Syllabus (Fourth Edition, 2023)
Topics
S1: Physiology of Immunology and Host Defence
i. Explain the immunological basis of hypersensitivity including anaphylaxis.
ii. Describe the factors involved in the process of inflammation and the immune response, including innate and acquired immunity.
iii. Outline the non-immune host defences used to defend against infection.
S2: Pharmacology Related to Immunology
i. Understand the pharmacology of Human Immunoglobulin.
Topics not covered in previous SAQs
S1: Physiology of Immunology and Host Defence
iii. Outline the non-immune host defences used to defend against infection.
S2: Pharmacology Related to Immunology
i. Understand the pharmacology of Human Immunoglobulin.
Learning Objectives for the First Part Examination in Intensive Care Medicine
- This will ensure that trainees, tutors, and examiners can work from a common base.
- All examination questions are based around this Syllabus.
- These learning objectives are designed to outline the minimum level of understanding required for each topic.
- The accompanying texts are recommended on the basis that the material contained within them provides sufficient information for trainees to meet the learning objectives.
- Trainees are strongly encouraged to explore the existing and evolving body of knowledge of the Basic Sciences as they apply to Intensive Care Medicine by reading widely.
- For all sections of the syllabus an understanding of normal physiology and physiology at extremes of age, obesity, pregnancy (including foetal) and disease (particularly critical illness) is expected.
- Similarly, for pharmacology, trainees are expected to understand a drug’s pharmacology in these contexts.
- An understanding of potential toxicity and relevant antidotes is also expected.
Definitions
Throughout the document specific wording has been used under the required abilities to indicate the level of knowledge and understanding expected and a glossary of these terms is provided.
Definitions
| Calculate | Work out or estimate using mathematical principles. |
| Classify | Divide into categories; organise, arrange. |
| Compare and contrast | Examine similarities and differences. |
| Define | Give the precise meaning. |
| Describe | Give a detailed account of. |
| Explain | Make plain. |
| Interpret | Explain the meaning or significance. |
| Outline | Provide a summary of the important points. |
| Relate | Show a connection between. |
| Understand | Appreciate the details of; comprehend. |
SAQs
S1: Physiology of Immunology and Host Defence
i. Explain the immunological basis of hypersensitivity including anaphylaxis.
2015A 15
Describe the different types of hypersensitivity reactions including an example of each.
2013A 16
Classify and describe immune hypersensitivity reactions. Give examples for each reaction.
2008B 19
Classify the hypersensitivity reactions, give an example for each reaction and describe the pathophysiological processes of each reaction.
2007B 09
Classify the hypersensitivity reactions. Briefly describe the pathophysiological processes of each reaction. Give an example of each reaction.
CICMWrecks Answer
HYPERSENSITIVITY REACTIONS
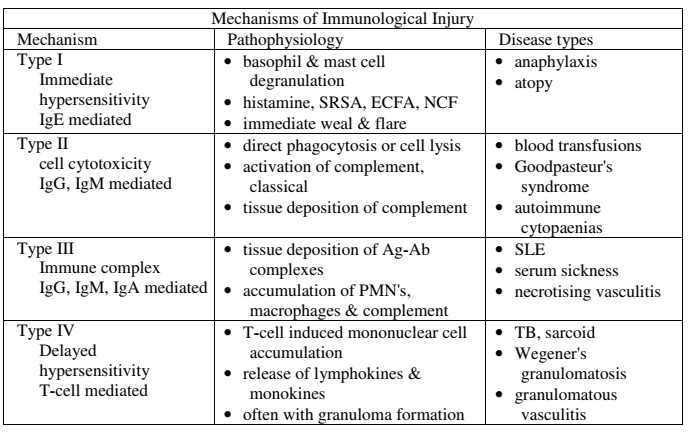
| Type | Pathophysiology | Disease types |
|---|---|---|
| Type I Immediate Hypersensitivity IgE mediated | Sensitisation Plasma B cell production of IgE Mast cell proliferation → IgE binds to mast cells On re-exposure Allergenic antigen binds to mast cell (expressing IgE) → Mast cell degranulates Mast cell degranulation leads to Primary mediators: – Serotonin – Histamine Secondary mediators – Leukotrienes (SRSA) – Prostaglandins – ECFA, NCF | Anaphylaxis Atopy |
| Type II Cell Cytotoxicity IgG, IgM Mediated | Antibody attaches to antigen on target cell Complement release C5-9 “membrane attack complex” → Causes cell lysis | Blood Transfusions Goodpasteur’s syndrome Autoimmune cytopaenias |
| Type III Immune Complex IgG, IgM, IgA mediated | Circulating antibody-antigen complexes are deposited in basement membranes e.g. peritoneum, blood vessels, joints, glumeruli Complement cascade activation Attract granulocytes → inflammation | SLE Serum Sickness Necrotising vasculitis |
| Type IV Delayed hypersensitivity T-cell mediated | T cell mediated Cell mediated, as opposed to previous humoral Peak reaction 2-3 days CD4 helper T cells cause recruitment of Neutrophils Macrophages CD8 cytotoxic T cells | TB, Sarcoid Granulomatosis with polyangiitis (Wegener’s) Granulomatous vasculitis |
SRSA: “slow reacting substance” A – Mixture of Leukotrienes (LTC4, LTD4, LTE4)
ECFA: Eosinophil chemotactic factor of anaphylaxis
NCF: Neutrophil chemotactic factor of anaphylaxis
Key Points:
- “Anaphylaxis” may be:
- True anaphylaxis: a symptoms complex following exposure of a sensitised individual to an antigen, produced by a type I hypersensitivity reaction, associated with IgE mediated mast cell degranulation
- Anaphylactoid reactions: Indistinguishable from true anaphylaxis, however the immune nature of the reaction is either unknown, or not due to a type I hypersensitivity reaction, immediate generalised reaction is a better term.
Gladwin / Mooney 2016
Examiner Comments
2015A 15: 79 % of candidates passed this question.
This question can be answered in tabular form and details have been described in a previous exam report (2007). Details of each of the four main types were expected. A description of the timing of reactions was also expected.
2013A 16:
Overall, this question was well answered. Candidates were expected to classify the hypersensitivity reactions into their typical groups (Type I – IV) and to describe the mechanisms within each group. Similar such questions have been asked in previous exams. Again, those candidates who could provide some structure to their answer tended to score well.
2008B 07: 3 (60%) candidates passed this question
A tabular format is a very desirable format for a response to this question. Again candidates who struggled to provide an organised response also failed to provide sufficient and succinct detail in their answer. A good answer would have included the following features.
Syllabus: M2g
Reference Text: Goodman and Gillman Chp 64
2007B 09: 2 candidates (28%) passed this question
Key Points:
- “Anaphylaxis” may be:
- True anaphylaxis: a symptoms complex following exposure of a sensitised individual to an antigen, produced by a type I hypersensitivity reaction, associated with IgE mediated mast cell degranulation
- Anaphylactoid reactions: Indistinguishable from true anaphylaxis, however the immune nature of the reaction is either unknown, or not due to a type I hypersensitivity reaction, immediate generalised reaction is a better term. i End-organ effects, e.g. H1 and H2 receptors
2016B 09
Describe the immunology and drug treatment of anaphylaxis.
CICMWrecks Answer
Anaphylaxis
- acute severe type I hypersensitivity reaction affecting multiple organ systems
- most common triggers:
- Food, Environmental
- Drugs: antibiotics, muscle relaxants
- Iodine contrast
- Chlorhexidine
- Latex
- Clinical effects
- Circulatory collapse: profound vasoplegia distributive shock
- Airway obstruction: angioedema, bronchospasm,
Pathophysiology
- Multiple exposures to target allergen
- 1st exposure: allergen presented by T helper cells to B cells → B cells produce specific IgE to target allergen
- Circulating IgE attach to mast cells → sensitization
- Subsequent exposure to allergen → allergen binds specific IgE on mast cells → mast cell degranulation → release of allergenic mediators
- Mediators trigger disseminated vasodilation + ↑ vascular permeability +/- bronchospasm → anaphylaxis
- Histamine: Localised release → urticaria; Systemic release → H1 + H2 → vasodilation, ↑vascular permeability → ↓MAP
- Bradykinin: ↑production PGI2, NO → vasodilation, ↑ vascular permeability → ↓MAP
- Prostaglandins: PGID2 → vasodilation, ↑ vascular permeability, bronchoconstriction, chemotactic for neutrophils + activates eosinophils
- Leukotrienes: LTE B4: chemotactic agent; LTE D4 + E4: angioedema, clotting/ thrombolysis/ DIC
- Tryptase: activates complement, coagulation, kallikrein-kinin pathways → ↓ BP, angioedema, clotting/ thrombolysis/ DIC
- TNF-a: cytokine → propagates anaphylactic reaction
- NO: vasodilates
- Serotonin: vasodilation, bronchoconstriction, aplatelet activation
- Platelet activating factor: acts at PAF Rs
Management of Anaphylaxis
- Oxygen
- IV Fluids
- Adrenaline is the drug of choice, as it treats cardiovascular collapse, bronchospasm, and decreases oedema formation.
- Stabilises mast cells to prevent degranulation
- Low doses: Beta agonism at (inotropy and chronotropy) and causing smooth muscle relaxation (including bronchorelaxation).
- Higher doses: alpha effects and causes vasoconstriction.
- In adults, 0.3-0.5mg IM Q5-15min
- In children, 0.01mg/kg IM Q5-15min
- Glucagon may be used in β-blocked patients resistant to adrenaline.
- In adults, 1-5mg IV over 5 minutes, followed by infusion at 5-15microg/min
- In children, 20-30mcg/kg up to 1mg over 5 minutes
Adjunctive agents include antihistamines and steroids. They are second line as they do not attenuate cardiovascular collapse, resolve airway obstruction, or have strong evidence behind their use. They include:
- Steroids:
- Work by binding to the cell nucleus and switching off the transcription of various genes which encode for inflammatory mediators such as cytokines, chemokines, adhesion molecules and arachidonic acid.
- They also activate anti-inflammatory genes such as MAP (mitogen activated protein) and increase the expression of beta2 receptors.
- Methylprednisolone, Hydrocortisone or Prednisolone
- Antihistamines:
- Binds to H1 receptors to block the effects of the histamine released from mast cells-
- inhibition of vasodilatation
- increased vascular permeability
- contraction of non-vascular smooth muscle
- Diphenhydramine 25-50mg IV (Children: 1mg/kg up to 40mg) up to 200mg in 24/24
- Binds to H1 receptors to block the effects of the histamine released from mast cells-
- Salbutamol, for bronchodilation
- Other Non-pharmacological management includes early intubation to protect against airway obstruction due to angioedema
Kerr / JC 2019
Examiner Comments
2016B 09: 32% of candidates passed this question.
It was expected candidates would detail the process of IgE mediated type I hypersensitivity reaction with some discussion of the mediators (Histamine / tryptase and others) and their consequences. Some detail describing time frame of response and the pre-exposure to Antigen (or a similar Antigen) was expected. Drug treatments would include oxygen and fluids as well as more specific agents such as adrenaline and steroids. Adrenaline is the mainstay of therapy and some comment on its haemodynamic role and prevention of ongoing mast cell degranulation was required. Better answers noted steroids take time to work and some also discussed the role of histamine blocking agents.
2013A 17
Compare and contrast the mechanism of action, pharmacokinetics, and side effects of adrenaline, steroids, and antihistamines when used for the treatment of anaphylaxis.
CICMWrecks Answer
| Adrenaline | Steroids | Antihistamines | |
|---|---|---|---|
| An endogenous catecholamine released from the mammalian post-ganglionic sympathetic nerve terminals. | Hydrocortisone and prednisone most common in treating anaphylaxis. Pharmacokinetics of hydrocortisone will be discussed here | Range of sedating and non-sedating agents. Fexofenadine will be discussed here. | |
| PD- MoA | Stabilises mast cells to prevent degranulation Low doses: Beta agonism at (inotropy and chronotropy) and causing smooth muscle relaxation (including bronchorelaxation). Higher doses: alpha effects and causes vasoconstriction. | Work by binding to the cell nucleus and switching off the transcription of various genes which encode for inflammatory mediators such as cytokines, chemokines, adhesion molecules and arachidonic acid. They also activate anti-inflammatory genes such as MAP (mitogen activated protein) and increase the expression of beta2 receptors. | Binds to H1 receptors to block the effects of the histamine released from mast cells- namely, inhibition of vasodilatation, increased vascular permeability, and contraction of non-vascular smooth muscle |
| SE | HTN, tachycardia and arrhythmias, Metabolic (glycogenolysis, lipolysis, gluconeogenesis) and can increase BMR. Can worsen PHTN(causes pulm vasoconstriction) and glaucoma. | Single dose– minimal side effects. Repeated dosing– multiple effects on virtually every organ system. CVS– HTN. CNS– psychosis, mood disorders. GIT– gastriculcers, pancreatitis. Haem– leukocytosis. ID– increased risk of infection. MSK– osteoporosis, weakening of proximal muscles, abdominal striae, easy bruising, thin skin | May cause headache or drowsiness |
| PK A | Route- IV, IM, S/C, NEB, ETT Dose- 1mg ALS, 0.1mg anaphylaxis, titrated dose for haemodynamic instability (Start at 0.01mcg/kg/min, for alpha effects) Onset to action- seconds, duration 2 mins | Route – PO, IV, inh, neb Dose– usually 200 mg IV for anaphylaxis. May require repeat dosing. | Route – PO, BA 33% Dose – 60-240mg daily in divided doses |
| D | Does not cross the BBB 50% protein bound | 90% protein bound at low concentrations, only 60-70% bound at higher. Vd 0.3-0.5L/kg | Protein binding 70% |
| M | Taken up by the sympathetic nerve terminals and metabolised via COMT and MAO circulating Adr metabolised via COMT | Hepatic to tetrahydrocortisone | Negligible metabolism in humans. |
| E | Via urine as inactive metabolites (half-life 2 min) | Elimination half-life 1.2-1.8hrs | Terminal half-life 14-15hours |
JC 2019
Examiner Comments
2013A 17:
This question asked candidates to compare and contrast the mechanism of action, pharmacokinetics, and side effects of these drugs in the context of the treatment of anaphylaxis. Information beyond that did not score marks. A structured approach (e.g. a table) assisted in presenting the information.
ii. Describe the factors involved in the process of inflammation and the immune response, including innate and acquired immunity.
2010B 09
Describe how the body defends against infection.
CICMWrecks Answer
Immune System: complex network of cells and proteins that defends the body against infection.
Physical barriers
- Skin
- Cilia
- Respiratory tract
- Acidic environment
- Stomach
Innate immunity
Recognize generic pathogenic motifs and directly attack or opsonize and phagocytose
- Defensins – perforate pathogenic membranes
- Compliment cascade – opsonize and signal for phagocytosis and directly lyse via membrane attack complex
- Innate immune cells
- Neutrophils
- Degranulate cytotoxic contents and cause oxidative damage to pathogens
- Macrophages
- Phagocytose and kill opsonized pathogens
- Dendritic cells
- Phagocytose and present antigen to cells of acquired immune system
- Natural Killer cells
- Recognize abnormal cell surface expression (e.g. lack of MHC, abnormal MHC proteins) due to intracellular pathogens (e.g. virus) and directly kill infected cells
- Neutrophils
Acquired immunity
- Pathogenic antigens presented to B cells and T cells via APCs such as dendritic cells
- Show: Specificity, Memory, Diversity, Immunological tolerance
- B cells (20%, Humoral Immune reponse)
- Produce antibody against antigen
- Antibodies opsonize and target for T cell killing, phagocytosis and compliment cascade
- B cells become memory B cells and plasma cells, primed for explosive antibody production on subsequent exposure to the same antigen
- T cells (80%, Cell-mediated immune reponse)
- Major subtypes into CD8 (Killer) T cells and CD4 (Helper) T cells
- CD8 (Cytotoxic/Killer) T cells recognize specific antigen presented to them via TCR and lyse pathogens and infected cells
- CD4 T (Helper) cells produce cytokines for adjacent B cells that recognize the same antigen, allowing B cell differenciation and antibody production
- CD28 (Regulatory) T cells dampen the immune reaction, preventing or limiting autoimmune damage.
- Memory T Cell: Reside in lymphoid tissue and induces more rapid and powerful immune response with 2nd exposure to Ag
Sakurai 2016
Examiner Comments
2010B 09: 8 (53%) of candidates passed this question.
For a good answer candidates were expected to describe physical barriers, innate and acquired immunity. Physical barriers such as skin, mucous membranes, normal flora, secretions, etc were poorly covered. Aspects of immunity such as cellular and humoral were better covered but often lacked a sufficient depth of knowledge.
Syllabus: M2a References: Guyton and Hall Textbook of Medical Physiology, Chp 33 and 34
2012A 07
Compare and contrast the characteristics of B and T lymphocytes.
CICMWrecks Answer
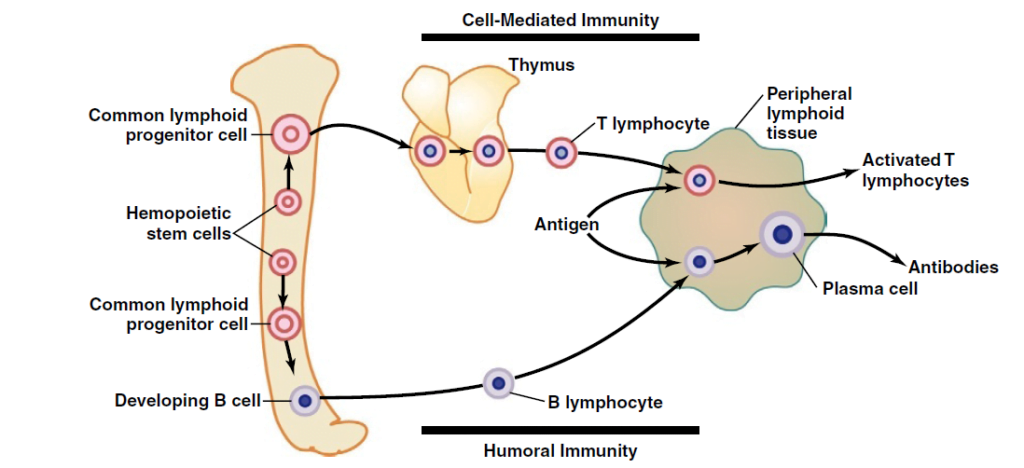
Lymphocytes are responsible for acquired immunity
Antigens on foreign material stimulate proliferation and immune response
- In T and B cells, there a millions of different clones which express different antigen binding site
- Each lymphocyte clone is highly specific for a particular antigen, and can only be activated by it
| T cell | B cell | |
|---|---|---|
| Cell mediated Immunity | Humoral Immunity | |
| Origin | Haemopoeitic stem cells in bone marrow → common lymphoid progenitor cell | Haemopoeitic stem cells in bone marrow → common lymphoid progenitor cell |
| Site of differentiation | Thymus | Liver in mid-foetal Bone marrow in late-foetal and after birth |
| Site of storage | Lymph (thymus, spleen, submucosa of GIT, bone marrow, lymph glands) | Lymph (thymus, spleen, submucosa of GIT, bone marrow, lymph glands) |
| Receptor | T cell receptor Only respond to antigens bound to antigen-presenting cell (macrophage) | B Cell receptor (Immunoglobulin molecules) Can bind to antigens directly |
| Mechanism of activation | Antigen binds to major histocompatability complex on 1) macrophages 2) B-lymphocytes 3) dendritic cells Antigen bound to MHC is sensed by surface receptor | Activated following T-cell activation |
| Type of immunity | Cell-mediated Cytotoxic T cells bind to pathogen (via antigen) → Release perforins → Punch holes in cell membrane → Also release cytotoxics into these holes | Humoral Antibody can cause: Precipitation Lysis Agglutination Neutralisation Antibody-antigen complex activates complement cascade → pathogen damage → recruitment of phagocytes and local inflammation |
| Derived cells | Helper T cells Encourage proliferation of cytotoxic and suppressor T cells Stimulate B-cell proliferation Attract and activate macrophages Cytotoxic T cells Suppressor T cells Suppress both cytotoxic and helper T cells Memory T cells Circulate until reactivation | Plasma cells Produce IgG antibodies and release them into lymph → blood Memory B cells Propogate and circulate to all lymph tissue, ready for reactivation |
| Function | produce antibodies that can bind to and neutralize extracellular pathogens or toxins | recognize and eliminate intracellular pathogens, such as viruses, or help other immune cells to do so |
| Lifespan of memory cells | Many years | 6-12 months (as B memory cells can reactivate them) |
Mooney 2016
Examiner Comments
2012A 07: 4 (40%) of candidates passed.
A structured response was required for this question. Candidates were expected to mention the origin of the cells, sites of differentiation (foetal liver, lymph nodes, bone marrow in early childhood for T lymphocytes and thymus for B lymphocytes), antigen receptors and what they bind with (highly specific IgM surface antibodies that bind with extracellualr antigens for T lymphocytes and surface receptors that bind to antigen presenting cells for B lymphocytes), type of activation cell, type of immunity (humoral for T lymphocytes, cell mediated for B lymphocytes), their functions and life span (T lymphocytes much shorter than B lymphocytes. Although some candidates found this question challenging, of those who passed it, most achieved a high score.
2023B 15
Describe the components and function of the complement system including the role, activation and control?
CICMWrecks Answer
Definition
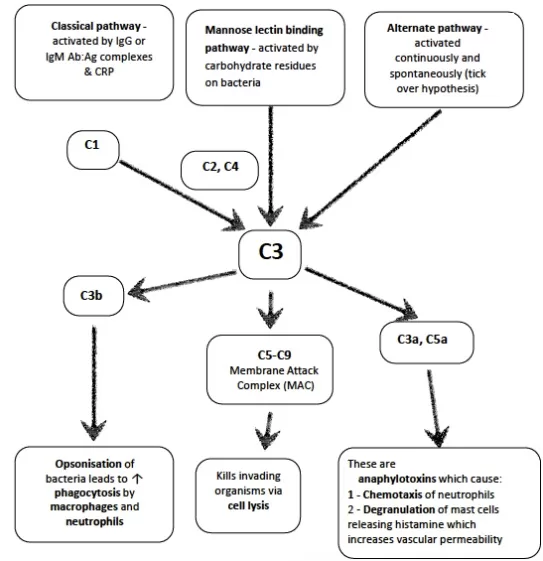
- Proteolytic enzyme amplification cascade system; forms part of innate + acquired immune response
- Components circulate as inactive precursors
- Activation amplifies as a cascade; regulated by regulator proteins e.g. C1 esterase inhibitor
- Proteins produced by liver
- 9 complements: C1(q, r, s), C2, C3, C4, C5, C6, C7, C8, and C9
- Also B, D, H, I and properdin
Main functions
- cell lysis of bacteria (MAC)
- opsonisation → ↑phagocytosis
- release of mediators via mast cell degranulation
- local vasodilation
- neutrophil aggregation
- chemotaxis
Components (7 functional)
| Group | Factor | Function |
|---|---|---|
| Initiators | C1q, MBL | Initiators |
| Enzymatic mediators and convertase activator | C1r, C1s, MASP2, and Factor-B | proteolytic enzymes that activate other members |
| C3 convertase C5 convertase | enzymatic mediators | |
| Membrane binding components or opsonins | larger fragments such as in C3, C3b | enhances phagocytosis |
| Inflammatory mediators | Smaller fragments like in C3, C3a | Inflammatory mediators |
| Membrane attack protein | Membrane attack complex (MAC) comprises C5b, C6, C7, C8, C9 | protein of MAC inserts and creates a hole on cell memrane so cell lysis occurs |
| Complement receptor protein | CR1 | binds to complement protein and signal-specific cell function |
| Regulatory complement components | Factor I Protectin | proteins that protect the host cell against the action of complement |
Pathways
- Classical – activation by Ag-Ab complex
- system of 11 enzymes
- pathway activated by formation of Ag-ab complexes, CRP, aggregated Ig (IgM or certain IgG)
- activates C1 → reactions involving C4+C2 → formation of enzymatic complex C4b-C2a → cleaves C3a and C3b → common pathway
- Alternate – activation by lipopolysaccharides
- C3 undergoes slow, spontaneous conversion to hydrolysed C3
- Multiple steps leading to complex ith C5 convertase → activation of common pathway
- Nil ab required
- Lectin – activation by mannose on surface of parasites, candida, viruses etc
Mechanism
following activation → triggers final common pathway → C3 activation → C3b acts as C5 convertase → C5b binds C6-C9 → forms membrane attack complex → inserted into target cell membrane → leakage of cellular material → cell lysis + destruction
Regulation
- Half of all complement proteins serve regulatory function
- goal
- to prevent complement damage to normal host tissue (inappropriate / wrong target)
- fluid-phase activation (no target)
- deficiencies lead to excessive complement activation
- Regulatory proteins inhibit system by destabilizing activation complexes and mediating specific proteolysis of actication-derived fragments
- Complement pathways are regulated at the following critical steps
- Activation (initiation) – C1 inhibitor (C1inh) in classic and lectin pathways
- Amplification (convertase formation) – e.g. binding proteins to C3 convertases
- Membrane attack (lysis) – S-protein prevents insertion of Membrane attack complex (MAC) into membrane, CD 59 (protectin) bind C8 and C9 inhibiting final steps of Membrane attack complex
- Anaphylactoids – carboxypeptidases inactivate C3a,C4a,C5a
Sources: Kerr’s notes, biosciencenotes.com
Examiner Comments
2023B 15: 8% of candidates passed this question.
Based on the question stem answers should have been structured to address the components of the complement system as well as the role, activation and regulatory mechanisms. A description of the components should include the number and type of molecule highlighting the important combinations of complement to produce the membrane attack complex. A description regarding the role in the innate immune response against bacterial infections was then required with a detailed description regarding the many ways this is achieved including opsonisation, phagocytosis, chemotaxis, mast cell/basophil activiation, lysis of cells and clearance of immune complexes. Information about the 3 pathways of activation where expected; classic, alternate and lectin pathyway, with some detail regarding the downstream effect of each that would take into account for the amplication of the response. The cessation of complement response is largely due to the limitatations of the half lives of the particular complement glycol-proteins or presence of specific inactivators.
2011A 20
Describe how previous immunisation protects against subsequent infection.
CICMWrecks Answer
Definitions
Immune System: complex network of cells and proteins that defends the body against infection. They can be classified as:
- Physical barries
- Innate Immunity: Recognize generic pathogenic motifs and directly attack or opsonize and phagocytose
- Acquired immunity: Pathogenic antigens presented to B cells and T cells via APCs such as dendritic cells
Immunization: A process by which a person becomes protected against a disease through vaccination. This term is often used interchangeably with vaccination or inoculation.
Vaccine: A product that stimulates a person’s immune system to produce immunity to a specific disease, protecting the person from that disease.
Immunization:
- Passive
- Active
- Passive Immunization:
- transfer of preformed antibodies to an unimmunized individual.
- develop temporary immunity to the particular organism or toxin
- Once these preformed antibodies have been destroyed, the individual would no longer have immunity to this microorganism or toxin.
- e.g: Natural: passage of maternal antibodies through the placenta to the fetus
- e.g: Artificial: administration of pooled human immune gamma globulin and antivenin
- Active immunization:
- occurs with the exposure of an unimmunized individual to a pathogenic agent
- Immune system begins the process of developing immunity to this agent
- produces long-term immunity due to the stimulation of the individual’s immune system.
Stimulation of Immunity by vaccines:
Detection:
- by innate immune system, and/or B-cells
- recognize epitopes on antigens
Primary Response to vaccine administration:
- Innate Immune System activation:
- Opsonize or bind to agent → aid in engulfment by Antigen-presenting cells (macrophages or monocytes) → insert processed antigen + MHC protein onto its surface
- Complex presented to Adaptive Immune System:
- Viral: Antigen + MHC I complex → presented to CD8 cell → trigger cell mediated immunity
- Bacterial or parasitic: Antigen + MHC II protein → presented to CD4 cell → trigger antibody- mediated immunity
- Memory T-cells and B-cells formed → undergo clonal selection following infection, which increases antigen-binding affinity
Subsequent Infection: 2° immune response
- Subsequent exposure to Ag
- memory T cells rapidly proliferate into active helper and cytotoxic T cells specific to that antigen
- memory B cells rapidly produce antibodies to neutralize the pathogen.
- more rapid, prolonged and powerful immune response
Types of vaccines:
- Live attenuated vaccines: produce a strong cellular and antibody responses and typically produce long-term immunity with only one to two doses: MMR, Typhoid
- Inactivated vaccines: Influenza
- Toxoid: Tetanus, diphteria
- Subunit vaccines: Hepatitis B
- Conjugate vaccine: Haemophilus Influenza B vaccine
- Outer membrane vesicle vaccine: B-Meningococcal
- Heterotypic/Heterologous: BCG
- Viral vector: Ebola
- RNA: Pfizer–BioNTech COVID-19 vaccine
JC 2020
Examiner Comments
2011A 20: 1 (8%) of candidates passed this question.
Providing a statement about what vaccines do followed by some detail about the processes involved in triggering a response and the nature of that response in both Innate immunity and acquired immunity would have achieved a good pass. Many candidates failed to adequately describe the nature of the primary and the secondary response to antigen exposure. The fact that previous immunisation enabled a brisk secondary response was recognised by most candidates but that this was largely due to the proliferation of IgG antibody producing B lymphocytes and effector T cells was not appreciated. Many answers simply did not include sufficient information to achieve a pass mark.
Syllabus: M2i
Recommended sources: Review of Medical Physiology, Ganong, Chp 3
iii. Outline the non-immune host defences used to defend against infection.
S2: Pharmacology Related to Immunology
i. Understand the pharmacology of Human Immunoglobulin.
VIVAs
| 2023B | |
| 2023A | |
| 2022B | |
| 2022A | IgE mediated anaphylaxis innate immunity |
| 2021B | |
| 2021A | |
| 2020B | |
| 2019B | |
| 2019A | |
| 2018B | |
| 2018A | |
| 2017B | immunology and associated pharmacology. Innate immunity |
| 2017A | |
| 2016B | |
| 2016A | |
| 2015B | |
| 2015A | |
| 2014B | |
| 2014A | |
| 2013B | Hypersensitivity reactions, histamine, H receptors, adrenaline |
| 2013A | |
| 2012B | |
| 2012A | |
| 2011B | Acute inflammatory response to tissue injury – cytokines, component, apoptosis, immune basis of rejection of allogenic organs, serotonin |
| 2011A | |
| 2010B | |
| 2010A | |
| 2009B | Allergic reactions, tratment, common agents in ICU |
| 2009A | Outline the body’s defence mechanisms against infection |
| 2008B | |
| 2008A | |
| 2007B |

Recent Comments