic
- Endocrine
1. Transfer
a. Gas Exchange
- Diffusion dependent on Fick’s Principle
- Maternal placental flow ~600ml/min at term (2x foetal flow) → ↑diffusion by ↑concentration gradient for solutes
- Molecules <600Da more readily diffuse down concentration gradient
- O2 diffusion
- PO2 entering placenta via uterine artery = 18mmHg (SpO2 45%)
- PO2 leaving placenta via uterine vein 28mmHg (SpO2 70%)
- Foetus able to absorb large enough vol O2 despite low PO2 because:
- Foetal Hb
- 2 y subunits cf β → prevent binding of 2,3-DPG → L shifted OHDC → favours O2 loading at ↓PaO2
- [FHb] 50% > maternal [Hb]
- Double Bohr effect
- Describes Bohr effects happening on either side of placental gas exchange in mother + foetal circulations
- Accounts for 2-8% of O2 transfer
- Bohr effect 1: placenta: foetus unloads CO2 in placenta → ↑placental CO2 → RIGHT shift HbA OHDC → ↓HbA affinity for O2 → ↑placental O2 unloading
- Bohr effect 2: foetus: foetus unloads CO2 → ↓foetal CO2 → LEFT shift HbF OHDC → ↑HbF affinity for O2 → ↑foetal O2 binding/ uptake
- Foetal Hb
- CO2 diffusion
- Foetal PaCO2 50mmHg; intervillous PCO2 37mmHg
- CO2 offloading favoured in foetus by:
- High foetal [Hb] ↑s amount of CO2 that can be carried as carbaminoHb
- Double Haldane effect
- Haldane effect: describes how ∆O2 sat of Hb affect CO2 transport: deoxyHb has ↑affinity for CO2 than oxyHb
- Double Haldane: describes Haldane effects happening across the placenta
- Accounts for 45% of CO2 transfer between maternal and foetal circulation
- Haldane 1: placenta: placenta unloads O2 → ↓placental O2 → deoxyHbA has ↑affinity of CO2 → ↑placental CO2 uptake from foetus
- Haldane 2: foetus: foetus takes up O2 → ↑HbF O2 → ↓HbF affinity for CO2 → ↑HbF CO2 release to placenta
b. Nutrient delivery
- Nutrient diffusion
- High foetal caloric requirements in late pregnancy
- Facilitated diffusion of glucose via carrier molecules in trophoblasts
- Active transport for amino acids, Ca2+, Fe, folate, vit A and C
c. Waste removal – Urea, Uric acid, Creatinine, Br
d. Heat transfer
2. Immunological function
- permeable to IgG via pinocytosis → allows maternal abs to provide passive immunity to foetus
- Trophoblast cells lose many cell surface MHC molecules → making them less immunogenic; also cells cover themselves in mucoprotein which
disguises them from maternal immunie system - Chorionic cells act as immunological barrier – preventing maternal T cells and abs from reaching foetal circulation
- Some bacteria (listeria) and viruses (rubella, parvovirus B19, HIV) can cross into foetal circulation
- Progesterone + alpha-foetoprotein produced by yolk sac act as maternal immunosuppressive agents
3. Metabolic
- synthesis of glycogen, cholesterol, FA, enzymes
4. Endocrine function
- synthesis of 4 main hormones:
- bHCG
- hPL: human placental lactogen (human chorionic somatomammotrophin)
- Oestriol
- Progesterone
- Synthesis of other hormones and growth factors
- Placental corticotrophin
- Human chorionic somatostatin
- Human chorionic thyrotropin
- Epidermal growth factor
- Somatomedin
Placenta
- Placenta:
- temporary fetal organ that begins developing from the blastocyst shortly after implantation
- ~22cm length, 2.5cm thickness. ~500gm
- Connects to fetus by umbillical cord
- “Chorionic villus” is the basic structural unit of the placenta → it is a vascular projection of foetal tissue that is bathed by maternal blood within the “Intervillous space”. It consists of:
- Foetal connective tissue containing foetal capillaries
- Chorion → outermost layer of foetal tissue that is made of 2 layers →
- (a) Syncytiotrophoblast (directly contacts maternal blood in intervillous space) and
- (b) Cytotrophoblast (b/t syncytiotrophoblasts and foetal CT)
Placental Circulation
- Placental circulation = Two circulation systems in parallel – maternal and the fetal
- Maternal circulation system
- Uterine Arteries (600ml/min, 100mm Hg) → arcuate arteries → radial arteries → spiral arteries (70 mm Hg) & basal arteries (myometrium and deciduas)
- Spiral arteries → intervillous spaces (10mm Hg) → uterine veins that are arranged in the periphery of the intervillous space.
- Blood in the intervillous space is exchanged 2-3 times per minute.
- Fetal circulation system:
- Two villus Umbilical Arteries (50mmHg) → finer vessels that cross through the chorionic plate → villus capillaries (30mmHg) → leaves placenta through umbillical vein (20mmHg)
- Their supply amounts to approximately 40% of the fetal heart blood volume per minute.
- The pressure in the fetal vessels and their villus branches always lies over that of the intervillous space. This protects the fetal vessels from collapse.
- Substances traverse between foetal and maternal blood via the following layers:
- Maternal blood (intervillous space) ↔ Chorion (2x layers of trophoblasts) ↔ Foetal connective tissue ↔ Endothelium of foetal capillaries ↔ Foetal blood
Determinants of Placental Blood Flow
Uteroplacental blood flow
- At term → uteroplacental BF is 500-700 mL/min (10% maternal C.O.) of which:
- 70-90% of this BF enters the intervillous space (via the spiral arteries) → NOT autoregulated as blood flow is “pressure-dependent” (see factors below)
- 10-30% of this BF supplies the myometrium/deciduas (via the basal arteries) → autoregulated blood flow
- Blood flow to the intervillous space (which participates in substance exchange with foetal blood) is affected by the following factors:
- Uterine arterial pressure (UAP):
- Maternal arterial BP → ↓ MABP (Ie. due to SNS block 2° neuraxial block,
hypovolaemia, supine hypotension syndrome, Etc.) causes ↓ UAP → ↓ UBF
- Maternal arterial BP → ↓ MABP (Ie. due to SNS block 2° neuraxial block,
- Uterine venous pressure (UVP):
- Uterine tone and contractions → ↑ tone/contractions (Ie. due to contractions,
oxytoxics, ketamine, Etc.) causes ↑ UVP → ↓UBF
- Uterine tone and contractions → ↑ tone/contractions (Ie. due to contractions,
- Uterine vascular resistance (UVR):
- Uterine arteriolar tone → ↑ vasoconstriction (Ie. a/w essential HT and PET, α-adrenoceptor stimulation (by endogenous SNS innervation, catecholamines or sympathomimetics), and vasopressin) causes ↑ UVR → ↓ UBF
Umbilical blood flow
- At term → umbilical BF is 360 mL/min (25-50% of foetal C.O. (≈ 1000 mL/min))
- It is “autoregulated” (cf. uterine BF) → involves vasodilators (PCI-2/NO) derived from vascular endothelium
- BF is ↓ with severe hypoxia, ↑ BGL, catecholamine and cord compression
Kerr / Bianca 2020
Examiner Comments
2021B 06: 49% of candidates passed this question.
There was a wide range of marks for this question with a few candidates scoring excellent marks. Those answers that scored well provided a comprehensive list of functions as well as an explanation as to the what, how and/or why of these functions. Poorer answers omitted some of the functions or failed to elaborate on them by providing only a limited list. The second component of the question was generally well outlined, most candidates provided some estimate of normal values at term and a simple elaboration regarding the factors that affect placental blood flow.
2018A 09: 32% of candidates passed this question.
Many candidates provided a broad overview of functions of the placenta but lacked detail.
Placental blood flow has maternal and foetal components, though most only considered the maternal circulation to the placenta and didn’t mention the foetal vessels. Many were not specific as to what blood vessels were described.
Many stated that uterine blood flow is not autoregulated, however went on to describe myogenic and neuro-humoral mechanisms of autoregulation
iii. Describe the transfer of nutrients, drugs and gases between mother and foetus including the double Bohr and Haldane effects.
2009A 24
Explain the factors which influence the transfer of drugs across the placenta to the foetus.
2008A 22
Outline the factors influencing the transport of drugs across the placenta.
CICMWrecks Answer
Physiological factors
- Drug transfer via diffusion, facilitated diffusion, secondary active transport, pinocytosis (e.g. immunoglobulins)/
- Diffusion according to Fick’s Law (see eqn):
where- MW = Molecular weight
- Drugs <500da freely permeable
- Δ[Drug] = Concentration gradient between maternal anf foetal blood
- SA = Surface area for diffusion
- 16m2 compared to alveolar surface area of 60m2
- h = thickness of diffusion membrane
- 3.5 microns compared with 0.5 for alveolar diffusion membrane
- MW = Molecular weight
- Drug delivery to uterus
- Blood flow ~750ml/min (Aprrox 600ml/min to placenta)
- No autoregulatory mechanisms
- Placental transporters
- MDR1 and p-glycoprotein efflux drugs out of foetal circulation
- Placental metabolism
- P450 reactions
- Pentobarbitol metabolized by placenta
- P450 reactions
Drug factors
- Drug size
- Heparin too large to permeate (Warfarin can)
- Lipophilicity
- Highly lipophilic drugs more permeable (Fentanyl > morphine)
- Ionization
- Charged molecules less permeable (Glycopyrrolate < atropine)
- Ionization trapping
- Alfentanyl (pKa 6.5) ~90% unionized at physiological pH → more permeable
- As alfentanyl crosses into foetal circulation, becomes more ionized in lower pH → trapped in foetal circulation
- Protein binding
- Reduces permeability
Disease factors
- Inflammation of placental barrier increases permeability of drugs
Sakurai 2016
Examiner Comments
2009A 24: Pass rate: 30%
Good answers showed an understanding of diffusion, the influence on transfer of lipid solubility, molecular size, degree of ionisation and protein binding. They also made reference to placental transporters and placental metabolism. Extra points were scored for mentioning that the real concern is teratogenicity to the foetus.
Syllabus O2 2d
Reference: Katzung 10th edition p 971-973.
2008A 22: No candidates (0%) passed this question.
The main points candidates were expected to know included the passive and active mechanisms that regulate the transfer of drugs across placenta and the potential clinical implications of drugs use in pregnancy in order to pass this question.
Good answers to this question included examples to all the possible mechanisms that can affect the transport of drugs across placenta.
The common omissions were degree of ionisation, active transporters, placental metabolism, explanation on the interaction between protein binding and ionisation of a drug in regulating placenta transfer, and the expected molecular size or weight of a drug that affects passive placental transfer of the drug.
2009B 24
Describe how gas exchange is influenced across the placenta near the term of pregnancy.
2008B 22
Describe how gas exchange is facilitated across the placenta near the end of pregnancy.
CICMWrecks Answer
Diffusion via Fick’s Law
- Flow of gas (Rate of movement of solute) across semi-permiable membrane J is
where
C = concentration (or partial pressure for gasses)
A = cross-sectional area
T = thickness of the membrane or distance over which diffusion takes place.
- These factors alter the rate of transfer as per the equation above.
- Valid for Most medium – small substances
- Water soluble (H2O, electrolytes, glucose, urea) via intercelular clefts
- Lipid soluble substances (O2, CO2) via endothelial cells themselves.
- Flow = 1.2ml of O2 mmHg-1minute-1 across entire placenta
- Surface area of placenta for diffusion = 16m2
- Thickness of placental membrane falls as pregnancy progresses
- Minimum thickness is 3.5 micrometres
Oxygen
- Mean partial pressure of oxygen (PO2) in maternal blood is considerably higher than in fetal blood
- As a consequence, oxygen readily diffuses across the placenta from maternal to fetal blood
- Despite its low PO2, fetal blood is able to transport essentially the same quantity of oxygen to tissues as maternal blood
| O2 Partial Pressure | Oxygen Content | |
|---|---|---|
| Maternal | PaO2 = 100mmHg (80-110) | CaO2 = 16.1ml/100ml |
| Fetal Umbilical Vein | PvO2 = 30mmHg (30-50) | CvO2 = 16ml/100ml |
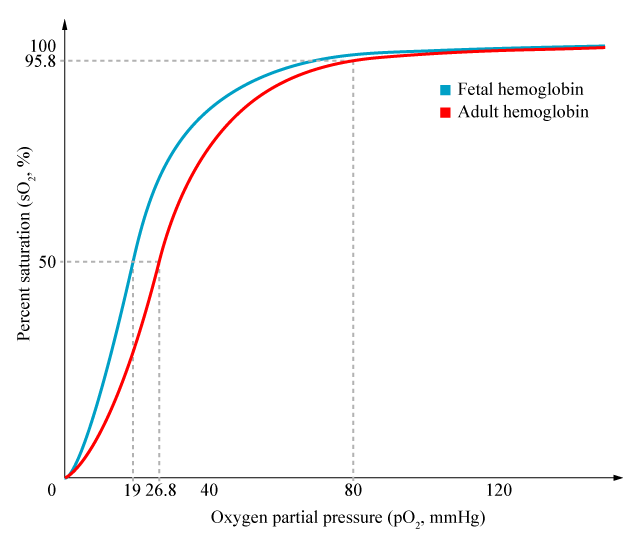
- Foetal Hb has a higher affinity for O2 than maternal Hb
- oxygen carrying capacity is improved, despite lower PaO2
- P50 is 20mmHg vs 26 in maternal
- Haemoglobin concentration in blood is higher in the foetus, increasing oxygen carriage
- 120g/L in mother
- 170g/L in foetus
- Double Bohr effect:
- Movement of CO2 from the foetal to the maternal circulation results in a simultaneous rise in maternal CO2 and fall in foetal CO2
- Rise in foetal Hb oxygen affinity, fall in maternal Hb oxygen affinity by the Bohr effect
Carbon dioxide
- Carbon dioxide is produced abundantly in the fetus
- PCO2 of fetal blood is higher than maternal blood
- Carbon dioxide therefore diffuses from fetal blood, through the placenta, into the maternal circulation, and is disposed of by expiration from the mother’s lungs.
| O2 Partial Pressure | |
|---|---|
| Maternal | PaCO2 = 32mmHg |
| Fetal Umbilical Artery | PvCO2 = 55mmHg |
- Hyperventilation in pregnancy (increased sensitivity of chemoreceptors to CO2) → Lower PaCO2
- Smaller gradient than oxygen, but oxygen has 20 times higher solubility
- Double Haldane effect:
- Simultaneous rise in foetal Oxy-Hb and fall of maternal Oxy-Hb
- Increased CO2 carrying capacity of maternal Hb, decreased in foetal Hb
Mooney / JC 2020
Examiner Comments
2009B 24: (11%) of candidates passed this question.
For a good answer candidates were expected to account how the placenta allows for effective diffusion to occur. Good answers incorporated the parameters within the Fick equation (eg. area of placental gas exchange, pressure of gas in maternal sinuses (PO2 = 50 mmHg), pressure of gas in umbilical vein (PO2 = 30 mmHg ). Also expected was an explanation of the role of foetal haemoglobin, the double Bohr and double Haldane effects. These were commonly omitted.
2008B 22: 3 (60%) candidates passed this question
Candidates were expected to cover the basic principles of gaseous diffusion across the placenta, with reference to: Both oxygen and carbon dioxide; Fick’s Law, including placental area and thickness, and relative gas tensions and solubilities; Changes in maternal and foetal blood flow approaching term; Approximate values for maternal and foetal gas tensions and content; The differences between foetal and maternal haemoglobin, quantitative and qualitative; The double-Bohr and double-Haldane effects; Relative maternal hyperventilation and it’s effects on arterial gas tensions and how these influence foetal transfer.
A good answer would also include a description of the physical arrangement of maternal sinuses and foetal capillaries; labelled dissociation curves for O2 and CO2 detailing the differences between maternal and foetal Hb; a placental gas exchange diagram, showing foetal and maternal arterial and venous gas tensions and content values.
Syllabus ref: O1 2d
Suggested Reading: Review of Medical Physiology / W F Ganong – 22nd ed Chapter 32.
Nunn’s Applied Respiratory Physiology / A B Lumb & J F Lunn – 6th ed
iv. Describe the transition from foetal to neonatal circulation and the establishment of ventilation.
2015A 02
Describe the Foetal Circulation and the changes that occur at birth
CICMWrecks Answer
Foetal Circulation
- Placenta
- Supplied by paired umbilical artery and drains to single umbilical vein
- Capillary networks in parallel à high flow, low resistance system, decreases overall systemic vascular resistance.
- Oxygenated blood (SpO2 80% PO2 35mmHg) from placenta returns to foetus via umbilical vein
- 60% of blood from umbilical vein bypasses liver via ductus venosus into IVC
- Blood in IVC from systemic circulation is hypoxaemic (SpO2 30%)
- Heart
- Blood from IVC enters right atrium and oxygenated blood, directed via the Eustachian valve, preferentially flows across foramen ovale to left ventricle à supplies ascending aorta (SpO2 65%, PaO2 25mmHg)
- This allows most oxygenated blood to supply the brain and coronary arteries
- Blood from SVC enters right atrium and continues to right ventricle and pulmonary arteries → flows into aorta via ductus arteriosus and predominantly supplies descending aorta (SpO2 60%, PaO2 20mmHg) and organs
- Blood from IVC enters right atrium and oxygenated blood, directed via the Eustachian valve, preferentially flows across foramen ovale to left ventricle à supplies ascending aorta (SpO2 65%, PaO2 25mmHg)
- Lungs
- High pulmonary vascular resistance due to;
- Unexpanded lungs
- Hypoxic pulmonary vasoconstriction
- Therefore blood in pulmonary artery preferentially perfuses systemic circulation via ductus arteriosus
- Only approx 12% of pulmonary arterial blood enters the pulmonary circulation
- High pulmonary vascular resistance due to;
Changes at birth
- Placenta
- Vasoconstriction occurs due to longitudinal stretch of umbelical vessels and increase in PaO2
- Augemented by clamping of vessels
- Loss of placenta increases systemic vascular resistance
- Increased left heart pressures
- Lungs
- After first breath…
- Hypoxic pulmonary vasoconstriction is relieved,
- Lung expands
- Recruitment of collapsed parallel capillary networks
- Dilation of existing vasculature
- Pulmonary blood flow increases 10-fold and pulmonary vascular resistance decreases
- Combined with decreased venous return (from placenta), decreases right heart pressures
- After first breath…
- Heart
- Foramen ovale
- Equilibration of right and left heart pressures closes flap of foramen ovale (occurs within minutes to hours)
- Pulmonary arterial blood flow further increases
- Ductus arteriosus
- The ductus arteriosus shunt become bi-directional
- Closure
- Due vasospasm caused by increased PO2
- Also, loss of PGE2 produced by placenta causes loss of vasodilation
- Occurs within 96 hours
- Foramen ovale
Sakurai 2016
Examiner Comments
2015A 02: 55 % of candidates passed this question.
This topic is well covered in standard texts and has been asked previously. Better answers displayed knowledge of the key concepts, such as the parallel circulations in the foetus and preferential flow of better oxygenated blood to the brain and upper limbs. Some candidates spent time on the maternal and placental circulations which were not required to answer the question asked.
v. Describe the physiological consequences of changes in posture during pregnancy including the consequences of aorto-caval compression.
V2: Obstetric Pharmacology
i. Describe the pharmacology of oxytocic drugs.
2013A 24
Describe the mechanism of action, and side effects of THREE (3) classes of drugs that are used to increase uterine tone and THREE (3) classes of drugs used to decrease uterine tone.
CICMWrecks Answer
Oxytotic
(used to augment labour and ↑ uterine tone)
- Oxytocin derivatives (syntocinon, carbitocin)
- Oxytocin synthesised in hypothalamus
- Gq-PCR on SM cells
- causing increased Ca influx
- Ca induced Ca relase from SR → SM contraction
- Cause milk ejection from mamary glands, hypotension (via relaxation of SM), arrhythmias, water retention (similar structure to ADH)
- Ergot derivatives (ergometrine)
- Acts on alpha 1 and 5HT2 recepters (both Gq-PCRs) on uterine and vascular SM cells
- ↑ force and freq of contractions
- ↑ uterine tone
- contraction of cervix.
- Prostaglandins
- PGF2 alpha (Gq-PCR)
- Intra myometrial injection
- causes ↑ SM tone
- Bronchospasm if injected intravenously.
Tocolytic
(↓ uterine tone to suppress pre-term labour)
- Beta 2 agonists (salbutamol)
- β2 receptors action → ↑AC → ↑ cAMP → ↑PLC → ↓calcium → relaxation of myometrial SMCs
- Tachycardia/tremour/hypokalaemia
- Ca-channel blockers (nifedipine)
- ↓d Ca influx due to action on l-type Ca channels → ↓ uterine tone
- Inhibition of hypoxic pulmonary vasoconstriction, Impaired platlet aggregation, Headache, flushing and dizziness, Peripheral oedema
- NSAIDs (indomethacin)
- ↓ formation of PGE2 and PGF2α → ↓ uterine tone
- Can cause premature closure of ductus arteriosus, oligohydramnios, NEC and broncho-pulmonary dysplasia
Gladwin 2016
Click here for CICMWrecks Pharmacopeia Table for Oxytocics and Tocolytics
Examiner Comments
2013A 24:
Candidates often appeared to have a sufficient awareness of the choice of drugs (e.g. oxytocin analogues, ergot alkaloids, beta-receptor agonists, calcium channel blockers, etc.), but then failed to produce sufficient depth of knowledge to adequately describe their mechanisms of action in respect to uterine tone. Candidates are reminded that if asked to mention side effects, mentioning side effects of greatest relevance to intensive care (e.g. bronchospasm) in addition to the more generic side effects (e.g. rash).
ii. Describe the pharmacology of tocolytic drugs.
2013A 24
Describe the mechanism of action, and side effects of THREE (3) classes of drugs that are used to increase uterine tone and THREE (3) classes of drugs used to decrease uterine tone.
CICMWrecks Answer
Oxytotic
(used to augment labour and ↑ uterine tone)
- Oxytocin derivatives (syntocinon, carbitocin)
- Oxytocin synthesised in hypothalamus
- Gq-PCR on SM cells
- causing increased Ca influx
- Ca induced Ca relase from SR → SM contraction
- Cause milk ejection from mamary glands, hypotension (via relaxation of SM), arrhythmias, water retention (similar structure to ADH)
- Ergot derivatives (ergometrine)
- Acts on alpha 1 and 5HT2 recepters (both Gq-PCRs) on uterine and vascular SM cells
- ↑ force and freq of contractions
- ↑ uterine tone
- contraction of cervix.
- Prostaglandins
- PGF2 alpha (Gq-PCR)
- Intra myometrial injection
- causes ↑ SM tone
- Bronchospasm if injected intravenously.
Tocolytic
(↓ uterine tone to suppress pre-term labour)
- Beta 2 agonists (salbutamol)
- β2 receptors action → ↑AC → ↑ cAMP → ↑PLC → ↓calcium → relaxation of myometrial SMCs
- Tachycardia/tremour/hypokalaemia
- Ca-channel blockers (nifedipine)
- ↓d Ca influx due to action on l-type Ca channels → ↓ uterine tone
- Inhibition of hypoxic pulmonary vasoconstriction, Impaired platlet aggregation, Headache, flushing and dizziness, Peripheral oedema
- NSAIDs (indomethacin)
- ↓ formation of PGE2 and PGF2α → ↓ uterine tone
- Can cause premature closure of ductus arteriosus, oligohydramnios, NEC and broncho-pulmonary dysplasia
Gladwin 2016
Click here for CICMWrecks Pharmacopeia Table for Oxytocics and Tocolytics
Examiner Comments
2013A 24:
Candidates often appeared to have a sufficient awareness of the choice of drugs (e.g. oxytocin analogues, ergot alkaloids, beta-receptor agonists, calcium channel blockers, etc.), but then failed to produce sufficient depth of knowledge to adequately describe their mechanisms of action in respect to uterine tone. Candidates are reminded that if asked to mention side effects, mentioning side effects of greatest relevance to intensive care (e.g. bronchospasm) in addition to the more generic side effects (e.g. rash).
2024A 10
(a) Explain the excitation contraction mechanism as it relates to the smooth muscle of the myometrium including a gravid uterus (50% of marks).
(b) For each tocolytic agent: salbutamol, nifedipine, magnesium sulphate, provide the following information:
(i) List the class (10% of marks)
(ii) Provide a dose (10% of marks)
(iii) Describe the mechanism of action (20% of marks)
(iv) Outline the adverse effects (10% of marks)
CICMWrecks Answer: Smooth Muscle in Uterus
Excitation Contraction Coupling in SM
- Motor neuron depolarisation
- ACh vesicular release
- Multiple MEPs → End plate potential
- Muscle AP propagates via T-tubles
- Opens L-type Ca channels
- Influx of EC Ca → ↑ IC [Ca]
- Variable amount of Sarcoplamic reticula in SM
- Can have some ↑ IC [Ca] via Ca induced Ca release.
- Ca binds Calmodulin → Ca-Calmodulin complex
- Ca-Calmod → ↑ MLCK activity
- → Phosphorylation of Myosin Light Chain (MLC)
- → Activation of Myosin ATPase
- Cross-bridge cycling.
Cross Bridge Cycling
- “Flexed” Myosin without ATP binds to Actin.
- Binding of ATP to Myosin causes release of Actin/Myosin complex and extension of the head
- In the presence of Ca-Calmod complex
- Actin binding sites are open and binding of myosin/Actin/ATP complex is formed
- Hydrolysis of ATP to ADP + P in myosin head by Myosin ATPase
- → conformational change “initial flexing” the myosin head and releasing phosphate
- Release of ADP further flexes Myosin head
- In presence of Ca return to step 2.
Relaxation
- Ca removed from cell
- Ca ATPase
- Ca2+/Na+ antiport
- Myosin Light Chain Phosphatase
- dephosphorylates MLC → inhibition of myosin ATPase
Differences in Gravid Uterus
These physiological adaptations in the gravid uterus maintain quiescence throughout most of pregnancy, ensuring fetal development, while preparing it to transition into a highly excitable and contractile state essential for effective labor.
| Feature | Gravid Uterus | Other Smooth Muscle |
|---|---|---|
| Resting Membrane Potential | Less negative near term, increasing excitability | Stable, less variation in response to hormones |
| Hormonal Regulation | Progesterone dominance (quiescence early), estrogen dominance (contractility late) | Task-specific, less pronounced |
| Gap Junctions | Increased (connexin-43) near term for synchronized contractions | Sparse, localized contraction |
| Calcium Handling | Increased L-type calcium channel activity and intracellular calcium recruitment near term | Stable calcium influx and release mechanisms |
| Oxytocin Sensitivity | High near term, upregulated oxytocin receptor density | Minimal, plays minor or no role |
| Relaxation Mechanisms | Progesterone/NO-mediated quiescence during pregnancy, reduced near term | Nitric oxide, prostaglandins, or sympathetic input |
| Action Potentials | Long, frequent, propagating bursts near term | Short, localized |
| Structural Adaptations | Hypertrophy and hyperplasia of myocytes | Minimal structural changes |
| Functional Synchrony | Whole-organ synchronization with gap junctions, pacemaker cells, and oxytocin | Localized function, no whole-organ synchronization |
Gladwin / JC 2024
CICMWrecks Answer: Tocolytic Agents (Limited)
Examiner Comments
2024A 10: 42% of candidates passed this question.
(a) This question required an explanation of the process of contraction in smooth muscle, as well as specific information pertaining to the smooth muscle of the uterus. Specific information included: stimuli for contraction (i.e., hormones such as oxytocin, oestrogen, and prostaglandins and stretch); possessing an unstable membrane potential which plays a greater role than nervous input; as well as the uterus smooth muscle functioning as a syncytia and having baseline tone.
The key steps of contraction (influx of calcium, formation of calcium-calmodulin formation, activation of MLCK, creation of myosin-actin cross bridges with utilisation of ATP) are those generic to any smooth muscle and marks were awarded accordingly. Descriptions of striated muscle did not attract marks. A description or explanation was required rather than a list of steps (e.g., the sources of calcium rather than a simple statement of calcium influx occurring).
(b) Use of these drugs as tocolytics is acknowledged as a less common reason for their utilisation – the fractionation of this question was to breakdown into more achievable parcels of information. This allowed candidates to score more marks for relating the mechanism of action specifically to the uterus. Higher marks in this section were awarded for specific unwanted effects relevant to use as a tocolytic e.g., foetal tachycardia for salbutamol as result of crossing the placenta. Marks were awarded to doses for these drugs when used as a tocolytic, as opposed to for other indications (i.e., salbutamol infusion rather than nebulised).
VIVAs
| 2023B | Factors that determine rate of gas transfer across placenta |
| 2023A | |
| 2022B | Identify curves which belong to major vessels involved in placental gas transfer |
| 2022A | |
| 2021B | |
| 2021A | Maternofoetal physiology. Normal ABG at term. Explain changes. ABG: pH 7.45 pO2 105 pCO2 30 HCO3 20 BE -2 |
| 2020B | Uterine blood flow at term, percentage to placenta |
| 2019B | |
| 2019A | Functions of placenta |
| 2018B | Maternal oxygenation, normal ABG values for 38 wk pregnant |
| 2018A | |
| 2017B | |
| 2017A | |
| 2016B | |
| 2016A | |
| 2015B | |
| 2015A | |
| 2014B | Obstetric and neonatal physiology – CV changes, gas exchange across placenta, changes with first breath, humidity |
| 2014A | |
| 2013B | |
| 2013A | |
| 2012B | ABG for pregnant woman at term. Resp changes, drug transfer across placenta, syntocine, ergotamine |
| 2012A | |
| 2011B | Respiratory changes in pregnancy at term, ABG, foetal circulation, changes at birth |
| 2011A | |
| 2010B | |
| 2010A | |
| 2009B | |
| 2009A | |
| 2008B | |
| 2008A | |
| 2007B |

Recent Comments